Chapter 10: supportive care
CHAPTER 10: SUPPORTIVE CARELung cancer and its treatment can cause many symptoms that may interfere with your ability to
live as you normally would. Health care providers often refer to this interference as a reduction in quality of life or QOL. Supportive care is a term that refers to treatments used to eliminate or reduce symptoms that interfere with your quality of life. The aim of supportive care is to provide you with the best quality of life possible, so that you are able to participate in your treatment and do the things that bring you pleasure and happiness. More simply, the goals of supportive care are to maximize comfort and eliminate suffering. Palliative care is very similar to supportive care. The difference between supportive and palliative care is the situation in which the treatment is given. Supportive care refers to symptom management while a person is receiving treatment to potentially cure his or her disease or extend life. Palliative care is symptom management and special care of a person whose disease cannot be cured. While there is a distinction between these two terms, there is a great deal of overlap between both the goals and methods used in these two types of care. Supportive and palliative care share the common goal of providing the best possible quality of life by maximizing your comfort and minimizing suffering. Palliative care often encompasses the treatment and support of both people who are sick and their loved ones. For simplicity, we use the term supportive care in this chapter. However, keep in mind that many supportive care treatments are also used for palliative care. Many side effects of lung cancer treatment are common and well known. Often health care providers use medicines or other therapies to prevent these side effects from occurring, sparing you from experiencing these discomforts. Other symptoms and side effects are treated as they arise. In general, symptoms can be most successfully controlled if they are treated as soon as possible. Early treatment not only reduces suffering but also helps preserve the body's ability to carry out its normal functions. Each person's experience with lung cancer is different. Supportive care plans are individualized to meet the unique experience of each person. Many supportive care measures are available to help people with lung cancer. Supportive care is most effective when you work in partnership with your health care team. Discuss your symptoms openly and honestly with your providers. If a recommended treatment is not helping the problem for which it was given, do not be afraid to tell your provider. Your health care providers are able to help you only if they are aware of what you are experiencing. Your job is to keep your health care providers informed about your symptoms. Their job is to ensure that your needs are met. Together, you and your providers will be able to develop a supportive care plan that works well for you. A large number of symptoms are discussed in this chapter because lung cancer is capable of causing a wide variety of symptoms. Do not be alarmed by the number of symptoms discussed. The symptoms described are just a list of possibilities. Some of the symptoms are common, while others are relatively rare. We have tried to include a wide variety of potential symptoms to address the experiences of as many people as possible. It is likely you will never experience many of the symptoms described here. It is also possible you will experience some symptoms not included here. The important thing to keep in mind is that all symptoms are important and should be discussed with your health care providers. Your doctors and nurses want to help you feel your best but can only accomplish that goal with your help. SIGNS & SYMPTOMS ASSOCIATED WITH LUNG CANCER
People living with lung cancer often experience different symptoms over the course of their illness. When you are examined by your health care provider, he or she may also discover signs of lung cancer. A symptom is something you experience such as a cough or shortness of breath. A sign is something observed by your doctor such as abnormal lung sounds heard with a stethoscope. Some things can be both a sign and a symptom. For example, you experience fever as a symptom that can also be observed as a sign of illness by your health care provider. Signs and symptoms of lung cancer are usually grouped into the following • those related to the original lung tumor (the primary tumor) • those related to spread of cancer in the chest (intrathoracic or local spread) • those related to spread of the cancer outside the chest (distant metastasis) • those related to paraneoplastic syndromes Paraneoplastic syndromes are groups of signs and symptoms not caused by cancerous tumors themselves but by substances produced by the tumors. These syndromes can affect a number of organs and cause a wide variety of signs and symptoms. Studies have shown that approximately 10% of people with lung cancer have paraneoplastic syndromes.1, 2
Before beginning a detailed description of the signs and symptoms of lung cancer, we want to say a few words about what to do if you experience a new sign/symptom or a change in a previously existing sign/symptom. 1. Do not ignore it. 2. Do not panic. Understandably, some people with lung cancer think any symptom they experience must be related to their cancer and ignore it. This is a mistake. Just because you have lung cancer does not mean that every symptom you experience is related to your cancer. You are subject to the same ‘normal' things everyone else is. The only way to know if a symptom is cancer- related is to let you health care team evaluate the problem. It is not in your best interest to ignore something that may give your doctors important information about your cancer. It is also important not to ignore a symptom that may indicate something new is happening in your body. While some people have a tendency to ignore their symptoms, others have a tendency to panic. Lung cancer is a life-threatening illness. It is perfectly understandable that some people become frightened by the development of a new symptom because they assume it means the disease has gotten worse. Jumping to this conclusion can cause a great deal of worry and emotional distress − and may be completely wrong. For example, lung cancer that has spread to the brain can cause headaches. Nonetheless, sometimes a headache is just a headache. The point of this example is not to tell you to ignore a headache − in fact you most definitely should report any new headaches to your health care providers. The point is to encourage you to not jump to conclusions. The best course of action to take when you experience a new symptom is to report it to your health care provider as soon as possible. He or she will evaluate the cause and take appropriate action to treat the underlying problem, regardless of whether it is related to your Over the next several pages, the signs and symptoms of lung cancer are explained. Under each listing, there is also a discussion of supportive care measures used to control or alleviate the sign/symptom.
