Designkolonien.dk

table of contents
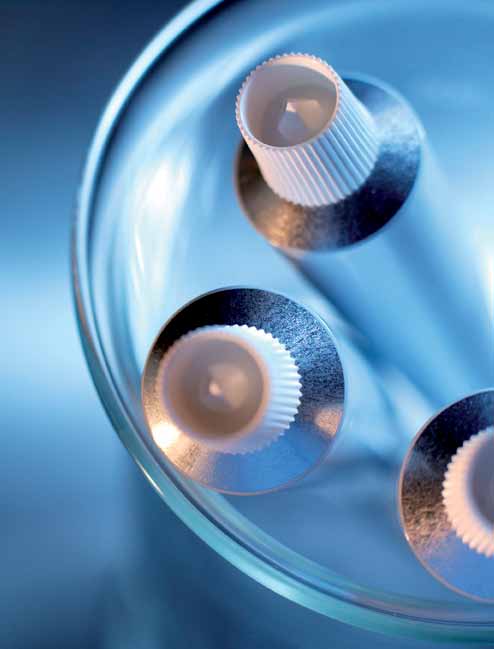
The Microlipid Crystallization Technology
astion pharma a/s
Active Substance
Manufacture and Stability
executive summary
Dermadexin™ Formulations
Dermadexin™ SD Cream
Dermadexin™ Scalp Solution
Dermadexin™ AD Cream
seborrhoeic dermatitis
Mechanism of Action
non-clinic al pharmacology studies
Seborrhoeic Dermatitis of The Face
Inhibition of Fatty Acid Amide Hydrolase (FAAH)
Seborrhoeic Dermatitis of The Scalp
Inhibition of NF-kB Transcription Response
Anti-inflammatory Effects in vivo 37
non-clinic al toxicology and safety studies 39
atopic dermatitis
Irritancy and Cytotoxicity
Acute Dermal Tolerance Test
28 Days Dermal Tolerance Test
Impaired Quality of Life
Sensitization Test
Phototoxicity Test
current treatment
Treatment of Seborrhoeic Dermatitis
clinic al studies
Treatment of Atopic Dermatitis
Trial-501 42 Trial-205
high unmet medic al need
Trial-301-01 50 Trial-502
IMS Survey Predicts Winner Position for Dermadexin™ SD Cream
patent protection
Target Product Profile
Product Characteristics
Astion Pharma is a privately held clinical-stage biopharmaceutical company.
Astion Pharma specializes in new products for large orphan diseases and autoimmune or inflammatory conditions with dermatological manifestations.
By combining highly innovative technologies with new scientific insights, Astion Pharma has set a new standard for safe and effective relief targeting unmet medical needs for both patients and physicians.
Astion Pharma's portfolio of cutting-edge topical products provides novel approaches to dermatological challenges in a variety of diseases.
dermatitis is a general term that describes inflammation of the skin
characterized by an array of symptoms including redness, pruritus (itching), scaling, crusting and in some cases small, clustered vesicles. It is estimated that dermatitis affects up to 20% of school children and 10% of adults. Dermadexin™
Therefore there are great unmet medical needs in several areas of dermatitis for
targets two of the most common types of dermatitis: seborrhoeic dermatitis and
safer, more effective topical treatment options providing lucrative niches for
atopic dermatitis, although Dermadexin™ is expected to have utility in a broader
novel treatments.
range of dermatoses. Seborrhoeic dermatitis and atopic dermatitis are both chronic diseases requiring continual treatment.
The global sales of topical corticosteroids, topical calceneurin inhibitors and
topical antifungal products excluding combination products reached a total in
Treatment of moderate to severe seborrhoeic dermatitis as well as atopic
2010 of USD 1,764 million. Alternative treatment options for dermatitis including
dermatitis poses unsolved problems due to the chronic nature of the diseases
emollients are excluded from this estimate, but their total sales are considered to
requiring effective and safe treatment that is suitable for long-term and recurrent
be of a significant magnitude.
administration. The current treatment options are either insufficient or associated with unwanted side effects. Moderate to severe seborrhoeic dermatitis of the
Dermadexin™ is a new topical treatment with the potential of meeting the
scalp and face as well as infantile atopic dermatitis represent specific areas with
above mentioned medical needs. due to a high efficacy without the risks
even more pronounced needs for alternative treatment options. The same is the
associated with current treatment options, dermadexin™ may be specifically
case with HIV-related seborrhoeic dermatitis which is characterized by more
targeted children and infants, as well as facial treatment where the prevalence of
extensive and severe symptoms and an increased prevalence ranging between
dermatitis is high, and the risk of side effects related to existing treatments is a
barrier for both clinicians and patients.



Dermadexin™, a New Treatment Targeting Dermatitis
All Dermadexin™ products are based on the proprietary pharmacologically active
Unique Mechanism of Actions addressing the pathophysiology of dermatitis
principle P3CGM with a unique dual Mechanism of Action (MoA):
at several essential levels providing a proprietary triple-action profile
Inhibition of fatty acid amide hydrolase (FAAH), which is induced
First effective topical treatment suitable for continual treatment of
in dermal inflammation.
chronic or recurring dermatitis
Inhibition of Nuclear Factor Kappa B (NF-kB) mediated inflammatory
Fast symptomatic onset of action
gene expression. This MoA gives rise to lower dermal levels of
High responder rate
inflammatory cytokines and chemokines.
Excellent safety profile
f o r m u l at i o n sCurrently three formulations of Dermadexin™ have been developed for different
target indications:
The Dermadexin™ products are based on Astion Pharma's Dual Anti-Neuro-
Dermadexin™ SD Cream indicated for seborrhoeic dermatitis.
inflammation Technology, which is related to the notion that the pathogenesis of
Dermadexin™ Scalp Solution indicated for dermatitis of the scalp.
dermatitis is generally associated with a combination of inflammatory and neuro-
and cradle cap (pityriasis capitis), including dandruff.
inflammatory mechanisms. Therefore the goal of the technology is to address both
Dermadexin™ AD Cream indicated for atopic dermsatitis.
aspects of the pathogenesis targeting inflammatory cells, like infiltrating leukocytes, as well as primary afferent sensory neuron peripheral endings. This is accomplished
Additional formulations may be developed for specific indications.
through the active principle P3GCM as described below.
Existing anti-inflammatory therapies like corticosteroids and calcineurin inhibitors
mainly address the contribution of inflammatory cells to the pathophysiology of
The excellent topical safety profile of dermadexin™ and the active principle
P3CGM has been demonstrated in a broad range of pre-clinical studies.
in humans the skin barrier repairing effects of dermadexin™ Sd Cream,
The Dermadexin™ emulsions further incorporate Astion Pharma's proprietary
Dermadexin™ Scalp Solution and Dermadexin™ AD Cream were convincingly
Micro Lipid Crystallization (MLC) technology which enables a physical restoration
demonstrated in a human model of irritant contact dermatitis induced by
of the disrupted skin barrier which plays an essential role in the pathophysiology of
application of Sodium Lauryl Sulphate (SLS) patches followed by 7 days of
treatment in 44 subjects. All dermadexin™ formulations displayed a marked and statistically significant
The triple-action profile of dermadexin™ is accomplished by the combination of
improving effect on skin barrier function measured as reduction of Trans
an innovative dual-action pharmacological principle and the additional MLC-based
Epidermal Water Loss (TEWL) and enhancement of skin hydration as compared
physical skin barrier repairing effect. This gives the dermadexin™ products a cutting
to an untreated control. no treatment related Adverse Events were observed.
edge efficacy with a strong commercial potential.


Interestingly topical corticosteroid and calcineurin inhibitors have no effect on
The dermadexin™ products can be ideally positioned for the pediatric market
skin barrier function (TEWL) in this type of study1.
targeting the high proportion of children with atopic or seborrhoeic dermatitis
Dermadexin™ SD Cream has been tested in two placebo-controlled multicenter
as well as infants with cradle cap.
clinical trials including a total of 436 patients with moderate to severe
Dermadexin™ SD Cream may be favorably positioned for use in the HIV
seborrhoeic dermatitis of the face with twice daily application of the test
positive or AIDS patients where the prevalence is high (30-83%) and the
products for a period of 21 days.
symptoms often more severe.
dermadexin™ Sd Cream displayed a marked and statistically significant effect
Another attractive niche for Dermadexin™ SD Cream is neurological patients
on the symptoms of facial seborrhoeic dermatitis with a fast onset of action
such as Parkinson disease and multiple sclerosis where both severity and
and an increasing effect over time, with significantly improved symptoms from
prevalence is reported to be high.
Day 7 and a very high responder rate (absence of symptoms) ranging between 48% and 69% after two weeks of treatment, increasing to between 60% and
ims survey predicts winner position for dermadexin™ sd cream
81% after three weeks of treatment in the two studies. The studies convincingly
The market potential of dermadexin™ Sd Cream was assessed in a survey
established the efficacy of the active compound P3CGm, and also indicated
conducted by IMS involving approximately 5% of the practicing dermatologists in
a major therapeutic contribution of the barrier repairing MLC technology as
denmark, who reviewed the clinical efficacy and safety data on dermadexin™
demonstrated by a high responder rate in the group treated with the Vehicle
MLC Cream (placebo).
