Woundhealingsa.co.za
Case Study : The WHASA Wheel THE WHASA WHEEL – Integrating multiplespecialities in patient management with wound healing
as the common basis
Widgerow AD, MBBCh, MMed(Surg), FCS(Plast), FACS
Private plastic surgeon, Linksfield Hospital, Johannesburg Correspondence to: Prof Alan Widgerow, e-mail: [email protected]
Introduction
There is not a speciality in Medicine that I can think of today where Wound Healing does not impact. The surgical specialities by their very
nature involve the healing of wounds in one form or another, but it is not always appreciated that almost every chronic medical condition
also has associated wound problems. This reality results in an unprecedented amalgamation of medical minds and basic scientists all
contributing to a surge in knowledge related to this relatively new field.
The WHASA (Wound Healing Association of Southern Africa) WHEEL is a concept that has been developed to demonstrate the impact of interspeciality co-operation for the ultimate benefit of the patient. This article, by means of a hypothetical case, attempts to demonstrate this co-operation and to highlight esoteric situations that arise when considering wound healing among the different fields. It is by no means exhaustive of surgical scenarios but merely representative of fairly common situations that any of us could encounter on a daily basis.
The article takes the form of a case report which is interspersed with ‘wound healing' discussions that I have added under the heading ‘WHASA background comments'. In addition invited comments from our esteemed col eagues that make up the components of the WHASA WHEEL are included within the text.
Wound Healing Southern Africa 2008;1(1):07-14
Case report
bleeding, debridement of the necrotic mesentery, fascia, A 57 year old male patient was seen in Trauma Casualty following peritoneum and muscle and a motor vehicle accident. Initial examination revealed polytrauma thorough washout of the including a head injury, blunt abdominal trauma and a compound abdomen, total closure of fracture of the left tibia. His medical history included that of a type 2 the abdominal wall was not diabetic on oral medication in an otherwise healthy male. possible and the abdomen The patient responded to pain and withdrew in response to pain with was packed and closed incomprehensible verbal responses. He was assessed as a 10/15 with a broad polyurethane Glasgow Coma Scale score head injury but pupils were equal and temporary ‘sandwich' dressing responsive to light. Examination of the abdomen revealed ecchymotic with the intention of returning areas with an underlying tense distended abdomen. Palpation the patient to theatre in 72 hours once compartment confirmed fullness of the abdomen with percussion tenderness. A pressure had reduced and diagnostic peritoneal lavage showed the presence of more 200 000 the patient considered stable RBC/mm3 constituting a positive result for an intra-abdominal bleed. for further surgery. Examination of the left leg revealed an obvious compound fracture Figure 1: Tibial plateau fracture with severed of the upper third of the tibia and a weak pulse in the posterior tibial Comments from WHASA
artery region of the left lower limb. The ankle-brachial pressure index Wheel partner – Trauma
was assessed to be 0.6. Sensation to the foot was intact. surgeon: Prof Ken Boffard
Fol owing initial resuscitation and external reduction and splinting This patient's blood pressure is not recorded. If the patient is stable, of the tibial fracture, the patient was transferred to the operating he would probably get a CT scan of his head, abdomen, and a CT theatre under the care of the trauma surgeon, orthopaedic surgeon angiogram of his leg. If unstable, either the DPL or a FAST ultrasound and a vascular surgeon. A straight X-ray and on-table single-shot would be appropriate. The priorities would be to minimise secondary femoral angiogram revealed a tibial plateau fracture and a suspected brain damage through hypotension, and if there are signs of shock, transected popliteal artery with associated thrombosis (Figure 1). the abdomen takes priority.
Exploration of the abdomen revealed injury to the smal bowel The leg has a tibial fracture, in its upper third. This is generally below the trifurcation, and sensation is intact. This implies that since there mesentery with significant bleeding and pressure necrosis of the are three vessels at this point, and the mechanism of injury is not peritoneal fascia and abdominal wal muscle. Fol owing control of the Wound Healing Southern Africa 2008 Volume 1 No 1



Case Study : The WHASA Wheel
compatible with transection of al three, that the most likely cause of the pulseless leg is positional, possibly with compartment syndrome. In the emergency department the fracture should be reduced and back-slabbed, or traction applied.
The X-ray (Figure 1) shows an upper tibial fracture, with popliteal transection, but reasonable col aterals. In this patient, on-table angiography is appropriate in the absence of CT angio.
