Untitled
REFRACTIVE SURGERY FEATURE STORYPRK and CXL in Patients
The combined procedure strengthens the cornea and regularizes the anterior surface.
BY MIRKO R. JANKOV II, MD, PHD; SLADJANA DELEVIC, MD; VESNA JOVANOVIC, MD, MS;
EFEKAN COSKUNSEVEN, MD; AND SLOBODAN GOLUBOVIC, MD, PHD
Irregular astigmatism can occur naturally or due to maintain the existing unfavorable biomechanical status trauma or surgery. Although technological and surgi- within the underlying stroma. In cases in which the irregular cal skill improvements in modern refractive surgery astigmatism is progressive, such as keratoconus, pellucid have led to excellent outcomes, the occurrence of marginal degeneration, and laser-induced iatrogenic ectasia, corneal irregularities postoperatively has been described.1 the corneal stroma is structurally weakened, and some of Highly irregular corneas can also originate from corneal these conditions may worsen following tissue ablation pro- scars derived from injuries, previous inflammation, or sur- gical procedures such as penetrating keratoplasty, radial Hence, to correct irregular astigmatism due to a biome- keratotomy, or arcuate cuts.2 chanically unstable cornea, a coadjuvant intervention such Another more challenging cause of corneal irregulari- as CXL should be considered to potentially stabilize the ty is ectatic disease.3 Some of these diseases arise natu- cornea while regularizing the corneal surface. rally, such as keratoconus and pellucid marginal degen-eration, and others are surgically induced, such as iatro- genic ectasia after laser surgery. Common among all CXL with riboflavin and ultraviolet-A (UV-A) light admin- ectatic disesases is progression due to a previous struc- istration is a technique that strengthens corneal tissue by tural weakening and thinning of the corneal stroma.
using riboflavin as a photosensitizer and UV-A to increase Patients complain of decreased vision, glare, photopho- the formation of intra- and interfibrillar covalent bonds bia and monocular diplopia.
through photosensitized oxidation.7 This technique is simi- Once the patient is unable to use rigid contact lenses, there lar to photopolymerization in polymers, and through it bio- are few surgical alternatives for correction. Expectations are mechanical stabilization of the cornea is achieved.
limited, and consequences may be unpredictable, both The key indication for CXL is to inhibit the progression of anatomically and functionally. In recent years, however, tech- corneal ectasias, such as keratoconus and pellucid marginal nological advances have led to two approaches: (1) corneal degeneration.8 CXL may also be effective in the treatment regularization based either on intrastromal corneal ring and prophylaxis of iatrogenic keratectasia resulting from implantation4 or limited topography-guided excimer laser LASIK.9 Beyond keratectasia, the technique can also be used customized ablation treatment (T-CAT)5 or (2) corneal stabi- in treating corneal melting conditions or infectious keratitis; lization using corneal collagen crosslinking (CXL).6 CXL strengthens the collagenolytic cornea while the UV-A Vision-correcting methods, such as laser treatment or irradiation sterilizes the infectious agent.10 intrastromal corneal ring implantation, attempt to regular- In the presence of 0.1% riboflavin acting as a photosensi- ize the front surface of the irregular cornea; however, they tizer, using an irradiance of 3 mW/cm2 of UV-A, as much as 32 I CATARACT & REFRACTIVE SURGERY TODAY EUROPE I OCTOBER 2009

REFRACTIVE SURGERY FEATURE STORY
95% of UV-A light is absorbed within the cornea.7Keratocyte apoptosis in the anterior corneal stroma to adepth of approximately 300 µm has been described, and aclear demarcation line between treated and untreatedcornea has been shown.11 Confocal microscopy studies alsoshow that repopulation of keratocytes is already visible 1month after treatment, and preoperative quantity and qual-ity in terms of functional morphology is achieved within 6months after treatment.12
T-CAT can achieve the goal of regularizing a distorted
cornea by significantly reducing high astigmatism.13
Figure 1. Treatment in progress; the cornea is soaked with
However, additional thinning of the already biomechanically
riboflavin and irradiated by the UV lamp.
challenged cornea may be counterproductive, with the riskof worsening corneal biomechanical stability due to further
inflammatory response and thus haze.
thinning after tissue ablation.