Based on their evaluation of the data the dermatologists expressed a very
There were no safety issues encountered in these trials and no Serious Adverse
positive opinion on dermadexin™ Sd Cream. The efficacy and the excellent
Events were reported. dermadexin™ Sd Cream was well tolerated.
safety profile were perceived as the greatest advantages of the product. The
Dermadexin™ Scalp Solution has been tested in an open-label trial comprising
propensity of prescribing Dermadexin™ SD Cream was:
41 patients with scalp dermatitis with moderate to severe dandruff, who were
• 87% for new patients
treated twice daily for 21 days. Dermadexin™ Scalp Solution demonstrated
• 80% for switch patients due to insufficient efficacy of current treatment
a highly significant effect and fast onset of action on dandruff, with symptom
• 87% for switch patients due to side effects of current treatment
reduction already after 1 week. improvement in symptoms continued to increase
• 87% as supplement treatment
with treatment time, resulting in an overall decrease in total dandruff score of
overall this means that Dermadexin™ SD Cream stands to capture 13 new and 6
46% after three weeks. The product was well tolerated and no safety concerns
switch patients per dermatologist per month with an estimated Dynamic Capture
were raised.
IMS concludes that Dermadexin™ SD Cream is ideally positioned to obtain
The studies indicate that the Dermadexin™ products can be positioned as fast
a high market share.
acting, effective and safe treatment alternatives for dermatitis. Since the Dermadexin™ products are devoid of the safety concerns associated with
corticosteroids and calcineurin inhibitors, they may be positioned as the preferred
Dermadexin™ SD Cream is ready for launch in 2013. It is under registration in
treatment for continual use in seborrhoeic dermatitis and atopic dermatitis.
the EU and is expected to receive a marketing authorization first half 2013.
The same is the case with facial dermatitis, where seborrhoeic dermatitis is the
Dermadexin™ Scalp Solution is expected to be ready for launch in 2014.
most prevalent cause, since both corticosteroids and calcineurin inhibitors are
Dermadexin™ AD Cream is expected to be ready for launch late 2014
associated with strong restrictions regarding facial use.
or early 2015.

The active principle of Dermadexin™, P3CGM, is covered by patents expiring
in 2023. The patents are issued in most countries and pending in some.
dermatitis is a general term that describes inflammation of the skin characterized
Astion Pharma's Micro Lipid Crystallization Technology is patent pending with
by an array of symptoms including redness, pruritus (itching), scaling, crusting and
patent expiry in 2033.
in some cases small, clustered vesicles. Dermadexin™ targets two of the most common types of dermatitis: seborrhoeic dermatitis and atopic dermatitis, although
Dermadexin™ is expected to have utility in a broader range of dermatoses.
The manufacture of all Dermadexin™ formulations is fully scalable and
cost-effective.
The term seborrhoeic dermatitis relates to the distribution of skin lesions in areas rich in sebaceous glands, such as the scalp, face, and upper trunk. Seborrhoeic dermatitis is a chronic, relapsing form of dermatitis characterized by red lesions covered with greasy-looking yellowish scales. it may be accompanied by pruritus as well as stinging and burning sensations of the skin. Seborrhoeic dermatitis is most commonly located in the nasolabial folds, the eyebrows and glabella as well as the scalp. Lesions are less commonly located in the presternal and interscapular regions and the flexures. dandruff is a mild form of seborrhoeic dermatitis of the scalp with minimal inflammation. The diagnosis of seborrhoeic dermatitis is usually made clinically, based on the appearance and location of the lesions.
e p i d e m i o l o g iSeborrhoeic dermatitis has a biphasic incidence, occurring in infants between the ages of 2 weeks and 12 months and later, during adolescence and adulthood. The prevalence of clinically significant seborrhoeic dermatitis is approximately 1-3% in the general population of the USA, and 3-5% in young adults2. The actual prevalence is reported to much higher (12%) when mild cases are included3. Dandruff, the mildest form of seborrhoeic dermatitis, is present in an estimated 50% of the population4. Men are affected more frequently than women, and there is no preference for any specific ethnic group. Seborrhoeic dermatitis is specifically common in young children. It has been reported in 10% of infants below 6 years of age and above 50% when seborrhoeic dermatitis of the scalp is included. Almost
30% of infants below 1 year of age with seborrhoeic dermatitis of the scalp are reported to have moderate symptoms5. Infantile seborrhoeic dermatitis with
Seborrhoeic Dermatitis of the Scalp
symptoms related to other areas of the body such as behind the ears, in the
The mildest and most common form of scalp seborrhoeic dermatitis is dandruff,
creases of the neck, armpits and diaper area has been reported to be present in
also known as pityriasis sicca. dandruff is characterized by minimal, subclinical
as many as 44.5% of infants below 1 year of age5. In HIV positive patients there is
inflammation and a fine, white, easily visible diffuse scaliness. dandruff may be
an increased prevalence of seborrhoeic dermatitis ranging between 30% and 83%9.
asymptomatic or accompanied by mild pruritus. There are great variations in the
The prevalence has been estimated to be around 36% among patients with early
ease with which dandruff scales become detached and float among the hair shafts
is the mildest form of
HIV infection despite normal helper T-cell count2. An association with Parkinson's
or fall on the collar and shoulders. Dandruff is not serious from a medical standpoint,
seborrhoeic dermatitis
disease and other neurological disorders is frequently mentioned, and a prevalence
but the condition can result in psychological stress and embarrassment in social
as high as 35% of patients with Parkinson or other neurological diseases has been
situations. Treatment may be important for both physiological and psychological
reasons. More severe forms of seborrhoeic dermatitis of the scalp are characterized by
visible inflammation with redness and patches of greasy yellowish scales. The lesions
The role of malassezia species, characteristics of skin surface lipids and the
are mostly located on the sides of the scalp but may extend to the post-auricular
host's susceptibility in the pathogenesis of seborrhoeic dermatitis have long
areas and to the outer canal of the ear and external ear, sometimes with marked
been debated in the literature. There is limited direct evidence that Malassezia is
pruritus or infection.
implicated in the etiology of seborrhoeic dermatitis. Thus far, studies have failed to
demonstrate a higher density of malassezia on the skin of affected individuals or a
seborrhoeic dermatitis of
is characterized by red
relationship between the intensity of skin colonization and severity of seborrhoeic
Pityriasis capitis, known as cradle cap in the recently born, is infantile seborrhoeic
the scalp is characterized
patches and plaques
dermatitis, although some specific malassezia species have been detected more
dermatitis confined to the scalp. it is characterized by scaling of the scalp in the
by visible inflammation
with yellowish scales
frequently on affected skin than on normal skin. As appears to be the case with
absence of seborrhoeic dermatitis on areas of the skin other than the scalp. The
with redness and
other inflammatory dermatoses, individual susceptibilities and predispositions to
severity can be divided into minimal symptoms with fine, powdery white scaling,
patches of greasy scales.
inflammatory responses are likely to play a major role in determining the presence
mild symptoms with slightly larger flakes loosely adherent to the scalp or hair shafts,
of seborrhoeic dermatitis and its severity7,8.
moderate symptoms with thick flakes or scales, yellowish, and associated with underlying erythema, and severe symptoms with very thick scales, closely adherent
Seborrhoeic Dermatitis of the Face
to the scalp and hair, involving most of the scalp and associated with erythema.
Although seborrhoeic dermatitis may affect various areas of the body including the upper part of the trunk and the intertriginous areas, seborrhoeic dermatitis of the face is the most socially invalidating. Seborrhoeic dermatitis of the face is characterized by sharply demarcated red patches and plaques with greasy scales
often related to sebum-rich areas such as eyebrows, eyelids, nasolabial creases,
is infantile seborrhoeic
around the lips and behind the ears. The moustache and beard areas are frequently
dermatitis confined
involved in men with facial hair. The highly visible symptoms associated with
to the scalp.
seborrhoeic dermatitis of the face are easily mistaken for bad hygiene and even alcoholism, and seborrhoeic dermatitis of the face may result in both social and professional debilitation and may affect patient's quality of life negatively.