There is injury to smal bowel mesentery, bleeding and necrosis of fascia and abdominal wal muscle. (Presumably due to a crush injury). There is no mention of the general condition of the patient, specifical y lactic acidosis. However, this patient fits the criteria for damage control, which implies haemostasis and any contamination control. This patient should have any mesenteric and other bleeders tied off, and then the operation should be terminated. No attempt should be made, in the presence of other injuries, to resect dead muscle. The abdomen should be thoroughly washed out. Any oozing should be judiciously packed.
NO attempt should be made to close the abdomen at this stage, and specifically the fascia should not be primarily repaired, grafted, or sutured. This case is ideal for an "Opsite Sandwich negative pressure dressing." Use of the proprietary VAC dressing at this stage is not indicated due to the risk of abdominal compartment syndrome. Equally, now is not the time to waste time on the abdomen.
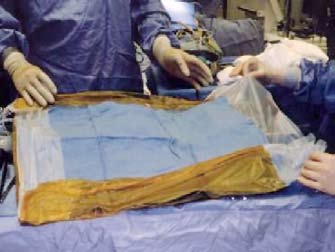
Figure 2B: Opsite Sandwich dressing technique. The skin is dried and shaved –
pubic hair shaved as necessary. A surgical drape is placed on Opsite, Steridrape,
or Ioban, covering one side only
Figure 2A: Temporary Opsite® negative pressure sandwich dressing
The sheet is placed on the intestines and spread between the gut and abdominal wall laterally with the plastic in contact with the bowel.
This allows the bowel to bulge out if pressures are high (Figure 3).
Figure 3: Bowel bulging under ‘sandwich dressing'
Two large suction drains are secured to the outside of the covered
compartment fasciotomy through bilateral open incisions was done.
surgical drape to control fluids. A large Ioban® or Opsite® is placed
Fol owing debridement and soft tissue closure, an external fixator
from the nipples to the groins.
was applied to reduce and align the fractured tibia. Negative pressure VAC dressing was then applied to the open wound anteriorly (See
Case report continued
Figure 4). Thus the vascular repair was isolated to an area apart from
Thus the abdominal injury was addressed by the trauma surgeon.
open wound and negative pressure dressing.
Simultaneously the vascular surgeon repaired the injured popliteal artery by a femoro-popliteal bypass using autologous saphenous vein
WHASA background comments
harvested from the contra-lateral limb. Complete heparinisation was
This case report highlights an interesting dilemma – negative
not used due to the increased risk of haemorrhagic complications
pressure therapy and anti-coagulation. Complications of bleeding in
intra- and post-operatively. The patient was put on low molecular
patients on oral anti-coagulants have been reported particularly in
weight heparin on the day after surgery.
infected leg ulcers.7 Most articles in fact would list anti-coagulation
In order to preserve the closure and reduce compartment tension
as a relative contra-indication to negative pressure therapy. Logic
in the leg and in the area of the repaired artery, it was elected
dictates that preference should be given to ensuring successful
not to close the anterior wound on the leg – in addition a ful four
outcome of the vascular repair – an alternative wound dressing
Wound Healing Southern Africa
2008 Volume 1 No 1
Case Study : The WHASA Wheel
to repair the arterial supply to the distal extremity. Exposure of the distal superficial femoral artery and the second part of the popliteal artery would be required. Autologous saphenous vein is the conduit of choice in bypass surgery distal to the knee joint. The use of the saphenous vein from the contra-lateral limb reduces the risk of venous insufficiency of the ipsilateral limb, especially in the setting of a concomitant venous injury (popliteal vein).
In an effort to conserve time and reduce ischaemia, the vascular surgeon could opt for the use of a temporary vascular shunt between the proximal and distal arteries. This would al ow time for the orthopedic surgeon to complete either internal or external fixation of the fracture. While this is being done, the vascular surgeon could harvest and prepare the saphenous vein from the controlateral limb. The bypass can then be performed on a stabilised limb. In extreme cases (damage control), the shunt could remain in position until the
Figure 4: Negative pressure dressing leg
patient has been adequately resuscitated.