It is probable that the ablation rate on a cornea previously
Our surface ablation protocol is intended to reduce
treated with CXL would not be significantly altered in com-
postoperative pain and haze by minimizing the inflamma-
parison with that of the normal cornea. Even if it were differ-
tion reaction and minimizing increased sensitivity to UV-
ent, one would expect slight overcorrection, as the corneal
radiation injury.14 A 50-µm phototherapeutic keratecto-
collagen seems to be more compact in the first 6 months
my (PTK) at a 6.5-mm optical zone is used to remove the
after the CXL treatment. This is the reason we recommend
epithelium. Afterward, PRK with a minimal amount of tis-
that approximately 80% of the refraction (mainly cylinder)
sue removal (less than 50 µm) and optical zones as small
should be treated at an optical zone of 6 or 5.5 mm and a
as 5.5 mm is planned, aiming at maximum cylinder reduc-
transitional zone of 9 mm. One must also be sure not to
tion with minimal tissue removal to regularize the cornea.
surpass 50 µm of ablation depth at the deepest point.5
A single procedure, meaning an immediate sequence
of T-CAT transepithelial PRK and CXL, would be without
The key indications for use of this combined treatment
doubt more comfortable for both the patient and the
method are to regularize distorted corneal optics, halt the
surgeon. It is also easy to predict what the ablation out-
progression of keratoconus, and achieve lasting visual reha-
come would be, as one would be applying the laser to
bilitation. The goal is to synergize the effects of the two
virgin corneal tissue and there would be no need to
treatments. When planning combined sequential treat-
remove the crosslinked cornea. Moreover, there would be
ments, two main questions arise: (1) Which is the correct
less chance of PRK-induced scarring because the CXL
treatment order? (2) What is the right time interval
would induce apoptosis of the keratocytes and thus
between the treatments?
eliminate the agents that would theoretically produce
Regarding treatment sequence, concerns include whether
the cornea pretreated with CXL will react to T-CAT PRK the
However, corneal thickness becomes crucial in this case,
expected way, or whether the effect will be altered because
as an excimer laser treatment, even with stromal removal
it is being applied now to a stiffer cornea. On the other
limited to 50 µm, would additionally decrease the thickness
hand, will CXL be safe when applied over a cornea addition-
of an already thin cornea. To avoid the danger of endothelial
ally thinned by laser ablation?
damage, we recommend intraoperative ultrasound contact
If the plan is to first stabilize the cornea with CXL and
pachymetry immediately after T-CAT PRK and the use of
later apply limited T-CAT transepithelial PRK, one should
hypotonic riboflavin to expand the corneal thickness
wait at least 6 months in between procedures, as by this
throughout the procedure.
time the cornea will have completed the repopulation and
Moreover, CXL alone additionally changes the corneal
deactivation of keratocytes.12 It is essential to wait past this
shape by flattening it up to 2.00 D of the keratometry value
period, as it is likely that a cornea with still activated kerato-
over several years,6,8,15-18 meaning that a planned laser treat-
cytes during the first few months after CXL will react exces-
ment may be enhanced or even overflattened by additional
sively to excimer laser injury, resulting in an exaggerated
CXL treatments later on. This is another reason why we rec-
OCTOBER 2009 I CATARACT & REFRACTIVE SURGERY TODAY EUROPE I 33
REFRACTIVE SURGERY FEATURE STORY
defining a horizontal line, are placed with help of a slit lamp,using the light slit rotated into horizontal position. Beforesetting the marks, the patient's head tilt is adjusted so thatboth pupils are level (ie, positioned along the same horizon-tal line). The second drop of anesthetic is applied beforeintroduction of the eye speculum under the laser micro-scope. Chilled balanced salt solution is applied to the corneafor 60 seconds to slow corneal metabolism.
Ablation using the Allegretto Wave excimer laser
(WaveLight AG, Erlangen, Germany) is aligned onto thecenter of the pupil. A 50-µm PTK at a 6.5-mm opticalzone is applied to remove the epithelium uniformly.
Immediately afterward, T-CAT PRK ablation of up to 50µm depth at a 5.5- to 6-mm optical zone is applied, fol-lowed by irrigation with chilled balanced salt solution foranother 60 seconds.
Immediately after the transepithelial PRK and before CXL
treatment, ultrasound pachymetry is performed over thedeepithelialized cornea at approximately the thinnest pointto ensure a minimal corneal thickness of 400 µm. Riboflavin
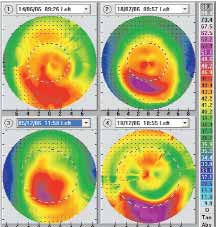
Figure 2. Serial computerized corneal topography: at the
0.1% solution in 20% dextran (Peschkemed, Huenenberg,
time of examination, right after the removal of the rigid gas
Switzerland) is applied to the cornea every 3 minutes for 30
permeable contact lens (upper left); 1 month after contact
minutes. For corneas thinner than the safety limit, 30-
lens removal and the day of the CXL treatment (upper right);
minute instillation of hypotonic riboflavin 0.1% without
5 months after CXL treatment and the day of T-CAT transep-
dextran is applied until the cornea has reached at least 3
ithelial PRK (lower left); 2 weeks after the T-CAT transepithe-
80 µm thickness.
lial PRK treatment (lower right).
