Microsoft word - lecture_no._15_gerd_tw_25052008.doc


Lecture no. 15
Esophageal Motility Disorders - 3
Gastroesophageal Reflux Disease
This chapter could begin like this: the esophageal mucosa is unable to endure contents
coming from the stomach. These contents may be fluids secreted by the stomach itself (the most oft-occurring possibility), or even duodenal-biliary in origin. These events lead to a anatomical-clinical condition that generally goes by the name of esophagitis.
The pathogenic action of the refluxate on the esophagus, nonetheless, depends on the
duration of the contact. When motility of the esophageal-cardia-stomach complex is normal, any refluxate is quickly eliminated through the expulsive action of the esophageal musculature.
This reflux disorder is thus induced by an irregular esophageal-gastric motility function, in
particular by the ineffectiveness of the principal antireflux agent, the lower esophageal sphincter (LES). In order to perform its elective function, this segment of the terminal esophagus with sphincteral functions (functional sphincter) must have an appropriate length (3 - 5 cm) and, during closure, sufficient pressure (10 - 20 mmHG) to contrast the subdiaphragmatic pressure of the stomach. Moreover, this high pressure zone (HPZ) owes its optimal function to its extension above and below the diaphragm: its complete dislocation above the diaphragm weakens its functioning. The activity of the LES is coordinated with the propulsive function of the esophagus and the receptive function of the gastric fundus.
The etiopathogenesis of pathological gastroesophageal reflux is thus traceable to the
abnormal function of the LES (Fig.1), which is normally accompanied by other factors that often
impact on the entity and extent of injury of the phenomenon: as already mentioned, these factors lie
in the clearing capacity of the esophagus and how compliant the fundus is to receive content.
Nevertheless, the motility activity of the gastro-pyloric-duodenal complex must also be accounted
for, which - more than is believed - influences the pathogenesis and severity of gastroesophageal
reflux disease (GERD).
Fig. 1 - Computerized 3D reconstruction of the esophageal manometry
LES: a) normal; b) in subject with reflux
If the stomach does not empty as it should, and the refluxate - which is often highly acidic -
stagnates in the stomach, it is easy to imagine the severity of the consequences GERD can have on the esophagus. As is known, this egestive function is the task of the pyloric antrum, which may be compromised by any of a number of conditions: chronic inflammation, modifications in mucosal trophism (chronic atrophic gastritis, dysplastic or metaplastic phenomena), primary alterations of gastric motility. Antral activity - responsible for physiologically normal gastric emptying and clearing of duodenal-gastric refluxate - even if fundamentally valid, may feel the dyskinetic effects of the duodenum. In fact, uncoordinated duodenal contractions can create resistance to the passage of gastric chyme into the duodenum through the pyloric ring (Fig. 2 - 6). This, beyond impeding correct gastric
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)


emptying, can induce pathological duodenal-gastric reflux, since the antrum is no longer in the
condition to exercise its clearing function. Prolonged contact with duodenal content causes serious
damage to the gastric mucosa, giving rise to so-called alkaline gastritis, better known as alkaline
gastropathy. As a result, two significant pathological conditions are created: greater availability of
refluxate from the stomach, and possible contamination of the same with duodenal material.
We, too, have documented the same elevated frequency of delayed gastric emptying in
patients with gastroesophageal reflux, reflecting and confirming the above-mentioned notions (Fig.
7). Depending on the motility pattern of the esophageal-gastric-duodenal complex, the pH of the
refluxate may alter the reflux, resulting in a condition that is, with decreasing frequency, either
acidic, mixed or alkaline. This frequent involvement of the entire upper digestive tract in the reflux
syndrome could very well elicit the term duodenal-gastroesophageal reflux disease (D-GERD).
What has been described above overturns some traditional convictions that attributed reflux
disease to the failure of some anatomic structures, such as Bertelli-Laimer's phrenoesophageal ligament, the acute angle between the esophageal margin and the gastric fundus (angle of Hiss), Allison's sling, etc.