(anything from simple hydrogel to foam cavity dressing) could
There should be a low threshold to perform four compartment lower
easily have been chosen if bleeding was deemed to be a real risk.
limb fasciotomies through medial and lateral incisions in this patient,
Fortunately most surgeons now do not routinely use systemic
due to the patient's increased risk of developing compartment
heparinisation fol owing vascular repair, so the negative pressure
syndrome of his left leg. Post-operative wound care within this
dressing should not be too much of a problem.
setting is of great importance. Various types of dressing, including negative pressure dressings, could be considered. A debridement
The timing of arterial repair and exposure of the site are also
of the fasciotomies is required within 24 to 48 hours. As soon as
important. Obviously one would like to carry out the arterial repair
the fasciotomy wounds can be closed, either primary closure of the
as rapidly as possible to diminish ischaemic time, but one has to
wound or skin grafting can be utilised.
consider the amount of manipulation and soft tissue exposure that the orthopaedic surgeon would need to fix the fracture. The surgeons
Due to the fact that fasciotomies compromise the normal muscle
would work together on that decision making process, and external
pump function of the lower extremities, the limb should be elevated
fixation of the fracture considerably simplifies the problem.
in the post-operative period. As soon as the wounds al ow, low grade graduated compression bandages and eventual y compression
For both procedures the avoidance of sepsis is paramount to success
hosiery can be applied to prevent venous insufficiency.
– thus the dressing chosen would be aimed at promoting granulation tissue and preparing the wound bed for closure (likely skin graft) as
Comments WHASA Wheel partner –
soon as possible. In this case this would coincide with the secondary
Orthopaedic surgeon: Dr Chris McCready
abdominal closure envisaged within the following week. Ideally
The patient, in this case study, has suffered severe trauma, with
discussion and planning between surgeons, and possibly the wound
multiple injuries. The main role of the orthopaedic surgeon in
therapist involved with the negative pressure dressing, should take
this case is damage control, regarding the left leg injury. He has
place so that the needs of the patient can be orchestrated.
sustained a Gustil o-Anderson type I Ic injury to the left tibia. The
Comments WHASA Wheel partner –
critical issue that needs to be addressed is the injury to the popliteal
Vascular surgeon: Dr Gregory Weir
artery. The ischaemic time plays a role in deciding if the artery should be repaired first, or if the fracture should be stabilised first.
Most published articles on the topic of vascular injury stress the
If the fracture is stabilised, the arterial repair is easier, however,
importance of reducing the ischaemic time. This wil reduce the
the viability of the limb should not be compromised. Another, more
morbidity and risk of amputation in these patients. In this specific
commonly used means of fixation is that of an external fixator. This
case, the absent/diminished pedal pulses and reduced ankle-
is quickly applied, gives stable fixation, and can be converted to rigid
brachial pressure index, could have been due to a displaced fracture,
internal fixation once the patient is more stable.
which might have caused pressure on the artery. The presence of a thrombosed vessel on the arteriogram confirmed an arterial injury
Another consideration, is the open wound. There is a 42% incidence
requiring urgent intervention.
of sepsis with these fractures. A complete surgical debridement should be performed, preferably within 6 hrs of the injury. Due to the
Life threatening injuries always require higher priority than limb-
high energy transfer involved, the extent of the soft tissue injury is
threatening injuries. The trauma surgeon and vascular surgeon would
difficult to evaluate. Therefore, it is preferable to leave these wounds
probably have explored the abdomen as a team. Only after the life-
open, and should the patients condition al ow, perform a second
threatening injury had been control ed, would the limb-threatening
debridement in 72 hrs to remove any remaining necrotic tissue. With
injury be addressed.
exposed bone, or metalwork, an occlusive dressing is preferred. A
Due to the fact that the patient was in a supine position for the
negative pressure dressing wil assist in stimulating granulation
explorative laparotomy, direct access to the popliteal artery behind
tissue, which wil provide an excel ent bed for a split skin graft at
the knee joint (usually done through a posterior incision), would have
been impractical. A short femoro-popliteal bypass could be used
Wound Healing Southern Africa
2008 Volume 1 No 1

Case Study : The WHASA Wheel
Comments from WHASA Wheel partner –
Basic principles involved are the following:
Trauma surgeon: Prof Ken Boffard
1. Creating and preserving the peritoneal space between the
Vascular surgeon is correct and timing is appropriate. Orthopaedic
abdominal viscera and the abdominal wal preventing adhesions
repair should, NEVER in this case be internal fixation, as there would
and fistulae.
be too much additional disruption of the blood supply and muscle
2. The space is usual y created with either a temporary prosthetic
attachments. This case should be external y fixed as described. The
sheet for early closure, absorbable meshes of varying types or
vascular repair takes priority over the orthopaedic fixation, but if
a non-absorbable bioprosthetic material that is non adherent to
necessary, a shunt can be used. External fixation is very rapid (10
underlying bowel where it is felt that fascial advancement and
closure wil not occur. Progressive closure of the peritoneal fascia
It is mandatory in this case to do a ful four compartment fasciotomy
should be attempted in all cases.