Seborrhoeic dermatitis is a common dermatosis in HIV-infected patients. The incidence and severity are closely related to the stage of HIV infection and inversely
Atopic dermatitis, also known as atopic eczema or Besnier's prurigo, is a chronic
correlated with the absolute CD4 and helper T-cell counts. Symptoms manifest
inflammatory skin disease with recurrent symptoms of pruritus, red, scaly, and
early in the course of the disease (CD4+ T-cell count range 450-550 cells/μL),
crusted lesions and papules which become excoriated and lichenified. The skin is
typically on the scalp, face and chest. Symptoms become more diffuse and severe
generally dry. Secondary infections are common, particularly in infants.
in patients with CD4 counts < 200 cells/μL, tend to be more extensive and severe,
The eruptions may occur anywhere on the skin, but the distribution usually varies
and involve unusual sites such as the extremities. Seborrhoeic dermatitis may regress
with age and in the infantile stage up to 2 years of age, the lesions are most often
with highly active antiretroviral therapy (HAART). However seborrhoeic dermatitis
located on the face and on the extensor surfaces. In the childhood stage from 2 to
may also be a cutaneous manifestation of the immune reconstitution inflammatory
12 years of age, the most commonly affected areas are the antecubital and popliteal
syndrome in patients on HAART. A small percentage of patients present with severe
fossae, the volar aspect of the wrists, ankles, and neck. in adults, the neck, antecubital
seborrhoeic dermatitis of the face and scalp as well as extensive involvement of the
fossae, and popliteal fossae are most commonly involved; other common sites
intertriginous areas spreading to the trunk and neck and potentially large areas of
are hands and feet, the face, wrists, and forearms. The skin is often lichenified and
excoriated. no specific laboratory findings or histological features define atopic dermatitis, and
the diagnosis is based on the clinical symptoms with pruritus and xerosis as the key
the neck and hands
are common sites of
atopic dermatitis.
popliteal fossae,
the feet, the face,
wrists, and forearms.
Atopic dermatitis is characterized by red, scaly, and crusted lesions and papules which become excoriated and lichenified.
Age of onset is typically between 2 and 6 months, and the vast majority of atopic dermatitis patients have an onset before age 5 years. There is a slightly higher
Treatment of Seborrhoeic Dermatitis
prevalence in females. It may occur in any race or geographic location, although
The mainstay of seborrhoeic dermatitis therapy is topical treatment. However,
there appears to be a higher incidence in urban areas and developed countries,
repeated or long-term treatment is necessary to control symptoms and prevent
especially western societies. Atopic dermatitis affects approximately 5-20% of
recurrence. Antifungals (ketoconazole and other imidazole derivatives) and low-
children and the prevalence of atopic dermatitis in the United States is around 11%.
and mid-potency corticosteroids, used alone or in combination, are the mainstay
The incidence of atopic dermatitis appears to be increasing10.
of therapy. Corticosteroids are preferred if there is a predominant inflammatory component. However, the two treatments are reported varying efficacy rates
ranging between 30-94%12, leaving a high proportion of non-responders or
The exact etiology of atopic dermatitis is unknown. The predominant hypothesis
insufficiently treated patients.
of the pathogenesis describes atopic dermatitis as a result of impaired epidermal
A wide selection of topical oTC products and various classes of prescription
pose a particular
barrier function due to structural and functional abnormalities in the skin. The
medication are used in a large variety of formulations of creams, foams, lotions,
stress to the family.
disease has a complex genetic basis with defects in factors important to skin barrier
solutions, shampoos and soaps based on:
function such as filaggrin and epidermal lipids. irritants, allergens and microbes that
antifungals such as ketoconazole
enter the skin through a defective skin barrier cause immune responses which may
contribute to the development of local inflammatory responses and the cutaneous
keratolytics (salicylic acid with or without sulfur)
findings of atopic dermatitis. A relation to type 1 igE-mediated hypersensitivity
calcineurin inhibitors (tacrolimus and pimecrolimus)
reactions is well established. However, 20-40% of individuals with atopic dermatitis
antiproliferatives based on coal tar and its derivatives
have a normal total or specific igE level. The inflammation of atopic dermatitis skin
other therapeutic options include metronidazole gel, tacalcitrol cream, topical
is chronic; even normal-looking, non-lesional skin of atopic dermatitis patients is
lithium succinate, selenium sulfide, zinc pyrithione and benzoyl peroxide.
immunobiologically anomalous with invisible inflammation and barrier defect11.
In severe cases or in cases that are refractory to topical treatment, oral itraconazole may be warranted.
i m pa i r e d q ua l i t y o f l i f eMany factors associated with atopic dermatitis seriously affect quality of life in atopic
dermatitis patients. Intense pruritus may impair sleep and disturb concentration
Depending on the severity of symptoms, treatment with an antifungal shampoo as
capacity during daytime activities. Sore fissures, visible chronic changes in the skin such
well as a variety of OTC anti-dandruff shampoos containing selenium sulfide, zinc
as lichenification and a tiresome daily routine of repeated applications of emollients
pyrithione, coal tar, or salicylic acid are used. For patients with itching and/or visible
for relapse prevention are all factors that may affect quality of life of patients negatively
inflammation, high potency corticosteroid solution, lotion, foam or shampoo are
and are particularly a burden to families when children are affected. Furthermore, the
recommended. oral antifungal treatment may also be used.
financial burden on patients and healthcare systems is significant.
s e b o r r h o e i c d e r m at i t i s o f t h e fac eA topical, low-potency corticosteroid formulation, a topical antifungal agent, or a combination of the two, are the most common treatments. For long-term control, application of a topical antifungal cream to the involved areas once a week or
ketoconazole shampoo may be used as a facial wash once weekly. Long-term (months to years) continuous use of even mild topical corticosteroids can result in permanent telangiectasia and atrophy and should be avoided. Men with moustaches and beards may require ketoconazole shampooing of the facial hair. Topical calcineurin inhibitors have been used for facial seborrhoeic dermatitis. However, they are not approved for treatment of seborrhoeic dermatitis and their use on sun-exposed skin areas is not recommended.
Topical Corticosteroids and Topical Antifungals
No randomized trials of antifungal agents or topical corticosteroids for the
Seborrhoeic dermatitis and atopic dermatitis are both chronic diseases requiring
treatment of seborrhoeic dermatitis in infants exist. Infantile seborrhoeic dermatitis
continual treatment for years. Topical corticosteroids are often used to obtain
of the scalp may be treated according to the severity. In the milder stages the
disease control in seborrhoeic dermatitis and is the mainstay of treatment in atopic
treatment includes application of an emollient to loosen the scales, or frequent
dermatitis, especially in the recurrent flare-ups. Heavy and prolonged use of topical
shampooing, followed by removal of scales with a soft brush. In persistent or more
corticosteroids is associated with risk of severe side effects such as skin atrophy,
extensive cases as well as in infantile seborrhoeic dermatitis in other areas than the
telangiectasia, striae, steroid-induced dermatoses, rosacea, acne exacerbation, and,
scalp, a short course of low-potency topical corticosteroids or topical antifungal
in some severe and rare cases, systemic effects such as hypothalamic-pituitary-
cream may be used.
adrenal axis suppression, growth retardation and ocular problems. Furthermore, the greatest penetration occurs with corticosteroid use on the groin and face, and the
face and skin folds are areas that are at high risk for corticosteroid induced atrophy.
Seborrhoeic dermatitis tends to be more diffuse and severe in HIV-positive patients
Compared with adults, children (especially infants) are at higher risk for the local
and may require a prolonged course of treatment. Initial management is the same as
and systemic side effects of topical corticosteroids. Moderate to severe seborrhoeic
for patients who are not HIV-positive. Severe cases or cases that are refractory to
dermatitis of the scalp is characterized by a marked inflammatory component and
topical treatment may be treated with a course of oral itraconazole.
high potency steroid formulations are used either alone or in combination with topical antifungals. However, a proportion of the patients have been reported to
Treatment of Atopic Dermatitis
respond insufficiently to steroid therapy13. Seborrhoeic dermatitis poses a similar
The goal of current atopic dermatitis therapy is to reduce the number and
therapeutic challenge with varying response rates to topical antifungal therapy13
severity of flare-ups. A multi-therapeutic approach that incorporates short-term
and an increased risk of skin atrophy even with mild corticosteroids14. Accordingly,
management of flares and longer-term strategies to prolong the time between flares
treatment of seborrhoeic dermatitis as well as atopic dermatitis with topical
is needed for proper disease control.
corticosteroids, especially in children, poses a great challenge and use of sufficiently
Topical anti-inflammatory treatment with corticosteroids combined with
potent corticosteroids and sufficient treatment duration is often avoided by the
maintenance of the skin barrier with emollients several times daily are the mainstay
patients for fear of side effects.
of disease treatment. Potent corticosteroids are generally avoided in skin folds and on the face. Maintenance therapy that includes intermittent use of a topical
Calcineurin Inhibitors
corticosteroid may help prevent relapse.
To avoid steroid side effects, the topical calcineurin inhibitors tacrolimus and pimecrolimus (Protopic® and Elidel®) have been used off-label for seborrhoeic
Systemic corticosteroids are reserved for use in patients with severe treatment-
dermatitis. These compounds are associated with a high frequency of undesirable
resistant atopic dermatitis and may improve the lesions, however, a disease flare-up
side effects including burning sensations, erythema, folliculitis and pruritus. In atopic
may occur when the treatment is stopped.
dermatitis they are approved only as second line therapy with great limitations, e.g. only short-term or intermittent therapy, no sun exposure and no use in children
The introduction of topical calcineurin inhibitors several years ago represented the
below 2 years of age. Since their approval, FDA has received reports of lymphoma
first new class of medication approved for the treatment of atopic dermatitis since
and skin cancer in children and adults treated with calcineurin inhibitors. FdA advises
the introduction of topical corticosteroids.
that Protopic® and Elidel® should be used only as labeled for patients who have failed treatment with other therapies.