Fig. 2 - esophageal and gastroduodenal manometry under conditions of normal motility. a) esophagus: the lower tracing corresponds to the high pressure zone (HPZ) at the level of the LES. The relaxations coordinated with the primary esophageal wave are evident. b) stomach (ST) - duodenum (D): the prevalence of antral propulsive wave pressure compared to duodenal wave pressure is noteworthy
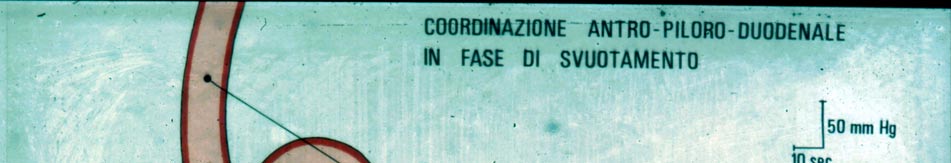
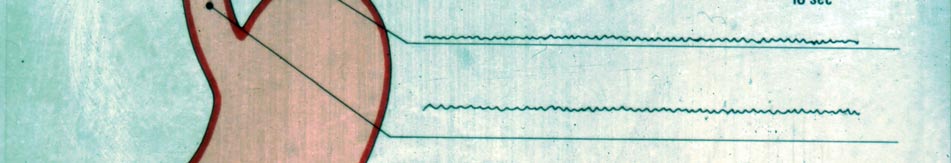
Fig. 3 - Schematic representation of motility activity normally under
antral-pyloric-duodenal coordination during gastric emptying.
The second tracing from the top corresponds to the HPZ/LES
during closure (anti-reflux function).
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
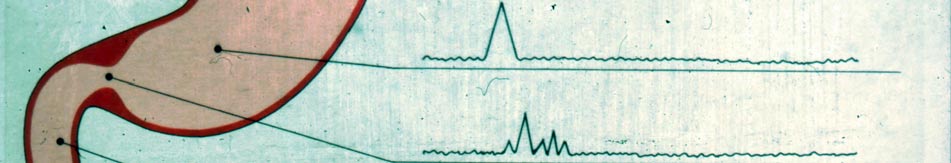
Fig. 4 - Serious duodenal hyperdyskinesia
Differences with the tracings in Fig. 2b are noticeable
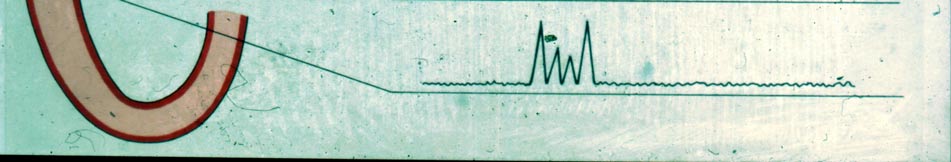
Fig. 5 - a) Difficulty in gastric emptying due to the prevalence
of duodenal over antral kinesis.
b) Normally coordinated gastroduodenal motility conditions.
Fig. 6 - Difficulty in gastric emptying and the possible
duodenal-gastric reflux are mutually responsible for GERD.
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
Gastroesophageal reflux disease is undoubtedly the most frequent esophageal disorder,
above all in the Western world: the increasingly widespread habit of consuming of rapidly-eaten meals (i.e., fast food), which compromises important proximal digestive mechanisms (mastication, salivation, etc.) is often viewed as the chief culprit of the upward trend of the disorder; the quality of foodstuffs is also called into play. In all likelihood, no less than 40-50% of the population experiences symptomatic gastroesophageal reflux, even though the discomfort is most often relieved with simple therapeutic expedients. The number of subjects requiring surgical intervention amounts to approximately 4-5/100,000. These numbers need to be viewed with caution, since gastroesophageal reflux - because it is not acidic (but mixed or alkaline) - may be clinically silent an undefined percentage of subjects. As we will see below, this situation is particularly dangerous for the serious esophageal damage that it can cause.