through bilateral open incisions which are of adequate length. Almost
3. Wherever possible early closure (within approximately 9 days of
certainly, the medial one wil be in continuity with the vascular
the initial procedure) should be attempted to encourage success
incision. In this case, since there is a col ateral blood supply, it is
and prevent adhesions of abdominal wall and mesh.
reasonable to do the vascular repair first. However, in the absence of pulses with absence of sensation, the fasciotomies should be done
4. Negative pressure dressings are used in al the above scenarios
before the repair. The popliteal vein should be checked since it is
as this wound therapy has lead to the egression of bowel oedema,
often damaged as wel . It is critical therefore to preserve the great
slow advancement of the fascial edges and early closure of the
saphenous vein, as this may be the only viable venous return, and
open abdomen.
if vein grafting is required, the vein should be harvested from the
Various prostheses are available
opposite leg.
for temporary abdominal closure,
The use of the VAC on the open fasciotomies is fine, but may be
including polytetrafluoroethylene
ineffective in the presence of an external fixator.
patch, polypropylene mesh, and polyglactin mesh. They al ow for
I don't believe anticoagulation is an issue here. One does not routinely
sequential closure when possible,
anticoagulate a vascular repair (especial y with the mesenteric
provide protection to the underlying
ooze, etc). Additional y, we would routinely put this patient on low
bowel as well as a method for
molecular weight heparin on the day after surgery.
fluid egress, and it al ows for
Case report continued
easy abdominal re-entry when necessary.1-4
The patient was returned to theatre at 72 hours fol owing the
The prostheses and negative
initial procedure. Abdominal compartment pressure had decreased
pressure dressing also address
considerably but not sufficiently for full abdominal closure. It was
the problems of fascial retraction
uncertain whether sufficient tissue would be available for full
and adherence of the viscera to
fascial/muscular closure. As a further interim measure VAC negative
the overlying abdominal wall,
Figure 5: VAC Dressing to the abdomen
pressure dressing was applied (Figure 5). The plan was to return the
al owing for continuing attempts at
patient to theatre in a further 72 hours – if tissue was deficient for
abdominal closure several weeks
closure additional materials such as vicryl mesh or acel ular dermis
after laparotomy.
would be considered for interposition closure.
Temporary abdominal wal closure
WHASA background comments
techniques in the past have been
Negative pressure therapy is intended to create an environment that
associated with enterocutaneous
promotes wound healing by secondary intention by preparing the
fistula produced by erosion of
wound bed for closure, reducing oedema, promoting granulation
the bowel by overlying dressings.
tissue formation and perfusion, and by removing exudate and
The major barrier has been lack
infectious materials. The concept of leaving the abdomen open
of a prosthetic material that can
intentional y after laparotomy is an accepted method of management
be put directly on bowel without
in certain circumstances (such as decompressive laparotomy as
eroding and can be inserted into a
depicted above). One needs to protect the viscera and al ow for
contaminated field. Authors have
Figure 6: Skin grafting directly on
a simple return to the abdomen at the time of reoperation. In the
reported success with aggressive
past simple skin grafting of the open area was undertaken with the
early closure of the open abdomen
resultant herniation needing secondary repair later (Figure 6).
using a nonabsorbable biological prosthesis made up of with human acellular dermal matrix (Alloderm,
Utilising negative pressure dressings, current data demonstrate
Lifecell Corporation, Branchburg, NJ).1
a fascial closure rate of 88%,1 with almost half of these closures
In these authors experience most of even the largest defects can
occurring at 9 to 21 days after initial operation. Thus the technique
easily be closed with just a few sheets because the dermal matrix
al ows for the large majority of abdomens to be closed with fewer
expands up to 40% of its original size once well hydrated. Successful
hernia repairs required. In addition, the technique allows for
incorporation of tissue into this prosthesis has been demonstrated.1
successful closure at a significant interval after laparotomy.
Wound Healing Southern Africa
2008 Volume 1 No 1



Case Study : The WHASA Wheel
Comments from WHASA Wheel partner –
Trauma surgeon: Prof Ken Boffard
With regard to the WHASA principles elaborated above:
I. I absolutely agree. The ideal is that the plastic is in contact with
bowel, while the swab or drape is in contact with the anterior abdominal wall. This stops it sliding about.
2 & 3. Most times, early closure is critical to avoid sepsis, so I would
suggest that 72 hours is optimum.