Oral Antifungalsoral itraconazole is used in severe cases or when topical treatment fails. However, nausea and abdominal pain as well as skin rash are very frequent side effects (1-10%) and there are a number of contra-indications and drug-interactions associated with the compound.
„ ConClusion
high unmet medical need
Treatment of moderate to severe seborrhoeic dermatitis as well as atopic dermatitis poses unsolved problems due to the chronic nature of the diseases requiring effective and safe treatment that is suitable for long-term and recurrent treatment. The current treatment options are either insufficient or associated with unwanted side effects.
Moderate to severe seborrhoeic dermatitis of the scalp and face as well as infantile atopic dermatitis represent specific areas with even more pronounced needs for alternative treatment options, as does HIV-related seborrhoeic dermatitis which is characterized by more extensive and severe symptoms.
„My daughter is 7 years old and suffers from chronic atopic dermatitis with red itchy
Therefore there are great unmet medical needs in several areas of dermatitis for
patches on the neck and dry, irritated, red skin around the eyes. She is conscious of people
safer, more effective topical treatment options.
staring at her because of the red marks on her throat. So far, cortisone cream products
Dermadexin™ is a new topical treatment with the potential of meeting these
have been the only effective treatment but my fear of side effects is a great stress factor
medical needs.
in our daily life. Dermadexin™ is the first hormone-free cream that is able to remove the symptoms so well, and I am relieved that she can now get rid of the symptoms with a cream that I am not worried about".
Stella Maria Sørensen
Large Market with High Unmet Medical Needin the seborrhoeic dermatitis market there is a high unmet need as many patients are
on a global basis, the total number of patients with dermatological diseases was
either untreated or poorly treated with no structured management of their disease.
estimated to reach 418 million in 2011 of which 237 million were seeking treatment.
Furthermore, seborrhoeic dermatitis occurs with a very high incidence in patients with HIV infection, and the prevalence of seborrhoeic dermatitis is also increased in various
The market for dermatological products is divided into three main segments
neurological disorders, especially in parkinsonism15. By specifically addressing these
covering topical antifungals, topical corticosteroids, and products for treatment of
special populations, the market for dermadexin™ Sd Cream and dermadexin™
acne. The sector is highly diversified with overlapping segments of therapeutics,
Scalp Solution could be significantly enlarged.
aesthetics and skin care products. The market is served by multiple global, US and EU players of varying sizes including big-pharma and large specialty companies.
IMS Survey Predicts Winner Position for Dermadexin™ SD Cream
The majority of pharmaceutical products targeting seborrhoeic dermatitis and atopic
The market potential of dermadexin™ Sd Cream was assessed in a survey
dermatitis are the topical corticosteroids, the calcineurin inhibitors tacrolimus and
conducted by IMS involving approximately 5% of the practicing dermatologists
pimecrolimus (Protopic® and Elidel®), and topical antifungal products, containing e.g.
in denmark55. The investigation involved 15 dermatologists of which 8 worked in
ketoconazole. in the skin care sector the majority of the products are emollients
private clinics and 7 worked in (public) hospitals.
providing skin hydration and skin barrier improvement. due to the heavily
The dermatologists were interviewed to gain information on the Seborrhoeic
fragmented and diversified market, it is difficult to estimate the total market size
dermatitis market and main results were as follows:
where all segments of the market are included.
A dermatologist on average sees 57.9 seborrhoeic dermatitis patients per month.
A typical seborrhoeic dermatitis patient is 40 years of age. 87% are male and
The global sales of topical corticosteroids, topical calceneurin inhibitors and topical
13% are female.
antifungal products reached a total in 2010 of USD 1,764 million. Not all of the sales
The main proportion of the patients present disease of moderate severity.
were related to seborrhoeic dermatitis or atopic dermatitis. Combination products
The seborrhoeic dermatitis market is dynamic with 60% being new patients
of the above mentioned drugs as well as alternative treatment options including
and 40% switch patients.
emollients are excluded from the estimate, but their total sales are considered to be
Approximately 25% of all seborrhoeic dermatitis patients consult a physician.
of a significant magnitude.
The main proportion of these patients sees their GP only.
Side effects are considered the main problem with topical corticosteroids.
Global sales 2010,
Million USD
Based on this review of the clinical efficacy and safety data the dermatologists expressed a very positive opinion on Dermadexin™ SD Cream. The propensity of
Topical corticosteroids
prescribing Dermadexin™ SD Cream was: • 87% for new patients
Topical antifungals
• 80% for switch patients due to insufficient efficacy of current treatment
• 87% for switch patients due to side effects of current treatment • 87% as supplement treatment
overall this means that Dermadexin™ SD Cream stands to capture 13 new and 6
switch patients per dermatologist per month with an estimated Dynamic Capture Rate of 52.8%.
Global sales 2010 of topical corticosteroids, topical antifungals, Protopic® and Elidel® (Source: Evaluate Pharma).
other main results are summarized below:
75% of the dermatologists state that no professional guidance is needed for
initiation of treatment with Dermadexin™ SD Cream, mainly due to ease of use.
66% of the dermatologists see no disadvantages with Dermadexin™ SD Cream.
The greatest advantages are the product's safety and efficacy.
no specific patient profile is deemed most suitable for treatment with
Dermadexin™ SD Cream.
Considering that only 25% of the Seborrhoeic dermatitis patients consult a physician imS concludes that it is important also to keep GP's and pharmacists well informed
"I have suffered from atopic
about Dermadexin™ SD Cream.
dermatitis since I was a child. I have recurrent dermatitis on my hand with bouts of intense irritation, redness, sore chaps and small itching blisters.
Usually, it takes at least a week of treatment for the skin to begin to heal. I was surprised at how fast and
ConClusion
ims market survey
effectively Dermadexin™ worked on
In conclusion this market survey found that Dermadexin™ SD Cream is very well
all my symptoms in only two days! In
accepted by the dermatologists. The efficacy and the excellent safety profile are
addition Dermadexin™ kept the skin
perceived as the greatest advantages of the product.
pleasantly moisturized without an
The propensity of prescribing Dermadexin™ SD Cream was at least 80% for
oily or sticky feel.
both new patients and switch patients.
I have tried Dermadexin™ on several occasions and it works
IMS concludes that Dermadexin™ SD Cream is ideally positioned to obtain a
equally effective each time".
high market share.
Berith Haveløkke
Target Product Profile
Unique Mechanism of Actions addressing the pathophysiology of dermatitis
Further information about the mLC technology is confidential and only available
at several essential levels providing a proprietary triple-action profile
under Confidentiality Agreement.
First effective topical treatment suitable for continual treatment of chronic
or recurring dermatitis
The formulations based on the technology are called MLC emulsions, e.g. MLC
Fast symptomatic onset of action
Cream, MLC Lotion, etc. depending on the viscosity and appearance of the product.
High responder rate Excellent safety profile
Product CharacteristicsDermadexin™ is based on Astion Pharma's proprietary dual-action pharmacological principle P3CGm formulated in a topical emulsion with physical skin barrier repairing effects due to Astion Pharma's patent-pending Micro Lipid Crystallization Technology.
The Micro Lipid Crystallization TechnologyDermatitis is associated with an impaired barrier function of the stratum corneum, and the severity of the symptoms of dermatitis is correlated with the skin barrier
dysfunction measured as Trans-Epidermal Water Loss (TEWL)17,18.
Occlusion is known in dermatology to provide therapeutic effects besides enhancing the penetration of drug molecules. The same is the case for ointments which generally provide a stronger therapeutic effect than emulsions beyond the effect of
the administered drug molecule.
The establishment of a correlation between impaired skin barrier function
and dermal inflammation has provided a scientific basis for understanding the therapeutic benefits of occlusion. For Astion Pharma, it has also provided the basis for developing an optimized formulation technology providing the benefits of occlusion in the form of a cosmetically friendly emulsion.
Dermadexin™ is based on the Micro Lipid Crystallization (MLC) technology.
Astion Pharma's MLC technology repairs the dysfunctional barrier of stratum corneum, the outer
The MLC technology is the result of a research program aimed at developing a
layer of the epidermis.
therapeutically optimized basic emulsion formulation giving an optimized repair of the skin barrier.
A shelf-life of three years can be assigned based on stability trials according to ICH
The active principle in Dermadexin™ is Pyridine-3-Carboxamide Glyceryl
Monocaprylate (P3CGM). P3CGM has optimal formulation qualities including aqueous solubility and good
stability of solutions.
Dermadexin™ Scalp Solution is a light gel formulation developed for application to the scalp in relation to scalp dermatitis. It is supplied in bottles with an applicator
Manufacture and Stability
making it possible to apply the product directly through the hair to the scalp. The
product is intended for self-application twice daily by the patients.