The symptomatology of acidic gastroesophageal reflux consists principally of pyrosis, a
burning sensation, painful at times in the sternal region, which is preceded by an analogous feeling in the epigastric region. This burning pain may be transitory or may persist, often radiating upwards until it reaches the neck, not rarely resulting in acidic regurgitation above all in a resting supine position, creating burning in the throat and setting the teeth on edge. Coughing and laryngeal disturbances are often frequent: otolaryngologists are well aware of laryngitis due to gastroesophageal reflux, that very often poses problems of differential diagnosis. The chance that even the slightest amount of refluxate is aspirated into the tracheobronchial tree leads to types of ab ingestis diseases of varying degree (bronchitis, bronchospasm with asthmatic symptoms, pneumopathies). The esophageal pain (esophagodynia) resembles cardiac pain to such an extent that the symptomatology of angina-like esophageal reflux has been described. At times, above all in an upright position, small amounts of extremely acidic gastric juice may reflux into the esophagus. This may induce a sudden spasm of the esophageal musculature, perhaps as a defense mechanism, which nonetheless provokes intense pain in the anterior region of the thorax, obviously including the precordial area, that naturally alarms whoever experiences it. Normally in situations such as these, a few acts of swallowing (esophageal clearing) suffice to resolve the phenomenon. Moreover, vagal stimulation, which the acidic refluxate exerts on the esophageal mucosa, may induce bradycardia and extrasystole. By contrast, if the refluxate is mixed or alkaline - because this is caused by biliary content - in the absence of symptoms such as those described for acidic reflux, a pathognomonic signal of the
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
disorder may be the yellow bile stain found on the pillow in the morning upon wakening, in addition to a bitter taste in the mouth.
The elective target of GERD is the esophagus, particularly its mucosal sheath, on which the
refluxate provokes inflammatory alterations - esophagitis - of varying degrees of severity, above all
in the supracardial segments and, any rate, the distal third of the esophagus. Esophagoscopy can
detect and classify this disorder. The pathologist then further defines the extent of the esophagitis by
examining in detail the damage to the mucosa on biopsy specimens.
On the basis of the results we have the classification of reflux-induced esophagitis:
Erythematous or erythematous-edematous esophagitis Erosive esophagitis, in which erosions may be (in order of severity): a) single or multiple, but
on one fold only; b) multiple and confluent on more than one fold; c) circumferential and confluent.
Ulcerative or ulcerous-hemorrhagic esophagitis, in which ulcers may be rare and superficial, or
extensive, deep and sanious. These latter tend to bleed easily on contact with the endoscope.
Stenosing or sclero-cicatricial esophagitis, which represents the scarring result of healed ulcers.
Should the sclero-connective tissue involve deeper layers of the esophagus, in particular the muscular sheath, and have a circumferential development, the emergence of a stiff, inelastic and, lastly, stenotic esophageal segment is likely.
Barrett esophagus (BE) (Norman Barrett, 1950), or metaplastic esophagus, indicates the
presence of intestinal-type metaplastic columnar epithelium in the supracardial esophagus. The prominent endoscopic feature is a raised Z-line (gastroesophageal junction), recognizable by the transition from a whitish mucosal lining (of the esophagus), to one resembling a reddish gastric and cardial tract lining. This Z-line ascension may be circumferential, or may be reddish and tongue-like (flame projections), which varyingly advance along the esophageal lumen. In other occasions, the disorder is evident through metaplastic islands in the esophageal mucosa. Two forms of BE, named accordingly by the extent of the ascension of the metaplastic columnar metaplasia, are recognized: long Barrett (> 3 cm) and short Barrett (< 3 cm). From a histological standpoint the metaplasia may be:
a) specialized intestinal (villi, crypts, mucosa secreting columnar cells, etc.); b) gastric fundic type; c) junctional type.
At this point it is worthwhile to reiterate the already mentioned notion that symptomatology
is due largely to the type of reflux. Generally, acid reflux is more symptomatic than alkaline or mixed reflux, this latter often entirely asymptomatic. As a consequence, the entity of symptoms can not always be correlated to the severity of esophagoscopic or biopsy samples. It is thus possible to encounter patients with intense subjective symptoms, those with only mild esophageal alterations (e.g., erythematous), or subjects with multiple symptoms whose serious alterations are completely asymptomatic. Hence, compared to other forms of reflux, the symptoms ensuing from acid reflux greatly facilitate diagnosis.
These - alkaline or mixed - are far more insidious for the damage that they slowly and
deceptively induce. Therefore, a serious and poorly treatable hypochromic anemia may obviously represent a cause for alarm. The presence of occult blood in stools will, as a rule of thumb, occasion diagnostic tests aimed at detecting the source of the hemorrhage. The absence of symptoms and other usual signs of disease (e.g., colon lesions) will ultimately lead (with difficulty) to an
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
esophagoscopy, which will reveal an ulcerative esophagitis as the cause of the hematic oozing (protracted microhemorrhage).