4. I absolutely agree with VAC as a secondary closure. It should
not be used initially, since it can exacerbate an Abdominal
Figure 8: Grade 2 heel pressure sore
Figure 9: Desquamating areas on the
Compartment Syndrome due to its rigidity under vacuum.
back – Stevens Johnson Syndrome
Case report continued
Successful resolution of this difficult condition transpired fol owing a treatment regimen that included: oral carbamazepine for epilepsy
Seven days later the patient was returned to theatre, the abdomen
control, intravenous methylprednisolone initially and decreasing
was successful y closed and the left leg wound was skin grafted. The
doses over the following 2 weeks, and oral pheniramine maleate.
patient was returned to ICU for ongoing monitoring.
Topical wound care with hydrocortisone acetate cream and
On the eighth day nurses observed an area of redness and inflammation
polyurethane sheet dressings.
in the sacral region and on the undersurface of the right heel. The
Comments WHASA Wheel partner –
sacral pressure sore progressed rapidly to significant skin breakdown.
Wound healing specialist: Prof Magda Mulder
Simultaneously the patient developed a rash on his back.
The symptomatic treatment in these patients are almost the same
The sacral pressure sore was diagnosed as a Grade 4 pressure
as for burns.
sore (full thickness damage involving underlying muscle ) (Figure 7).
The nursing objectives are to:
Hydrocol oid dressings were initial y used then hydrogel dressings were introduced to stimulate granulation tissue in preparation
• Maintain fluid and electrolyte balance
for surgery.
• Prevent wound infection and sepsis• Promote wound healing
Fortunately the heel pressure was diagnosed as Stage 2 (damage to
• Control environmental temperature (30 – 32ºC reduces caloric
the epidermis and part of the dermis presenting as a blister) (Figure
loss through the skin)
8). The heel blister was evacuated, hydrocol oid dressings applied
• Give psychosocial support
and a pressure relieving system was utilised. Due to the patient's background diabetic condition, the resident podiatrist was consulted
Because skin and mucosa are the body's first line of defence,
to manage the patients feet and to educate him on long term care
infection is almost an unavoidable consequence. Scrupulous aseptic
of his feet.
technique is essential when any procedure is carried out on the patient. Prophylactic systemic antibiotics are not recommended.
Several approaches in wound management are used:
• Extensive debridement of nonviable epidermis fol owed by
immediate cover with biological dressings or non-adherent dressings that can either absorb excess exudate, add moisture to a dry wound bed or retain moisture to ensure moist wound healing.
• Leaving the involved epidermis that has not yet peeled off in
place and cover it with dressings only to protect and absorb and using biological dressings on raw dermis.
Comments WHASA Wheel partner –
Figure 7: Sacral pressure ulcer
Dermatology specialist: Dr Gary Levy
The rash that presented on the patients back was initially a mystery.
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis
The rash then progressed rapidly to involve the patient's eyelids
(TEN) are severe life-threatening forms of skin disease. In about half
and lips. The rash consisted of atypical blistered targets and
the cases the cause is not known while in 50 % of cases the use
erythematous macules encompassing bullous lesions of irregular
of a drug can usually be identified. The more severe the reaction,
size and shape dispersed over his body progressing to desquamating
the more likely that it was drug-induced. Anticonvulsants, non-
skin lesions (Figure 9). The dermatologist consulted carried out a
steroidal anti-inflammatories and antibiotics especially penicillin and
detailed analysis and discovered that following on the head injury the
sulpha drugs are the most commonly reported drugs, but more than
patient was being treated with an anti-epileptic drug (lamotrigine) as
100 other medications have been implicated.
preventative therapy. Stevens Johnson Syndrome was diagnosed.
Wound Healing Southern Africa
2008 Volume 1 No 1
Case Study : The WHASA Wheel
SJS and TEN are probably the same condition, the name SJS being
oedema makes footwear difficult and is a major cause of foot
applied when less than 10% of the skin surface is involved, TEN
ulceration. Wearing roomy shoes, with fastenings that can improve
when more than 30% of the skin surface is involved, and SJS-TEN
width fitting (such as laces or Velcro fastenings) may be required
overlap when the involvement is 10-30 %. Skin involvement is
until the peripheral oedema is resolved. Post surgical compression
usually preceded by malaise, fever, cough and a sore throat.
hose may be required based on the input of the vascular surgeon. Custom footwear may need to be considered in col aboration with
Skin lesions usually begin on the face and trunk and spread rapidly
the orthotist.
to involve other areas of the body. The initial lesions are macular, and may remain so, fol owed by desquamation, or may transform
The fracture and reconstruction of the left leg is bound to alter lower
into target lesions with purpuric centres, and may even form bullae,
limb mechanical function, placing uneven forces on one or both
which will later slough. Mucosal surfaces are almost always involved:
feet which may increase the risk of foot ulceration. This needs to
the oral mucosa and the conjunctiva being the most frequently
be assessed; and measures taken to normalise foot function with
affected. The genitalia, oesophagus and respiratory epithelium can
the use of an in-shoe device, such as foot orthoses, and/or shoe
also be involved. Consequently, eating, drinking and urinating can be
extremely painful.