Currently three formulations of Dermadexin™ have been developed for different
Stability trials according to ICH guidelines are ongoing.
target indications:
Dermadexin™ SD Cream indicated for seborrhoeic dermatitis
Dermadexin™ Scalp Solution indicated for dermatitis of the scalp and cradle
dermadexin™ Ad Cream has been developed specifically for application to skin
cap (pityriasis capitis), including dandruff
affected by atopic dermatitis. Due to the MLC cream formulation, the extra need
Dermadexin™ AD Cream indicated for atopic dermatitis
for barrier repair in atopic dermatitis is addressed, but without leaving the skin greasy and sticky. The cream should be applied twice daily on the affected areas by
All three products are Medical Devices Class 3 as they have a medicinal substance
the patients or their parents (in the case of children). The product is an oil-in-water
incorporated. This classification enables medical claims similar to OTC drugs, but
emulsion based upon Astion Pharma's patent-pending Micro Lipid Crystallization
with a less rigid control of marketing. reimbursement is considered possible in many
(MLC) technology. Stability trials according to ICH guidelines are ongoing.
jurisdictions. Manufacture of all three Dermadexin™ products employs standard manufacturing techniques of semi-solids. only pharmaceutical grade components
Mechanism of Action (MoA)
are utilized (Ph. Eur.) and all products are manufactured according to Good
Manufacturing Practice (GMP) and ISo13485.
it is now well-established that the peripheral nerves in the skin interplay with dermal cells and infiltrating leukocytes in the pathophysiology of dermatitis, even
Additional formulations may be developed for specific indications.
with different underlying pathogeneses19. neurotransmitters like substance P and endocannabinoids play a central role in dermal inflammation together with the
traditional inflammatory mediators such as cytokines, chemokines, eicosanoids, kinins
dermadexin™ Sd Cream has been developed specifically for application to facial
skin. The cream is intended for self-application twice daily by the patients. The product may also be applied to the scalp in relation to severe seborrhoeic dermatitis
Dermadexin™ is based on the proprietary pharmacologically active principle
of the scalp where the barrier-repairing effects exerted by the MLC technology are
P3CGM with a unique dual mechanism of action (MoA):
advantageous as compared to the Dermadexin™ Scalp Solution.
Inhibition of fatty acid amide hydrolase (FAAH), which is induced in
The product is an oil-in-water emulsion based on Astion Pharma's patent-pending
dermal inflammation. FAAH is responsible for the breakdown of anti-pruritic
MLC technology. The manufacture employs standard manufacturing techniques of
and anti-inflammatory dermal endocannabinoids. This moA gives rise to
semi-solids, and commercial scale batches have been successfully produced.
enhanced dermal endocannabinoid levels which exert anti-inflammatory effects via cannabinoid receptors on peripheral sensory nerve endings and various inflammatory cells including leukocytes and keratinocytes.
Inhibition of Nuclear Factor Kappa B (NF-kB) mediated inflammatory
rather than being stored in intracellular vesicles, endocannabinoids like AEA are
gene expression. This moA gives rise to lower dermal levels of inflammatory
formed on demand from membrane phospholipids, and their concentration is
cytokines and chemokines.
regulated by a series of biosynthetic and catabolizing enzymes20.
the endoc annabinoid system of the skin and inhibition of faah
AEA is degraded to arachidonic acid and ethanolamine by the enzyme fatty acid
The endocannabinoids are lipids that act as endogenous ligands for the cannabinoid
amide hydrolase (FAAH), which is a membrane-bound serine hydrolase found
receptors CB1 and CB2. The N-acyl ethanolamines are a prominent class of
in mitochondrial and plasma membranes. The endocannabinoids are produced
endocannabinoids, and n-arachidonoyl ethanolamine (AEA) is considered the
by various cells, including cells of the immune system, the peripheral nervous
most important.
system (PnS), the central nervous system (CnS) and cells of the skin, including keratinocytes21. Inhibition of FAAH is a promising strategy to increase the level of EAE and related endocannabinoids in various tissues including the skin.
Endocannabinoids have also been shown to activate other receptors, including peroxisome proliferator-activated receptors (PPARs) and the transient receptor potential vanilloid-1 (TRPV-1) channel, which may contribute to their bioactivity.
The role of the endocannabinoid system in skin physiology is under intense investigation. Cannabinoid receptors are expressed throughout the skin. Keratinocytes and melanocytes are known to express CB1, CB222,23, whilst sebocytes express CB2. With regard to resident skin cells, AEA displays anti-inflammatory effects and has been shown to reduce TNF-a- induced IL-8 and monocyte chemotactic protein 1 (MCP-1) release from keratinocytes24. in addition to cannabinoid receptor expression in resident skin cells, it has also long been established that many subpopulations of immune cells express CB1 and CB2, including B-cells, NK-cells, monocytes, neutrophils, CD8+ T-cells, CD4+ T-cells, mast cells and dendritic cells25,26. There is a large body of evidence supporting the fact that endocannabinoids like AEA can provide anti-inflammatory effects. EAE has been shown to reduce the release of TNF-a and IFN-g by CD4+ and CD8+ T-cells, and IL-17 by Th17 cells,
and to suppress the proliferation of all subtypes of T-cells. All of these effects are
mediated by CB2. However, both CB1 and CB2 are known to affect T-cell signaling27.
of particular relevance for several types of dermatitis, endocannabinoids control not only human skin mast cell activation, but also their maturation from resident
The MoA of P3CGM has been demonstrated in vitro in an enzyme inhibition assay
progenitor cells in situ via CB1 stimulation28.
related to FAAH and a cellular model of NF-kB transcription response. The potential
All in all, inhibition of FAAH represents a promising MoA to enhance the level of
of P3CGm to inhibit mediators of dermal inflammation has been tested in vivo with
EAE and related endocannabinoids in the management of dermatitis.
a well-established cutaneous inflammatory model, the tetradecanoylphorbol acetate-induced inflammation model.
Inhibition of Fatty Acid Amide Hydrolase (FAAH)
transcription factor that amplifies the expression of a range of inflammatory genes,
The inhibitory effect of P3CGM on FAAH was tested in an in vitro enzyme assay.
in all inflammatory cells, including cytokines (TnF, iL-1, iL-6), chemokines (monocyte
it proved to have a significant inhibitory effect on the FAAH function measured as
chemotactic protein-1, MCP-1; IL-8), cell adhesion molecules (intercellular adhesion
inhibition of AEA breakdown32,33. P3CGM was effective at concentrations within
molecule-1, ICAM-1; vascular cell adhesion molecule-1,VCAM-1), and proteases29,
a relevant therapeutic range (see figure below).
which all contribute to the pathophysiology and symptoms of dermatitis.
Multiple bacterial and fungal factors stimulate NF-kB activation leading to pro-
inflammatory gene expression30. Colonization with Malassezia spp. is implicated in
the pathogenesis of seborrhoeic dermatitis and colonization with Staphylococcus
aureus is implicated in the pathogenesis of atopic dermatitis31.
In conclusion, inhibition of NF-kB transcription response is a promising therapeutic
strategy in the management of dermatitis.
Concentration (µM)
Dose-response curve of the inhibitory effect of P3CGM on FAAH activity33.
Inhibition of NF-kB Transcription Response
Anti-Inflammatory Effects in
The effect of P3CGM on NF-kB transcription response was tested in vitro in
the Tetradecanoylphorbol Acetate Mouse Model
Human T-lymphocytic Jurkat cells, transfected with a response element-lacZ reporter
Significant dose-related anti-inflammatory effects of P3CGm have been
in which transcription of the B-galactosidase gene is directed by the binding
demonstrated in the tetradecanoylphorbol acetate-induced ear oedema model of
site for the NF-kB transcription factor34,35. P3CGM displayed a dose-dependent
dermal inflammation. This is a well-established anti-inflammatory model in mice36
inhibition within a relevant therapeutic range (see figure below) and was devoid of
associated with NF-kB dependent inflammatory gene expression37,38 and the release
cytotoxicity at the tested concentrations.
of a broad range of inflammatory mediators including cytokines and chemokines. The model is therefore a suitable mechanistic in vivo model for the evaluation of the topical efficacy of P3CGm. The study has been conducted with BALB/c mice39-44 and SPF NMRI mice45. P3CGM displayed a dose-dependent inhibition of ear oedema
that was comparable to the strong corticosteroid betamethasone-17-valerate in a
commercial preparation, Celestonvalerat® 0.1% Cream (see figure below).
Concentration (µM)
Dose-response curve of the inhibitory effect of P3CGM on NF-kB transcription response34.
The figure shows the inflammation expressed as relative ear oedema (%). Level of statistical
significance (all groups versus vehicle): p<0.01, Mann-Whitney Rank sum test (n=10).
ConClusion
non-clinical pharmacology studies
The Dermadexin™ formulations have been based on a composition of ingredients
P3CGM displays a dual mechanism of action characterized by inhibition of FAAH
with a well-known safety profile and without any toxicological issues. All three
and NF-kB dependent inflammatory gene expression giving rise to a combination
products contain the active medicinal substance P3CGM, and upon administration
of enhanced levels of anti-inflammatory endocannabinoids and suppression of
to the skin the formulations release free pyridine-3-carboxamide and free glyceryl
the release of inflammatory mediators.
The anti-inflammatory efficacy of topical administration of P3CGM in clinically
Pyridine-3-carboxamide is an endogenous substance and a precursor to
relevant doses has convincingly been demonstrated in a well-established model
intracellular NAD of vital importance to cellular metabolic processes. Pyridine-
of cutaneous inflammation.