UV-A irradiation is performed using an optical system
(Koehler illumination) consisting of an array of seven UV-A
ommend treating the spherical component of the refraction
diodes with a potentiometer in series to allow regulation of
only partially and planning 80% of the cylinder correction.
voltage (UV-X; Peschkemed; Figure 1). Irradiance is per-formed for 30 minutes at 3 mW/cm2, corresponding to a
surface dose of 5.4 J/cm2. During treatment, riboflavin solu-
The procedure is conducted under sterile conditions in
tion and topical anesthetic proparacaine 0.5% are applied
an operating theater. Our surface ablation protocol aims
every 2 to 3 minutes to saturate the cornea with riboflavin
to reduce postoperative pain and haze by minimizing the
inflammation reaction and minimizing increased sensibility
After the treatment, dexamethasone with tobramycin
to UV-radiation injury. Vitamin C for protection against UV
ointment (Tobradex; Alcon Laboratories, Inc.) and topical
damage and haze formation18 and omega-3 fatty acids for
ofloxacin 0.3% (Floxal; Bausch & Lomb, Rochester, New
improvement of the tear film, both 1 g daily, are given for
York) are applied. A bandage contact lens is fitted to the
3 days before surgery and 6 months after the surgery. NSAID
corneal surface and removed after reepithelialization, typi-
treatment with ibuprofen (Brufen; Galenika, Belgrade,
cally on day 3 postoperative. The patient is given the topical
Serbia) 600 mg four times daily is started 2 days before sur-
steroid dexamethasone phosphate 0.1% (Maxidex; Alcon-
gery and continued through day 3 postoperative. A pred-
Couvreur, Belgium) four times daily, with gradual decrease
nisolone 50 mg (Pronison; Galenika) tablet is given orally as
of dosage over the following 2 months.
a single dose 30 minutes before the surgery. Diclofenac 0.1%(Voltaren; Novartis, Basel, Switzerland) and ciprofloxacin
0.3% (Marocen; Hemofarm, Vrsac, Serbia) eye drops are
Case 1: CXL first, T-CAT transepithelial PRK later. A 36-
administered 15, 10, and 5 minutes before surgery.
year-old woman who had worn rigid gas permeable contact
The first drop of anesthetic, proparacaine 0.5% (Alcaine;
lenses for 20 years reported to our service because of con-
Alcon Laboratories, Inc., Fort Worth, Texas) is applied dur-
tact-lens intolerance. Her BCVA with contact lenses was 1.0
ing the preparation of the eyelids and the surgical field.
in both eyes. Papillary reaction was observed on the upper
Scleral (perilimbal) marks at the 3- and 9-o'clock positions,
tarsal conjunctiva, with red eye and corneal punctate ero-
34 I CATARACT & REFRACTIVE SURGERY TODAY EUROPE I OCTOBER 2009
REFRACTIVE SURGERY FEATURE STORY
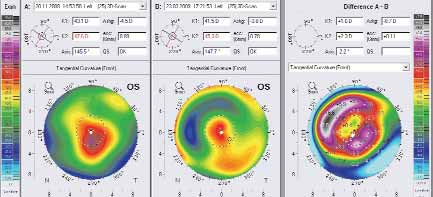
Figure 3. Computerized corneal Scheimpflug tomography: (left) before and (center) after the combined T-CAT transepithelial
PRK-CXL treatment. Difference map is at right.
sions. At the examination, her BCVA in the right eye was 0.6
ago. She had been treated at another center with succes-
with refraction of -2.00 -1.50 X 90º and in the left was 0.4
sive CXL and implantation of Ferrara Rings (Ferrara
with refraction of -2.50 -1.75 X 100º. Ultrasound pachyme-
Ophthalmics, Belo Horizonte, Brazil) 1 year ago in her right
try was 493 and 474 µm in the right and left eyes respective-
eye. This resulted in UCVA in the right of 0.3 and BCVA of
ly, and her computerized corneal topography can be seen in
0.6 with refraction of -0.75 D sphere, which did not
improve with pinhole. Her left eye had UCVA of 0.1 and
After 1 month of contact lens abstinence, a typical pat-
BCVA of 0.3+ with refraction of -1.75 -1.75 X 150º, achiev-
tern of keratoconus could be appreciated on corneal topog-
ing 0.6 with pinhole.
raphy. At that time bilateral CXL treatment was performed.