Case report continued
The pathogeneses of SJS and TEN have not been fully elucidated. Histology in both conditions shows extensive keratinocyte apoptosis.
Following 10 days of aggressive treatment for the dermatologic
It is now hypothesised that the apoptosis is caused by the suicidal
condition and dressings of the sacral pressure sore and heel sore,
interaction of Fas which is expressed by keratinocytes and increased
the sacral area was clean enough for definitive closure and the
amounts of soluble Fas ligand (sFasL) secreted by peripheral blood
heel sore had resolved. Ongoing cleaning and maintenance of the
mononuclear cells (PBMC's).
sacral area was extremely difficult due to the proximity to the anal area. Surgeons thus decided to perform a defunctioning colostomy
Management of these patients is similar to those with an extensive
(cognisant of the previous abdominal reconstruction performed).
burn. Most patients are hospitalised and suspected drugs are immediately stopped. Fluid and electrolyte balance must be
Once the patient had once again stabilised, he was returned to theatre
maintained via intravenous fluids. Bacteraemia and septicaemia
and the plastic surgeon performed a bilateral V-Y advancement flap
are common complications and can result in death. Appropriate
for closure of the sacral pressure sore (Figure 10).
antibiotics are usually given intravenously. The use of intravenous
The patient stil suffered from residual skin hypersensitivity and
steroids is controversial: in theory the use of immunosuppressives
was treated by the stoma therapist for stomal dermatitis. The cause
is to prevent further "immune" damage to the skin. Whether there
appeared to be an inadequate seal and leakage of effluent. Once this
is any benefit remains controversial and certainly once most of the
was corrected overall healing occurred uneventfully.
skin is lost, steroids only add to the morbidity and perhaps mortality of the patients.
More recently, reports of high doses of intravenous immunoglobulin (IVIG), administered within the first 4 days of onset of SJS/TEN have shown promising results. It is felt the IVIG blocks the Fas- sFasL interaction and thereby reduces/stops apoptosis. Renal function, which may already be impaired, must be carefully monitored, as there are reports, especial y in adults, of deterioration of renal function following IVIG administration. In patients who survive, re-epithelialisation takes 3-4 weeks. Complications include scarring, loss of vision and blindness. Mortality averages 5% for SJS patients
Figure 10: Grade 4 sacral pressure sore closed with V-Y advancement flap
and 30% for those with TEN. A rule of thumb is that the mortality rate parallels that of skin involvement i.e. 50% skin involvement will
Comments WHASA Wheel partner –
result in a 50 % mortality rate.
Wound care specialist: Prof Magda Mulder
Comments WHASA Wheel partner –
It is essential to try and prevent pressure sores in all bedfast
Podiatric specialist: Joanne Crawford
patients. (Prevention is better than cure.) An important aspect of the
This patient appears to have intact sensation; however a thorough
prevention of bedsores is the identification of those who run the risk
medical history and comprehensive clinical examination may reveal
of developing them. If it appears that a patient does run that risk,
subtle signs and symptoms of early peripheral neuropathy. This
adequate precautions in terms of a scientifically based nursing care
patient needs education on the foot complications of diabetes and
plan must be implemented from the time of admission.
the importance of good metabolic control to prevent or reduce future
A number of pressure sore risk assessment instruments are available,
foot complications.
e.g. the Norton, Douglas, Waterlow, Gosnell and Braden scales.
The immediate podiatric concerns in this situation are the right heel
Pressure sore risk assessment scales attempt to identify the
and peripheral oedema. The resolved pressure ulcer of the right
presence of extrinsic and intrinsic factors that are known to increase
heel may require in-shoe cushioning/accommodation now that
an individual's susceptibility to pressure damage, and to quantify the
the patient is ambulatory, to protect the recently healed area from
risk with a numerical scale.
breakdown. Post surgery any peripheral oedema must be assessed,
Wound Healing Southern Africa
2008 Volume 1 No 1
Case Study : The WHASA Wheel
Since most patients' conditions do not remain static, pressure sore
Case report continued
risk assessment should be seen as a dynamic process. Patients should be reassessed when their conditions alter.