3-carboxamide is administered intravenously in the treatment of pellagra. The toxicology and the safety of the substance is well established, and it is considered safe and without health concerns even in relatively high systemic doses.
Glyceryl monocaprylate is an endogenous substance formed extensively in
the intestines during the digestion of medium-chain-triglycerides from a variety of vegetable sources. on this basis there is a widespread systemic exposure to the substance in the general population, and the substance is considered safe and without health concerns even in relatively high systemic doses.
For further evaluation of the local tolerance of P3CGM in the concentration used in the Dermadexin™ formulations, Astion Pharma has conducted tests for dermal tolerance, sensitizing potential and contact photo toxicity of P3CGM with very positive results.
Irritancy and Cytotoxicity in Reconstituted Human Epidermis In VitroDermadexin™ SD Cream (4.5% P3CGM) was tested for cytotoxicity and irritancy in a well-established in vitro model of human epidermis56. The cream was applied to the surface of in vitro reconstituted human epidermis, and cytotoxicity, as indicated by decreased metabolic activity of keratinocytes, was measured. Leakage and/or secretion of interleukin-1a from keratinocytes were measured as a predictive indicator of skin irritation. The cell culture supernatant from the study was therefore collected and the content of interleukin-1a determined by ELiSA.
Dermadexin™ SD Cream was found not to be cytotoxic to reconstituted human
dated July 30th, 1996. The test item was a 4.5% (w/v) aqueous solution of P3CGM
epidermis, and the cream did not give rise to increased interleulin-1a release and
which was applied to 11 albino guinea pigs of dunkin-Hartley strain. Five additional
was concluded to be non-irritative.
animals served as negative control and were not subjected to the test item48. After induction of the animals, followed by an 18 days rest phase, the challenge
Acute Dermal Tolerance Test
phase was conducted under occlusive conditions for 24 hours. Macroscopic
P3CGm was tested for dermal tolerance in a single dose test in new Zealand
readings of erythema and edema were performed 24 and 48 hours after removal
rabbits according to the OECd guideline no 404 (adopted 24 April 2002) and the
of occlusive dressing.
test method B.4 of the directive no 2004/73/EC.
4.5% P3CGM (w/v) dissolved in 2% aqueous propylene glycol was applied under
No macroscopic cutaneous reactions attributable to allergy were recorded during
4 hours semi-occlusive dressing to undamaged skin areas of three new Zealand
the study, and P3CGM was concluded to be non-sensitizing.
rabbits. A dose of 0.5 mL was applied to the right flank of each animal and the left flank served as the control. Skin reactions of erythema and edema were assessed 1,
Phototoxicity Test
24, 48 and 72 hours after removal of the patch.
In order to assess the phototoxic potential of P3CGM, a phototoxicity test was performed in 11 female albino dunkin-Hartley guinea pigs49. Test item was 4.5%
No cutaneous reactions (erythema and edema) were observed at any time point,
P3CGM dissolved in 2% aqueous propylene glycol.
and P3CGm was classified as a non-irritant46.
doses of 0.5 mL of the test item were applied to the right flank of 11 guinea-pigs 30 to 35 minutes before irradiation with 7000 mJ/cm2 of UV-A light and 150 mJ/cm2
28 Days Dermal Tolerance Test
UV-B light. Cutaneous reactions of erythema and edema were assessed 24 and 48
Dermadexin™ SD Cream (4.5% P3CGM) was tested for repeated-dose dermal
hours after the irradiation.
tolerance in new Zealand rabbits47. This test was performed in accordance with EmA note for Guidance on non-clinical Local Tolerance Testing (CPmP/
no phototoxic reactions were observed, and P3CGm was classified as non-phototoxic.
SWP/2145/00) and according to GLP.
The study was performed in male SPF nZW rabbits, 1.8-2.0 kg body weight. Six rabbits were dosed with 2 g cream to areas of shaved, non-abraded skin, approximately 10 x 15 cm in size. Single daily applications for three weeks were performed.
„ ConClusion
non-clinical toxicology and safety studies
Dermadexin™ and P3CGM are concluded to have a good dermal safety profile. P3CGM and Dermadexin™ were found to be non-irritating in the acute local
The study concluded that Dermadexin™ SD Cream did not cause dermal irritation
tolerance test and in the 28 day local tolerance test. No sensitising effects were
when applied topically for three weeks and can be classified as having a good dermal
observed, and P3CGM was classified as non-phototoxic.
tolerance after repeated application.
All in all, the Dermadexin™ formulations are concluded to be safe and without
Sensitization Test
safety concerns both locally on the skin and systemically.
The sensitizing potential of P3CGm was tested in a model according to OECd guideline no 406 dated July 17th, 1992 and the method B.6 of the EEC no 96/54
days 2, 3, 4 and 8: Clinical examination, TEWL measurement and skin hydration measurement.
The preclinical and early clinical development of Dermadexin™ was carried out in
The subjects applied the investigational products twice daily to the treatment zones
cooperation with Professor Dr. Hans Christian Wulf, Lead Physician of the largest
dermatological clinic in Scandinavia at Copenhagen University Hospital.
TEWL was measured using an Aquaflux® TEWL instrument and skin hydration was
An extensive clinical test program has demonstrated the efficacy and safety of the
measured using a Corneometer. The primary endpoint was TEWL on zones treated
Dermadexin™ products. The test program included four trials:
with investigational product as compared to the non-treated SLS-patched zone.
One trial of the skin barrier repairing effect of all three products in
healthy volonteers, Trial-501.
Two efficacy trials on dermadexin™ Sd Cream, Trial-205 and Trial-301-01.
Treatment with dermadexin™ Sd Cream resulted in a significantly lower TEWL
One efficacy trial on dermadexin™ Scalp Solution, Trial-502.
indicating an improved skin barrier function compared to the non-treated SLS-patched zone from Day 3 and at the following time points (Day 3 p=0.0150; Day
Trial-501: Test of Skin Barrier
4 p=0.0014; Day 7 p=0.0216; Day 8 p=0.0207). At Day 8, the Dermadexin™ SD
Repairing Effect in Irritant Contact Dermatitis
Cream had induced a 20% better skin barrier function compared to the non-treated
The skin barrier repairing effect of dermadexin™ Sd Cream, dermadexin™ Scalp
SLS-patched zone.
Solution and dermadexin™ Ad Cream was investigated by Trans Epidermal Water Loss (TEWL) measurements on skin with impaired barrier function in a model
of induced irritant contact dermatitis obtained by application of Sodium Lauryl
Treatment with this product resulted in a significantly lower TEWL compared to
Sulphate (SLS) patches under occlusive conditions for 24 hours50.
the non-treated SLS-patched zone from Day 3 and at the following time points (Day 3 p=0.0258; Day 4 p=0.0003; Day 7 p=0.0078; Day 8 p=0.0054). At Day 8,
The trial was a single-center, open-label intra-individual trial. 44 subjects were
dermadexin™ Scalp Solution had induced a 24% better skin barrier function as
included. The subjects had each forearm divided into three zones the size of a
compared to the non-treated SLS-patched zone.
standard patch. one zone was left untreated and was not exposed to SLS. Another zone was SLS-treated but otherwise left untreated. The remaining four zones were
SLS-treated and treated with the investigational products. Study procedures were as
Treatment with this product resulted in a significantly lower TEWL compared to
the non-treated SLS-patched zone from SLS Day 2 and onward (Day 2 p=0.0497; Day 3 p=0.0304; Day 4 p=0.0006; Day 7 p=0.0145; Day 8 p=0.0117). At Day
8, dermadexin™ Ad Cream had induced a 22% better skin barrier function as
A patch with 0.5% SLS was applied to five of the six zones.
compared to the non-treated SLS-patched zone.
interestingly topical corticosteroid and calcineurin inhibitors have no effect on skin
The SLS patches were removed and the zones examined. TEWL measurement and
barrier function (TEWL) in this type of study51.
skin hydration measurements were performed two hours after SLS patch removal.
The TEWL measurements at the different time points are presented in the figure below:
„ ConClusion
clinical trial-501
The Dermadexin™ products significantly improved the skin barrier function in irritant contact dermatitis induced by SLS exposure by reducing the TEWL. Moreover, the products had significant hydrating effects by normalizing the skin hydration after the SLS exposure. No safety concerns were raised in this trial.
The demonstrated effect is highly relevant in the treatment of various types of dermatitis where the disrupted barrier is an important part of the pathogenesis. Interestingly, topical corticosteroid and calcineurin inhibitors have no effect on skin barrier function (TEWL) in this type of study
TEWL in treated and non-treated zones.
data from the skin hydration measurements were confirmatory of the TEWL data. Significant hydrating effects of the three products were shown, and the xerosis induced by the SLS exposure returned to normal at the finalization of the study whereas the untreated zone remained very dry.
All three products were well tolerated and a total of 30 Adverse Events were reported. 23 Adverse Events related to the study procedures were reported by 16 subjects. However, none of these events were considered related to the investigational products but associated to SLS exposure. 7 Adverse Events experienced by seven patients were considered unrelated to the study procedures or the investigational products. no Serious Adverse Events were reported.