In her left eye, we performed T-CAT transepithelial
Almost 5 months after the CXL treatment, BCVA in the
PRK followed by immediate application of CXL. Three
right eye was 1.0+ with refraction of -3.25 -1.00 X 90º and in
months after treatment, her UCVA was 0.5 and BCVA
the left eye 0.6 with -3.50 -1.50 X 100º. As the patient was
was 0.6 with refraction of -0.50 -1.25 X 155º. Topography
contact-lens intolerant, T-CAT transepithelial PRK was per-
can be seen in Figure 3.
formed in the left eye. After 2 weeks, UCVA reached 0.8, andBCVA was 1.0+ with refraction of -0.75 -0.50 X 90º.
CONCLUSIONS
Case 2: T-CAT transepithelial PRK followed immedi-
Treatment of keratoconus with a combination of
ately by CXL. A 26-year-old woman with a 10-year history
CXL and excimer laser topography-guided transepithe-
of keratoconus became contact-lens intolerant 1.5 years
lial PRK is possible. The aim of this combined treat-ment is regularization of the cornea and significant
reduction of irregular astigmatism rather than com-
• In patients with irregular astigmatism due to keratoconus,
plete elimination of spherical refractive error. Thus, an
treatments such as PRK or corneal rings can regularize the
ablation depth of up to 50 µm with small optical
front surface of the cornea, but they do not address the
zones (6 or 5.5 mm) and larger transition zones (9
underlying unfavorable biomechanical status of the stroma.
mm) is recommended.
• A coadjuvant intervention with CXL can potentially stabi-
With sequential CXL followed by T-CAT transepithe-
lize the cornea and regularize the corneal surface.
lial PRK, an interval of at least 6 months should beallowed between the two treatments. Coadjuvant T-
• With combined CXL and topography-guided
CAT transepithelial PRK immediately followed by CXL
transepithelial PRK, Dr. Jankov and colleagues aim to
is more comfortable for the patients; however, it is
regularize the cornea and reduce irregular astigmatism, rather
suitable for thicker corneas or earlier stages of kerato-
than completely eliminating spherical refractive error.
36 I CATARACT & REFRACTIVE SURGERY TODAY EUROPE I OCTOBER 2009


Mirko R. Jankov II, MD, PhD, practices at
LaserFocus Centre for Eye Microsurgery, Belgrade,Serbia. Dr. Jankov states that he is a paid consult-ant to WaveLight Laser Technologie AG. He maybe reached at e-mail: [email protected].
Sladjana Delevic, MD, is with Oculus Specialized Hospital for
Ophthalmology, Belgrade, Serbia. Dr. Delevic states that shehas no financial interests in the products or companies men-tioned.
Vesna Jovanovic, MD, MS, practices at LaserFocus Centre for
Eye Microsurgery, Belgrade, Serbia. Dr. Jovanovic states thatshe has no financial interests in the products or companiesmentioned.
Efekan Coskunseven, MD, is with the Dunya Eye
Hospital, Istanbul, Turkey. Dr. Coskunseven statesthat he has no financial interests in the products orcompanies mentioned.
Slobodan Golubovic, MD, PhD, is with Oculus
Specialized Hospital for Ophthalmology, Belgrade, Serbia. Dr.
Golubovic states that he has no financial interests in the prod-ucts or companies mentioned.
1. Hersh PS, Fry KL, Bishop DS. Incidence and associations of retreatment after LASIK. Ophthal-mology. 2003;110(4):748-754.
2. Lindstrom RL. The surgical correction of astigmatism: a clinician's perspective. Refract CornealSurg. 1990;6(6):441-454.
3. Kennedy RH, Bourne WM, Dyer JA. A 48-year clinical and epidemiologic study of keratoconus.
Am J Ophthalmol. 1986;101(3):267-273.
4. Coskunseven E, Kymionis GD, Tsiklis NS, et al. One-year results of intrastromal corneal ring seg-ment implantation (KeraRing) using femtosecond laser in patients with keratoconus. Am J Ophthal-mol. 2008;145(5):775–779.
5. Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: atemporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26(7):891-895. 6. Coskunseven E, Jankov MR, Hafezi F. Contralateral eye study of corneal collagen cross-linkingwith riboflavin and UVA irradiation in patients with keratoconus. J Refract Surg. 2009;25(4):371-376.