One week fol owing the sacral surgery the patient was transferred to a general ward and began his process toward recovery. He was
Consequently the precautions must be continuously adapted
now ambulatory, metabolical y stable and recovery transpired
uneventfully from here. Two months following this severe injury,
Comments WHASA Wheel partner –
multiple surgeries and concomitant complications the patient was
Stoma therapy specialist: Sr Jane Hoole
discharged from hospital. His holistic management involved 11 different specialists working in tandem.
Trauma: There are many injuries involving the colon, anus, rectum and perineal area that may require temporary diversion of the faecal
Two years fol owing this episode, the patient presented to the wound
stream. The most common of the diversions is the colostomy. The
care clinic with a non-healing ulcer of the left leg (Fig 15). Armed with
patient wil have the stoma until continuity of the distal tract can
a history of significant trauma to the leg, an ankle -brachial index
be restored.
of greater than 0.8 and the typical appearance of the wound, the wound care sister diagnosed a venous ulcer. The vascular surgeon
Obstetric injuries, skin grafting of extensive sacral pressure
was informed and treatment was instituted with hydrogels, foams
ulceration, extensive anal fistulae are but a few of the indications for
and most importantly compression bandages to the area. Healing
diversion of the faecal stream, thus preventing wound contamination
was accomplished over the fol owing six weeks and the patient
in the perineal area.
received training in long term maintenance (stockings, diet, hygiene,
exercise, etc) of this condition.
Figure 11: Loop Colostomy
Figure 12: Loop colostomy 1 day
following surgery
Peristomal dermatoses are a significant problem, affecting more than one third of patients with colostomies and more than two thirds of patients with urostomies and ileostomies. The most common cause of peristomal dermatitis is the leakage of effluent due to ill fitting/incorrect use of the various pouching systems and accounts for approximately 22% of al skin problems. Al ergy accounts for only 0.6% of skin problems.
Figure 15: Venous Ulcer
There are however, many and varied reasons for the development of peristomal dermatoses besides leakage, example: psoriasis,
Comments WHASA Wheel partner –
eczema, allergens and disease.
Wound healing specialist: Prof Magda Mulder
As the patient is diabetic, infection due to abnormal cellular and/or inflammatory responses is always a great risk. In view of this, a bone scan must always be taken first to exclude osteomyelitis before compression bandages are applied.
Secondly, ankle-brachial pressure index values are not very reliable in diabetics. An ABPI of 0.8 can therefore be misleading due to arteriosclerosis because the hardened arterial walls are not effectively occluded by the cuff. Transcutaneous oximetry (TcPO2)
Figure 13: Second degree burn ileal
Figure 14: Persistent irritation
would therefore be a better option. A TcPO2 of less than 40 mmHg
colostomy effluent
at a temperature of 44ºC on the dorsum of the foot indicates tissue vulnerability, while a value of 10 mmHg indicates critical limb
Comments WHASA Wheel partner –
Plastic surgery specialist: Prof Widgerow
Should it appear that the arterial supply is adequate and that the
The V-Y advancement flap is not the workhorse for closure of sacral
application of compression would be safe, the patient must be
pressure sores. Closure utilising this technique results in an incision
careful y assessed beforehand for peripheral neuropathy. The
line directly in the area of pressure. This is only acceptable in the
application of compression bandages in the presence of peripheral
above case as the patient is ambulant (at this stage) and the area is
neuropathy can be risky as the patient wil be unaware of symptoms
sensate. Other choices (such as rotation flaps, gluteal island flaps)
such as a local burning pain that could indicate possible underlying
would be better in paraplegic patients.
Wound Healing Southern Africa
2008 Volume 1 No 1
Case Study : The WHASA Wheel
If compression bandages are applied, the patient should preferably
also wear a sandal with Velcro straps on the foot of the affected leg.
1. Rodriguez, Eduardo D. D.D.S., M.D.; Bluebond-Langner, Rachel M.D.; Silverman, Ronald P. M.D.;
A half-stocking must be pul ed over the toes to protect them against
Bochicchio, Grant M.D.; Yao, Alice B.A.; Manson, Paul N. M.D.; Scalea, Thomas M.D. Abdominal Wall Reconstruction following Severe Loss of Domain: The R Adams Cowley Shock Trauma Center Algorithm.
trauma and to prevent smal particles such as pebbles from landing
Plastic & Reconstructive Surgery. 120(3):669-680, September 1, 2007.
between the sole of the foot and the bandages.