Another serious consequence of esophagitis due to alkaline or mixed reflux is stenosis of the
supracardial segment of the esophagus or, at any rate, the lower third of the organ: total dysphagia (solids and liquids) and regurgitation. Because symptoms manifest themselves without prodromic events, the first clinical and radiological diagnostic interpretation points to a neoplastic lesion, and not infrequently the esophagoscopic and biopsy examination may also not yield conclusive evidence on the nature of the stenosis.
Barrett esophagus represents another serious condition, the result of a usually prolonged -
particularly dangerous if asymptomatic - esophagitis. This complication may be detected following hemorrhagic or stenotic phenomena, or on radiological examination that evinces a certain shortening of the esophagus as my be seen with some forms of esophagitis-induced stenosis. The severity of BE lies in the neoplastic risk that the lesion harbors. It is estimated that 5-6% of cases evolves into adenocarcinoma, thereby labeling BE as a preneoplastic lesion. According to many authors, the risk of cancer in BE ranges from 20 to 350 times greater than that in normal esophagus. Running parallel to the increased incidence of GERD in Western populations is the prevalence of BE, which some investigators calculate at 22/100,000 subjects in endoscopic cohorts, but which other autopsy studies estimate to be 17 times higher, equal, that is, to 376/100,000. These figures coincide with the increase in Western populations of adenocarcinoma of the cardia/terminal esophagus, which together with tumors of the fundus has surpassed the (already prevalent) incidence of antral stomach cancer and, at final analysis, with the above-mentioned rise in the frequency of GERD in the same population.
Acid gastroesophageal reflux may be responsible for two other esophageal defects:
• Sliding hernia and related shortening of the esophagus (acquired short esophagus),
• Zenker's pharyngo-esophageal diverticulum.
As already stated, acidic refluxate exerts a motility reaction on the circular musculature of
the esophagus that affects clearing & cleaning. This reaction may to some extent and sporadically involve the longitudinal musculature, which, if the stimulation is protracted and repetitive, is able to shorten the organ and "pull" the esophagus-cardia-fundus complex upwards. Indeed, the impressive elastic properties of the esophagus thanks to the longitudinal musculature are well-known: during an esophagectomy, if not appropriately fastened to a device for pathological examination, the surgical specimen shortens noticeably.
The same defense mechanism against reflux may affect the upper esophageal sphincter,
which in cases of repeated stimulation may become dyschalasic, with the resulting formation of the diverticulum. Indeed, in Lecture no. 2 on this website - entitled Zenker's Diverticulum - the section on the etiopathogenesis of this disorder reads: "The causes underlying this discoordination may be primary, but are most often secondary to a gastroesophageal reflux disorder (GERD). This leads to a dyskinetic-hyperkinetic motor reaction in the esophagus that may also involve the UES. Nearly 2/3 of our cases showed lower esophageal sphincter (LES) incontinence, with GERD. An understanding of these etiopathogenic and anatomopathological features characterizing symptoms is crucial to defining the proper therapeutic approach."
• Esophagus-stomach-duodenum radiography
The examination performed in Trendelemburg position with epigastric compression may reveal the ascent of barium meal into the esophagus and possible related esophageal alterations, either functional (dyskinesia) or organic (sliding hernia, short esophagus, stenosis, etc.).
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
• Esophagoscopy with biopsy
hyperemic erosive
esophagitis ulcerative
cicatricial stenotic
Barrett esophagus
• Esophagus-gastro-duodenum manometry
LES study basal average tone
% relaxation duration of relaxations
and, if needed (non-acidic refluxate), study of gastric and duodenal motility.
• 24-hour esophageal-gastric pH monitoring (Fig. 8 - 9)
average pH value during registration total number of acid reflux episodes
Parameters overall duration of acid reflux (% of time)
number of episodes lasting > 5 minutes duration of the longest episode
number of symptom-related reflux episodes
Symptomatic index
total number of symptoms
N.B.: in cases of mixed reflux pH monitoring may not be helpful
Fig. 8 - 24-hour gastroesophageal pH monitoring. Upper tracing: esophagus / lower: stomach. Numerous
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
Fig. 9 - Examples of 24-hour pH monitoring tracings in patients with mixed reflux
• Study of gastric emptying: -a) ultrasound -b) radiological (Madsen and Rasmussen
method) -c) radioisotopes
reflux subjects without esophagitis
217,5 m' +/- 48,13
reflux subjects with esophagitis
378 m' +/- 123,03
• Cholescintigraphy (HIDA) (Fig.10)
Fig. 10 - Cholescintigraphy (HIDA scan) with 99mTc: alkaline gastroesophageal reflux
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
• Measurement of esophageal bilirubin (Bilitec®)
• Impedance manometry
Impedance is the resistance to the flow of an electrical current (measurement of the electrical conductivity of an organ's content).