Efficacy DataAn indication of fast onset of action was observed in the proportion of patients
Two clinical trials were performed:
with an oSS score of 1 or 0 (responders) treated with Dermadexin™ SD Cream
A proof-of-concept study: Trial-205
already after 7 days of treatment (37.5% of responders vs. 20% in the group treated
A larger confirmatory study: Trial-301-01
with Vehicle mLC Cream) with a significantly higher responder rate on Day 14 (68.8% vs. 26.7%; p=0.03).
TRIAL-205 Trial-205 was a proof-of-concept study investigating efficacy and safety of
After three weeks of treatment, the proportion of patients with an OSS score of
Dermadexin™ SD Cream in patients with moderate to severe seborrhoeic
1 or 0 (responders) was 81.3% in the Dermadexin™ SD Cream group and 46.7%
dermatitis of the face52.
in the placebo group (ITT population). Despite the large difference in responder rate between the groups, it was not statistically significant (p=0.0659), which was
Dermadexin™ SD Cream was compared to an identical MLC emulsion formulation
attributed to a decreased statistical power related to the sample size.
without P3CGM (placebo), in the following referred to as ‘Vehicle MLC Cream'.
The relatively high responder rate in the Vehicle MLC Cream group is attributed to the barrier repairing effects provided by Astion Pharma's proprietary MLC
The study was conducted as a multicenter, parallel-group, double-blind study with
three centers in France on patients with a clinical diagnosis of facial seborrhoeic dermatitis. Patients with moderate to severe facial seborrhoeic dermatitis were
included in the trial. The investigational products were applied twice daily by the
patients for 21 consecutive days. 16 patients received Dermadexin™ SD Cream and
seborrhoeic dermatitis
15 patients received Vehicle MLC Cream.
of the face in a patient
before and after 7
on Day 0, Day 7, Day 14 and Day 21 the patients' erythema and scaling were
days of treatment with
assessed by the investigator and the pruritus assessed by the patient. A four-point
DermadexinTM SD Cream
symptom scale was used as follows: 0: Absent, 1: Mild, 2: Moderate, 3: Severe. At each visit the investigator calculated the Overall Severity Score (OSS) defined as the sum of the erythema and scaling scores.
The primary efficacy endpoint was the proportion of patients with an OSS of 0 or 1 after three weeks of treatment. The secondary endpoints included the proportion
Responder rates over time.
of patients with clearance of symptoms (oSS=0), erythema score, scaling score, pruritus score, patients' global assessment and safety.
The difference in total symptom clearance between the two groups was significant
All other secondary efficacy endpoints, i.e. scaling, erythema and pruritus, were
after three weeks (37.5% vs. 6.7%; p=0.003).
positive and in support of a good effect of Dermadexin™ SD Cream on the symptoms of Seborrhoeic Dermatitis of the face.
Safety DataThe investigational products were well tolerated, and no safety concerns were raised. There were no Serious Adverse Events reported during the study. 14 subjects experienced a total of 29 Adverse Events that were either mild (25) or moderate (4) in intensity. No patients stopped treatment or left the trial.
Proportion of patients with total clearance of their symptoms.
„ ConClusion
clinical trial-205
Dermadexin™ SD Cream displayed a marked effect on the symptoms of facial
There was also a significant improvement at all three time points when considering
seborrhoeic dermatitis compared to Vehicle MLC Cream with a fast onset of
the difference between the total ooS scores (Day 7: p=0.0319; Day 14: p=0.0069;
action and an increasing effect over time until three weeks of treatment, with
day 21: p=0.0168).
significantly improved symptoms from Day 7 and a very high responder rate of almost 70% after 2 weeks of treatment, increasing to more than 80% after three weeks of treatment. The study convincingly established the efficacy of the active compound, P3CGM, and also indicated a major therapeutic contribution of the barrier repairing MLC technology as demonstrated by the high responder rate in the group treated with the Vehicle MLC Cream.
Dermadexin™ SD Cream was well tolerated.
OSS score over time.
rate in the group treated with MCL Control Cream indicated a large contribution of the MLC technology to the therapeutic effect of Dermadexin™ SD Cream.
Trial-301-01 was a larger clinical trial investigating efficacy and safety of Dermadexin™ SD Cream in patients with moderate to severe seborrhoeic dermatitis of the face53.
Dermadexin™ SD Cream was compared to a similar product without P3CGM (placebo), in the following referred to as ‘Vehicle MLC Cream'.
The investigational products were applied twice daily by the patients for 21 consecutive days.
The trial was a randomized, double-blind, parallel-group, multi-center clinical trial with centers in Canada, denmark, Finland, France, Germany, Sweden and UK. 302 patients received Dermadexin™ SD Cream, and 103 received Vehicle MLC Cream.
Frequency of responders over time.
Efficacy assessment and parameters were as in Trial-205. The primary endpoint was again the proportion of patients having an oSS of 0 or 1 after three weeks of treatment. The secondary endpoints included proportion of patients with clearance
The difference in total symptom clearance between the two groups was significant
of symptoms (oSS=0), erythema score, scaling score, pruritus score, patients' global
already after 14 days of treatment (18.7% vs. 4.9%; p=0.002) and after 21 days the
assessment and safety.
effect was even more pronounced (30.0% vs. 13.6%; p=0.002).
Efficacy DataAn indication of fast onset of action was observed in patients treated with Dermadexin™ SD Cream already after 7 days of treatment (25.4% responders vs. 15.5% in the group treated with Vehicle mLC Cream) with a significantly higher responder rate on Day 14 (47.8% vs. 25.2%; p<0.001). A highly significant difference was observed after three weeks of treatment where a responder rate of 59.6% was seen in the group treated with Dermadexin™ SD Cream vs. 41.7% in in the group treated with Vehicle MLC Cream (P=0.001, ITT population). Trial-301-01 therefore met the primary endpoint. The high responder
Proportion of patients with clearance of symptoms.
When comparing the effect of the Dermadexin™ SD Cream with the effect of
the Vehicle mLC cream after three weeks of treatment correlated with the disease
no Serious Adverse Events were reported in the trial. A total of 112 patients
severity at baseline, there was a significantly better effect of the dermadexin™
reported one or more Adverse Events, most of them mild, and there was no
SD Cream in the more severe cases while the effect of the Vehicle MLC Cream
statistical difference in the number of Adverse Events reported in the two treatment
decreased with disease severity at baseline, indicating that the active substance
groups. overall, Dermadexin™ SD Cream was well tolerated.
P3CGM played an increasing role with increasing disease severity:
oSS=5 at baseline: 64.0% responders in Dermadexin™ SD Cream
group vs. 33.3% responders in the vehicle MCL Cream group (p=0.006).
oSS=6 at baseline: 45.7% responders in the Dermadexin™ SD Cream group
vs. 0.0% responders in the Vehicle MCL Cream group (p=0.008).
„ ConClusion
clinical trial-301-01
The results of the large Trial-301-01 confirmed the results of Trial-205 in the treatment of moderate to severe facial seborrhoeic dermatitis. A fast onset of action and increasing effect over time until three weeks of treatment was seen.
The primary endpoint was met with a pronounced and highly significant effect of Dermadexin™ Cream at the end of the treatment.
An important contribution of the barrier-repairing effect of the MLC technology to the therapeutic effect of Dermadexin™ SD Cream was indicated by a marked and increasing effect over time in the Vehicle MLC Cream group. There was a significantly better effect of the Dermadexin™ SD Cream compared to the Vehicle MLC Cream in the more severe cases and the effect of the Vehicle MLC Cream decreased with disease severity at baseline, indicating that the active substance P3CGM played an increasing role with increasing disease severity. Overall, the Dermadexin™ SD Cream proved convincingly efficacious in the
Proportion of responders correlated with disease severity at baseline.
treatment of moderate to severe seborrhoeic dermatitis with a fast onset of action and an advantageous safety profile. Dermadexin™ Cream was well
All other secondary efficacy endpoints on e.g. scaling, erythema and pruritus
tolerated and there were no Serious Adverse Events reported during the conduct
were positive and in support of good effects of Dermadexin™ SD Cream on the
of the trial.
symptoms of Seborrhoeic Dermatitis of the face.
Trial-502 Trial-502 evaluated the effect of Dermadexin™ Scalp Solution in patients with scalp dermatitis moderate to severe dandruff 54.
The trial was a single-center, open-label trial involving 41 patients treated with Dermadexin™ Scalp Solution for 21 consecutive days. The patients treated themselves twice daily with Dermadexin™ Scalp Solution directly on the affected areas of the scalp.
Assessment of the anti-dandruff effect on days 7, 14 and 21 was intra-individual with the evaluation carried out in comparison to the baseline data. Efficacy parameters included non-adherent dandruff, adherent dandruff and erythema. All three
Total dandruff score over time.
parameters were assessed on a 6 point scale (0-5) by the investigator. Total dandruff score was defined as the sum of the scores for adherent and non-adherent dandruff. Pruritus was assessed by the patients on a 4 point scale (0-3).