7. Spoerl E, Huhle M, Seiler T. Induction of cross-links in corneal tissue. Exp Eye Res.
1998;66(1):97–103.
8. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A–induced collagen crosslinking for thetreatment of keratoconus. Am J Ophthalmol. 2003;135(5):620–627.
9. Hafezi F, Wiltfang, R, Kanellopoulos J, Seiler T. Corneal collagen crosslinking with riboflavin andultraviolet A to treat induced keratectasia after laser in situ keratomileusis. J Cat Refract Surg.
2007;33(12):2035-2040.
10. Schnitzler E, Spoerl E, Seiler T. Irradiation of cornea with ultraviolet light and riboflavin administra-tion as a new treatment for erosive corneal processes, preliminary results in four patients. [Article inGerman] Klin Monatsbl Augenheilkd. 2000;217(3):190-3.
11. Seiler T, Hafezi F. Corneal cross-linking-induced stromal demarcation line. Cornea.
2006;25(9):1057-1059. 12. Mazzotta C, Balestrazzi A, Traversi C, et al. Treatment of progressive keratoconus by riboflavin-UVA-induced cross-linking of corneal collagen: ultrastructural analysis by Heidelberg Retinal Tomo-graph II in vivo confocal microscopy in humans. Cornea. 2007;26(4):390-397.
13. Jankov MR, Panagopoulou SI, Tsiklis NS, Hajitanasis GC, Aslanides IM, Pallikaris IG. Topogra-phy-guided treatment of irregular astigmatism with the WaveLight excimer laser. J Refract Surg.
2006;22(4):335-344.
14. Stojanovic A, Wang L, Jankov MR, Nitter TA, Wang Q. Wavefront optimized versus custom-Qtreatments in surface ablation for myopic astigmatism with the WaveLight Allegretto Laser. J RefractSurg. 2008;24(8):779-789.
15. Jankov MR, Hafezi F, Beko M, et al. Corneal cross-linking for the treatment of keratoconus: pre-liminary results. [Article in Portuguese] Arq Bras Oftalmol. 2008;71(6):813-818.
16. Agrawal VB. Corneal collagen cross-linking with riboflavin and ultraviolet – a light for kerato-conus: results in Indian eyes. Indian J Ophthalmol. 2009;57(2):111-114.
17. Wittig-Silva C, Whiting M, Lamoureux E, Lindsay RG, Sullivan LJ, Snibson GR. A randomizedcontrolled trial of corneal collagen cross-linking in progressive keratoconus: preliminary results. JRefract Surg. 2008;24(7):S720-725.
18. Vinciguerra P, Albe E, Trazza S, et al. Refractive, topographic, tomographic, and aberrometricanalysis of keratoconic eyes undergoing corneal cross-linking. Ophthalmology. 2009;116(3):369-378.
19. Stojanovic A, Ringvold A, Nitter T. Ascorbate prophylaxis for corneal haze after photorefractivekeratectomy. J Refract Surg. 2003;19:338-343.
Source: http://www.spectrumsurgical.com.au/downloads/mirko_1_10.pdf
09.informationbulletin.october.pub
THE INFORMER INFORMATION BULLETIN OF THE ISLAND GOVERNMENT OF ST. EUSTATIUS Volume 1, Issue 2 OCTOBER ISSUE , 2009 Dutch civil servants supporting transition St. Eustatius– The Dutch civil servants of the Ministry of Traffic and Water Management visited their local counter-parts on Tuesday September 8th 2009, to discuss Air Traffic Control, Air Space and Airport Development after the tran-sition. One of the topics was the condi-tion of the servicing of the landing strip. This point needs priority in the master plan. Another issue which has the at-tention is the airlift to and from the is-land. A market scan for airlift is in the making. During their visit they met with, Planning Officer, Mr Maldwyn Timber, of Planning, Mr. Ellis Schmidt, Airport Manager, and the Executive Council. The Airdrome will remain a responsibility of the Island Government. They discussed navigation aids, airspace and airport developments . The agree-
A prospective study of salvage high-intensity focused ultrasound for locally radiorecurrent prostate cancer: early results
Scandinavian Journal of Urology and Nephrology, 2010; Early Online, 1–5 A prospective study of salvage high-intensity focused ultrasound forlocally radiorecurrent prostate cancer: Early results VIKTOR BERGE1, EDUARD BACO1 & STEINAR JOHAN KARLSEN1,2 1Department of Urology, Oslo University Hospital, Aker, Oslo, Norway, and 2Faculty of Medicine, University of Oslo,Norway