Low Conductivity = High impedance
Esofageal wall
Refluxate
High Conductivity = Low impedance
Fig. 11 - Impedance scale
Medical therapy
Acid gastroesophageal reflux is the most frequent manifestation of GERD and, as already
mentioned, the most symptomatic. The epigastric and retrosternal sensation of burning worries the patient, who as soon as possible consults the physician. This (acute) phase is therefore easily recognizable and, lacking other, more important, disturbances - above all those emerging recently - generally do not require instrumental diagnostic tests. The disturbance is often triggered by eating disorders or by the intake of substances (NSAIDs, corticoids, alcoholic beverages, etc.) able to induce gastric inflammation (acute gastritis). This condition may compromise - perhaps only temporarily - and disable the function of the LES. The following sequence of events thus ensues: acidic gastric hypersecretion, prolonging of gastric emptying times, and acid esophageal reflux. This event may be episodic and easily treatable with antacids and dietary modifications, or by suspending the intake of those substances that were found to be responsible for the disturbance. Should this scenario persist, it is likely that conditions which are much harder to resolve have taken root, and for which more aggressive measures must be taken. This ushers in the so-called short-term treatment of GERD, non-pharmacological and pharmacological.
Non-pharmacological approaches mainly entail measures aimed at modifying life-style.
These can be summarized as:
Sleeping in a semi-upright position (elevating the head approximately 20 cm); Losing weight (if overweight); Drinking liquids (water) between meals; Avoiding chocolate, coffee, tea, carbonated bevarages, wine/alcohol, herbs and spices (basil,
parsley, mint, marjoram, etc.), fatty foods;
Avoiding gastrointestinal-damaging agents.
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
It is estimated that approximately 60% of cases achieve improvement with such measures.
The pharmacological approach to the treatment of GERD is based primarily on antacids,
antisecretory agents and prokinetic drugs. Protonic pump inhibitors (PPI), omeprazole and derivatives (lansoprazole, pantoprazole, rabeprazole) are the most frequently used drugs, having supplanted H2 receptor antagonists. The most often used prokinetic agent is metoclopramide.
As stated, this treatment may be short-term and is effective against the disorder after eight
weeks in more than 90% of cases. However, GERD recurs frequently, and affects a number of so-called non-responders. Under these circumstances, or when faced with symptoms that are atypical, or at least do not reflect the classic picture of acid reflux (dysphagia, esophagodynia, odynopahgia, epigastralgia, bile regurgitation, cardiac and pulmonary symptoms, etc.), instrumental diagnostic investigation becomes compulsory.
As GERD becomes chronic, and with it the clinical picture becomes complicated or atypical,
surgical intervention is indicated.
Surgical therapy
R. Nissen (Gastropexy and fundoplication in surgical treatment of hiatal hernia Am. J. Dig.
Dis. 6:954-961, 1961), conceived the procedure still bearing his name today, which resolves the pathophysiological defect underpinning the cause of GERD, namely LES incompetence.
Nissen fundoplication, the originally devised version of which was further elaborated and
refined by his deputy and collaborator, Rossetti, is the surgical procedure of choice to treat GERD.
The operation (Fig. 12), which is easily performed laparoscopically (see videos), entails wrapping
the inferior part of the esophagus with a sleeve of the gastric fundus, which is thereby literally
plicated around it (total fundoplication).
Fig. 12 - Nissen-Rossetti fundoplication
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
The gastric fundus, wrapped 360° around the esophagus, is able to restore a high pressure
zone (neo-HPZ) in the esophageal segment corresponding to the LES (Fig. 13), thanks to its ability to contract in a quiescent phase and to release during swallowing.