A significant decrease from baseline in erythema score was seen after three weeks
of treatment (1.3 vs. 0.9; p=0.0223). Decreases in erythema scores were also
A fast onset of action was demonstrated, and all dandruff parameters significantly
observed at Day 7 and Day 14.
decreased after 1 week of treatment compared to baseline (p<0.0001). A significant difference of 0.9 units in the total dandruff score (6.8 vs. 5.9; p<0.001) was found. Furthermore, there was a significant decrease in the score of pruritus rated by the subjects (1.27 vs. 0.80; p<0.0001).
Improvements of dandruff and pruritus were further increased after 14 and 21 days of treatment (p<0.0001 for all parameters) and after three weeks of treatment an average improvement of 46% of the total dandruff score was observed (6.8 at baseline vs. 3.7 after 21 days; p<0.001). The product also had a good effect on pruritus. At baseline 70.7% of the patients reported pruritus but after three weeks of treatment (d21) this proportion was reduced to 36.6%
Erythema score over time.
no Serious Adverse Events were reported in the trial. Five subjects experienced seven mild Adverse Events, possibly related to the investigational product. These
The active principle of Dermadexin™, P3CGM, is covered by patents expiring in
events were mild in intensity and disappeared within one hour after application.
2023. The patents are issued in most countries and pending in some.
11 subjects experienced 15 Adverse Events which were considered unrelated to the protocol or investigational product.
Astion Pharma's Micro Lipid Crystallization Technology is patent pending with patent expiry in 2033.
overall, the product was well tolerated and no safety concerns were raised.
The dermadaxin™ formulations meet the requirements of the European medical Device regulations because:
ConClusion
1) They are intended for treating conditions in human beings, and;
Dermadexin™ Scalp Solution demonstrated a highly significant fast onset of
2) They have a primary Mode of Action which is physical/mechanical in
action in dandruff, the main symptom of moderate to severe scalp dermatitis,
nature due to Astion Pharma's MLC technology.
with symptom reduction already after 1 week. Improvement in symptoms
The Dermadaxin™ formulations incorporate a medicinal substance with an ancillary
continued to increase with treatment time, resulting in an overall decrease in total
effect and are thus Class 3 Medical Devices according to current legislation.
dandruff score of 46% after three weeks.
Overall, the Dermadexin™ Scalp Dermatitis Cream proved efficaceous in the
dermadexin™ Sd Cream is currently awaiting the CE-mark and a design dossier
treatment of scalp dermatitis with a fast onset of action and an advantageous
has been compiled and submitted to the relevant authorities (notified Body). The
safety profile.
part of the Design Dossier related to the incorporated medicinal substance has been submitted for approval by a Competent Authority within the EU.
Astion Pharma is ISo13485-certified, which is a requirement for manufacturing of Class 3 Medical Devices.
The Dermadexin™ products are currently not approved in other territories, and no submissions for marketing approvals have been submitted outside the EU.
Engel K, et al. J Eur Acad dermatol Venereol. 2008 Apr;22(4):447-50.
25. Galiegue S et al. Eur J Biochem. 1995;232:54-61.
rook's Textbook Of dermatology. 7th edition. Volume One,
26. Samson MT et al. J Immunol. 2003 May 15;170(10):4953-62.
17. Blackwell Science.
27. Cencioni MT et al. PLoS one. 2010 Jan 14;5(1):e8688.
Bangsgaard n. månedsskrift for praktisk lægegerning 2011 Mar;89:199.
28. Sugawara K et al. J Allergy Clin Immunol. 2012 Mar;129(3):726-38.
Manuel F and Ranganathan S. Int J Trichology 2011 Jan-Jun;3(1):3-6.
29. Bell S et al. Cell Signal. 2003 Jan;15(1):1-7.
Foley P et al. Arch Dermatol. 2003;139(3):318-322.
30. Lin YT. Clin Rev Allergy Immunol. 2007 Dec;33(3):167-77.
Scheinfeld NS. Medscape Journal Article 2005 Jan (online).
31. Pivarcsi A. et al. Curr Immunol Rev 2005;1:29-42.
32. Study AB16840.
Kim GK. J Clin Aesthet Dermatol. 2009 Nov;2(11):14-17.
33. Study AB17420.
Sasseville D. UpToDate 2011 June; (online).
34. Study AB16841.
35. Study AB17421.
36. rao TS et al. inflammation. 1993 dec;17(6):723-41.
Chatzikokkinou P. Acta dermatovenerol Croat 2008;16(4):226-230.
37. Afaq F et al. Toxicol Appl Pharmacol. 2004 Mar 15;195(3):361-9.
10. Weston WL. UpToDate 2012 January; (online).
38. Park JH et al. mutat res. 2008 Jul 3;642(1-2):68-73.
39. Study AT3023.
40. Study AT3026.
=atopic+dermatitis&selectedTitle=2 150.
41. Study AT3029.
11. Wollenberg A and Ehmann Lm. Ann dermatol. 2012 Aug;24(3):253-60.
42. Study AT3038.
12. Cohen S. Arch Dis Child 2004;89:288-89.
43. Study AT3043.
13. Ramirez RG and Dorton D. J Dermatol Treat. 1993;3(3):135.
44. Study AT3044.
14. Elewski BE. Journal of drugs in dermatology 2006;5(7):646-50.
45. Study AT3065.
15. Binder RL and Jonelis FJ. Arch Dermatol. 1983 Jun;119(6):473-5.
46. PharmaScan Study no: iC-OCdE-PH-05/0280.
16. Thomsen SF and Agner T. rationel Farmakoterapi 2010 (8):1-4.
47. BioAdvice Study No. 2152.
17. Hon KL et al. Am J Clin Dermatol. 2008;9(1):45-50.
48. PharmaScan Study No: SMK-PH-05/0294.
18. Addor FA et al. Int J Dermatol. 2012 Jun;51(6):672-6.
49. PharmaScan Study No: PTC-PH-05/0280.
19. mikami n et al. Crit rev immunol. 2012;32(4):307-20.
50. Astion Pharma Trial 501.
20. Hansen HS, et al. J Neuroendocrinol. 2008 May;20 Suppl 1:94-9.
51. Engel K et al. J Eur Acad dermatol Venereol. 2008 Apr;22(4):447-50.
21. Pucci m et al. Eur J dermatol 2011;21 Suppl. 2:29-34.
52. Astion Pharma Trial-205.
22. Pucci M et al. J Biol Chem. 2012 May 4;287(19):15466-78.
53. Astion Pharma Trial-301-01.
23. Toth BI et al. J Invest Dermatol. 2011 May;131(5):1095-104.
54. Astion Pharma Trial 502.
24. Leonti M et al. Biochem Pharmacol. 2010 Jun 15;79(12):1815-26.
10279-01 Radar Success Finder. 2010.
56. Study AT3182.
company informationastion pharma a/s
addressLiterbuen 11dK-2740 Skovlundedenmar k
tel. +45 4444 1544
email [email protected]
Web www.astion.com
Source: http://designkolonien.dk/DOWNLOAD/Dermadexin_download.pdf
lactacyd.com.co
18 al 20 de febrero de 2009 3er Foro Latinoamericano sobre Higiene íntima Femenina Actualización en patología vulvar y tracto urinario Del 18 al 20 de febrero de 2009 se realizó en la Ciudad de Varadero, Cuba, el 3er Foro Latinoamericano sobre Higiene Íntima Femenina. En esta ocasión, el evento estuvo dirigido a la actualización en patología vulvar y tracto urinario. Diversos especialistas de países latinoamericanos comentaron sus experiencias con el objetivo de actualizar al médico ginecólogo en la etiología, el diagnóstico y el tratamiento de las distintas afecciones vulvares y vaginales. Se contó con la presencia del Dr. Jaime Piquero Casals (Venezuela), quien habló sobre los aspectos clínicos de las vulvitis frecuentes y de la problemática de la infección vulvar por HPV. Las distrofias vulvares, especialmente el liquen escleroso y el liquen simple crónico, fueron comentadas por la Dra. Lina María Figueira (Venezuela). El Dr. Wel ington Aguirre (Ecuador) se refirió a los trastornos genitourinarios en la menopausia y su abordaje farmacológico. El Dr. Alejandro Paradas (República Dominicana) disertó acerca de la protección y la prevención de las infecciones vaginales. Finalmente, el Dr. Santiago Herrán (Colombia) expuso los resultados del primer estudio epidemiológico latinoamericano sobre hábitos de higiene íntima femenina y su relación con la vaginosis bacteriana en mujeres latinoamericanas, inquietud que tuvo su origen en el foro predecesor realizado en 2008 en Panamá.Surge como principal conclusión de este encuentro que la adopción de hábitos de higiene íntima femenina adecuados es una medida esencial en la prevención de afecciones genitourinarias tanto de origen infeccioso como no infeccioso.
environment.fudan.edu.cn
23 September, Fudan University, China International Symposium on Innovation in Sustainability: Air, Water and Materials Registered charity number 207890 with the world's leading chemistry community and join our 51,000 members globally Registered charity number: 207890 041536 China Membership_advert_A4_Chinese.indd 1 11/06/2015 09:08:31 Welcome address from the Royal Society of Chemistry