2. Miller, Preston R. MD; Meredith, J Wayne MD; Johnson, James C. PA-C; Chang, Michael C. MD
Prospective Evaluation of Vacuum-Assisted Fascial Closure After Open Abdomen: Planned Ventral Hernia Rate Is Substantially Reduced. Annals of Surgery. 239(5):608-616, May 2004.
After the ulcer has healed, compression bandages must be applied
3. Miller, Preston R. MD; Thompson, James T. MD; Faler, Byron J. BS; Meredith, J. Wayne MD; Chang,
for a further two to three weeks as premature degradation of col agen
Michael C. MD Late Fascial Closure in Lieu of Ventral Hernia: The Next Step in Open Abdomen Management. Journal of Trauma-Injury Infection & Critical Care. 53(5):843-849, November 2002.
may occur in diabetics.
4. Stone, Patrick A. MD; Hass, Stephen M. MD; Flaherty, Sarah K. BS; DeLuca, John A. MD; Lucente, Frank
C. MD; Kusminsky, Roberto E. MD Vacuum-Assisted Fascial Closure for Patients With Abdominal Trauma. Journal of Trauma-Injury Infection & Critical Care. 57(5):1082-1086, November 2004.
5. Scott, Bradford G. MD, FACS; Welsh, Francis J. MD; Pham, Hoang Q. MD; Carrick, Matthew M. MD;
Liscum, Kathleen R. MD, FACS; Granchi, Thomas S. MD, MBA, FACS; Wall, Matthew J. Jr MD, FACS;
Wound healing forms the basis of medicine in al its forms. It is
Mattox, Kenneth L. MD, FACS; Hirshberg, Asher MD, FACS Early Aggressive Closure of the Open
noteworthy that the speciality has found its own unique position
Abdomen. Journal of Trauma-Injury Infection & Critical Care. 60(1):17-22, January 2006.
6. Pretre, Rene MD; Bruschweiler, Ivan MD; Rossier, Jacques MD; Chilcott, Michael MD; Bednarkiewicz,
in medicine today as the incorporation of basic science, general
Marek MD; Kursteiner, Karine MD; Kalangos, Afksendiyos MD Phd; Hoffmeyer, Pierre MD; Faidutti,
medicine and surgery in all its forms all contribute to furthering the
Bernard MD Lower Limb Trauma with Injury to the Popliteal Vessels. Journal of Trauma-Injury Infection & Critical Care. 40(4):595-601, April 1996.
knowledge and advancement of this field. The above case il ustrates
7. Steenvoorde, Pascal M.D., M.A.; van Engeland, Anneke M.D.; Oskam, Jacques M.D.,Ph.D. Vacuum-
the co-operative ideal of multi-specialist input in managing a patient
assisted closure Therapy and Oral Anticoagulation therapy Plastic and Reconstructive Surgery Volume 113(7), June 2004, pp 2220-2221.
with multiple problems and one common goal – achieving wound
8. Kocak, Sedat 1; Girisgin, Sadik A 1; Gul, Mehmet 1; Cander, Basar 1; Kaya, Halil 1; Kaya, Esengul 2
healing efficiently and effectively. Herein lies the WHASA wheel of
Stevens-Johnson Syndrome Due to Concomitant Use of Lamotrigine and Valproic Acid. American Journal of Clinical Dermatology. 8(2):107-111, 2007
Figure 16: WHASA Wheel
Wound Healing Southern Africa
2008 Volume 1 No 1
Source: http://www.woundhealingsa.co.za/index.php/WHSA/article/viewFile/6/7
nuweb9.neu.edu
The EMBO Journal (2006) 25, 868–879 & 2006 European Molecular Biology Organization All Rights Reserved 0261-4189/06 Y-family DNA polymerases respond to DNAdamage-independent inhibition of replication forkprogression Veronica G Godoy1,3, Daniel F Jarosz2, properly restored. Mutations in components of such check- Fabianne L Walker1,4, Lyle A Simmons1
nada-danmark.dk
Using the NADA Protocol to Improve Wellbeing for Prostate Cancer Survivors: Five Case Studies Beverley de Valois and Tarsem Degun cardiovascular disease, and cardiac events. Distress, anxiety, This paper presents case studies of five men diagnosed and irritability, depression, and loss of confidence are emotional and