Fig. 13 - Computerized 3D reconstruction of the esophageal manometry signal
- new HPZ after fundoplication -
The post-swallowing release afforded by the gastric fundus to the swallowed bolus is thus
exploited. The operation must assure the repositioning of an adequate segment of the esophagus in the abdomen, i.e., restoring the HPZ between the thorax and abdomen to its correct position (in addition, naturally, to recreating sufficient pressure). This much be carefully calibrated in order to avoid inducing a dyschalasia, or worse yet, an achalasia, in the event the fundoplication is too tight. Some methods are available to achieve this calibration: preoperative manometry, the guide of calibrated endoesophageal probes, the crocodile test (whereby the jaws of a forceps inserted between the sleeve and the esophageal wall openly easily), the floppy Nissen procedure, etc. When cardial incompetence is accompanied by long delays in gastric emptying, and pyloric hypertone has been confirmed, it may be convenient to weaken the pyloric function together with the Nissen (anterior pylorectomy or pyloroplasty). In confirmed cases of esophageal motility hypofunction, a posterior 270° partial fundoplication (Toupet procedure) may be performed. To prevent the possible prolapse of the fundoplication into the thorax (slipped Nissen), the fundic sleeve may be fastened with a couple of stitches to the anterior wall of the stomach (Rossetti's stitch) or to the esophageal wall; moreover, drawing the diaphragmatic pillars of the hiatus together with a few stitches is also useful. In this regard it must be pointed out that the hiatus is often wide and permits the formation of a sliding hernia. In these cases becomes even more advisable to modify the pillars, and, at times, application of a prosthetic mesh may be necessary.
The major complications of GERD - cicatricial stenosis and acquired shortening of the
esophagus - require more aggressive intervention: in the first case, esophageal resection with
recanalization via a loop positioned between the esophageal stump and stomach - jejunum
(Merendino), colon (Belsey) - lengthening of the esophagus - Collis gastroplasty - in the second.
Duodenal Gastroesophageal Reflux Disease (DGERD)
As already mentioned, gastroesophageal reflux is sometimes accompanied by delayed gastric
emptying. Generally, the surgical correction brought about by Nissen fundoplication restores the normal gastric egestive function., even when refluxate in the esophagus is - episodically and in low amounts - mixed with bile and pancreatic juice. Sporadic mixing of this kind may play a role in the pathogenesis of esophagitic lesions, but it does not meaningfully alter the therapeutic approach.
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
A completely different scenario presents when bile and pancreatic juice reach a high
concentration in the stomach and persistently and conspicuously reflux into the esophagus. This generally comes about due to impaired motility activity of the antrum (Fig.14), to a duodenal barrage resulting from hyperdyskinesia of the same, or both mechanisms (Fig.15).
Fig. 14 - Gastric adynamia
Fig. 15 - Duodenal barrage
Such conditions, for starters, will negatively condition the results of a simple Nissen
fundoplication, setting the stage not only for the likely recurrence of esophageal reflux, but also for the development of new and serious symptoms, which are at times worse than those preceding surgery, such as gas-bloat syndrome(Fig. 16) or gastric ulcer.
Fig. 16 - Duodenal-gastroesophageal reflux disease (D-GERD) cannot be resolved
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
It therefore becomes necessary to accurately recognize DGERD patients and to
distinguish them from subjects with simple GERD. Such a differential diagnosis is not always
easy. We have already mentioned that patients with non-acid reflux may not present esophageal
symptoms. Nevertheless, in subjects with clear evidence of disease, the physician must be alert to
other disturbances which often manifest themselves. These can be summarized as follows:
epigastralgia hyporexia dyspepsia epigastric tension after meals ("food doesn't agree with me") nausea vomiting of bile and at times food weight loss anemia anxiety
These patients require the use of all of the previously cited instrumental diagnostic means. Aware of
the potential neoplastic risk of both esophageal (Barrett) and gastric (metaplastic-dysplastic) lesions,
endoscopic biopsy takes on extreme importance in these cases.
When these dangerous signs are absent, medical therapy, which is still based chiefly on the
use of antisecretory and prokinetic agents with a mindful watch on the possible evolution of the disease, may be attempted.
Here, more so than for GERD, surgical treatment with conservative - defined as functional -
and ablative procedures, is indicated. The former entail combining a non-resective operation with the fundoplication, which improves gastric emptying and rids the stomach of bile and duodenal juice, thereby correcting the motility alterations that cause the disorder. These can be employed when the stomach does not present serious lesions, when antral activity is still adequate and when migratory motility complexes (gastrointestinal motility activity) is still intact. The following constitute non-ablative, functional procedures:
extramucosal duodenal myotomy (EDM) (Fig. 17 - 20) (Mattioli et al. Gastroenterology 1981 - Minerva Chirurgica 1989), indicated in cases of primary, prevalent duodenal hyperdyskinesia (see images); anterior pylorectomy (F. Holle) only if isolated pyloric hypertonia is present (the operation
entails the extramucosal removal of the anterior segment of the pyloric ring, thereby further reducing sphincteral activity);
duodenal switch (Fig. 21) (T.R.De Meester, Ann. Surg. 1987) (see images).
Demoltive procedures, necessary in the presence of serious gastric lesions and compromised antral
activity, are principally represented by subtotal gastric resection and recanalization, also known as
Roux-en-Y total duodenal diversion.
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
Fig. 17 - Extramucosal duodenal myotomy (EDM)
Fig. 18 - A total fundoplication together with EDM resolves the problem.
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
Fig. 19 - a) Mobilization of the duodenal-pancreatic block.
b) tracing of the EDM
Fig. 20 - Extramucosal duodenal myotomy
Fig. 21 - Duodenal Switch Fig. 22 - Total duodenal diversion
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
Barrett Esophagus
The management of patients with BE is not simple, let alone univocally shared by all
practitioners. The truth is that our understanding of this complication arising from reflux disease, especially of the degree of neoplastic risks, is far from thorough.
At present, the extension of the metaplastic area (short or long BE) and the degree of
dysplasia provide the grounds for prognosis and, hence, criteria for treatment. Therapeutic choices are thus made on endoscopic evidence and on biopsy findings. Debate currently addresses questions like whether BE without dysplasia can regress after medical and/or surgical antireflux therapy, or whether the evolution of low-grade dysplastic disease can stop (regress?) after treatment. Even if these possibilities are viable, the absolute need remains for long-term monitoring, which, with increased signs of high risk, must be performed with greater frequency. The alterations found in high-grade dysplasia (cellular atypia, varying degrees and combinations of epithelial and architectural disorder, etc.) are unanimously interpreted as being equivalent to those found in in situ carcinoma.
In summary, the treatment of BE is conditioned by the above-mentioned evidence. Initially, a
conservative approach may be hypothesized, bearing in mind the need for effective surgical therapy against reflux disease. The following options may be considered:
endo-bioptic postoperative monitoring, endoscopic ablation
The tested methods of endoscopic ablation are
- mono/bipolar electrocoagulation - argon plasma coagulation
- Photodynamic Therapy (PDT)
- Ultrasound aspiration - Endoscopic mucosectomy
These procedures can be employed in selected patients, above all enrolled in controlled
clinical trials. They often require repeated application, and are not without adverse events. Nevertheless, results are conflicting for a number of reasons, chief of which is the incomplete ablation of the metaplastic-dysplastic area.
When BE has taken on features that are seemingly or are indisputably precancerous, patients
must undergo a resective procedure, which may range from partial esophageal resection and recanalization with an interposed loop to total esophagectomy.
www.mattiolifp.it (Lectures - Esophageal Motility Disorders – 3)
Source: http://www.mattiolifp.it/lectures/lectures_15_eng.pdf
gpli.info
Bitoric Lens Design and Fitting Stephen P. Smith, B.S. Michigan College of Optometry at Ferris State University Abstract Bitoric contact lenses are a type of gas permeable (GP) contact lens with two different curves. One curve is on the front surface and the other curve is on the back surface. It is best utilized when corneal cylinder is equal to or exceeds 2.50 diopters. The two curves allow the "saddle
7170229
Open Science Journal of Clinical Medicine 2015; 3(6): 199-204 Published online November 2, 2015 (http://www.openscienceonline.com/journal/osjcm) ISSN: 2381-4748 (Print); ISSN: 2381-4756 (Online) Prevalence and Drug Susceptibility of Isolates of Urinary Tract Infections Among Febrile Under-Fives in Nsambya Hospital, Uganda Christine Ocokoru1, *, Robert Anguyo DDM Onzima2, Philip Govule3, Simon-Peter Katongole4