SYMPTOMS ASSOCIATED WITH PRIMARY LUNG TUMORS
Cough is the most common symptom experienced by people with lung cancer. Coughing is the body's natural way of clearing the airways. Dust, chemicals, smoke, excessive phlegm, and other substances irritate the airways leading to the urge to cough. We have all had the experience of having something ‘go down the wrong way', that is, going into the airway instead of the stomach. This causes irritation in the airways that leads to immediate and explosive coughing as the body tries to clear the lungs of a substance that should not be There are two main types of coughs, dry coughs and productive coughs. Dry coughs are referred to as hacking or barking coughs because of how they sound. Dry coughs can be quite persistent but do not usually result in coughing anything up. Dry coughs are commonly caused by inhaling smoke or another irritant, breathing cold air, viruses, allergies, sore throats, sinus infections, and certain forms of asthma. There are other causes for dry coughs, too. Productive coughs have a loose sound and frequently result in coughing up phlegm. This type of coughing often feels as if it is coming from deeper in the chest than a dry cough. Productive coughs indicate congestion or excessive fluid in the lungs. The fluid may be watery or thick depending on the underlying cause of the cough. Phlegm that is bloody or streaked with blood is called hemoptysis, and is relatively common in people with lung cancer. Cold or flu viruses, pneumonia, and bronchitis are common causes of productive coughs. There are many other causes as well. Despite the fact that many people with lung cancer have a cough related to their cancer, there are many other causes of cough. Your health care provider will evaluate you to determine the cause of your cough so that he or she can prescribe an appropriate treatment. It is important to accurately identify the cause of a cough in order to effectively treat it. For example, certain blood pressure medications can cause cough. A cough caused by medication can easily be alleviated by switching to another medicine, a much simpler and more effective solution than trying to suppress the cough. Tumors that partially or completely block an airway can lead to pneumonia and a productive cough. Antibiotics are often used to treat pneumonia. Your doctor may also recommend a procedure to clear the blocked airway. This can help avoid repeated bouts of pneumonia. Persistent coughing caused by a tumor irritating the airways can be a very troubling symptom. Coughing can interfere with sleeping, eating, and even conversation. Mild cough suppressants found in over-the-counter cough medicines may help some people but often do not adequately control this symptom. Coughs associated with lung cancer often require stronger medications. Medicines called bronchodilators may help relieve cough. Drugs called opiates such as codeine, oxycodone, and morphine are powerful cough suppressants and may be needed to control severe coughing. Inhaled morphine can suppress a cough while limiting its effects on the rest of the body. If one form of therapy does not adequately control your cough, be sure to talk with your health care provider. There are several options available to help treat this troublesome and disruptive symptom. Breathing Difficulties (Dyspnea)
Dyspnea is a common symptom of lung cancer. Dyspnea is defined as difficult, labored, or
uncomfortable breathing. People with dyspnea describe it as a feeling of air hunger. Dyspnea is triggered when the cells of the body are not getting enough oxygen. Sensations of dyspnea may include tightness in the chest, fast breathing, and/or shortness of breath. Dyspnea and the effects of having too little oxygen in the body can seriously affect your quality of life. Lung cancer can cause dyspnea in several different ways including blockage of the airways by a tumor, fluid in or around the lungs, anemia, and muscle weakness. Dyspnea caused by partial blockage of a large airway may cause noisy breathing or wheezing. Dyspnea can also be caused by other medical conditions such as asthma, chronic obstructive pulmonary disease (COPD), emphysema, pneumonia, or heart disease. Shortness of breath usually causes anxiety, which tends to make the problem worse. To treat dyspnea effectively, the underlying cause must be determined. Your doctor may send you to a pulmonologist (an expert in the treatment of lung diseases) to help determine the specific cause of your dyspnea. The treatment recommended by your health care provider will depend on the underlying cause of the problem. Following are some of the treatments your doctor may recommend to help alleviate dyspnea. Supplemental Oxygen Supplemental oxygen increases the amount of oxygen taken in with each breath. This eases shortness of breath by providing the body with the oxygen it needs. Supplemental oxygen is moisturized to keep it from drying the airways. Medications A variety of breathing medications can be used to treat dyspnea. The choice of medications depends on the underlying cause of your symptoms. Drugs called bronchodilators open up the airways. Steroids are also sometimes used. Some medications are taken by mouth; others are inhaled. Pain can worsen dyspnea. Therefore, pain medication such morphine sometimes helps alleviate severe dyspnea. Treating Airway Obstruction If one or more of your major airways is obstructed by a tumor, you doctor may recommend a procedure to clear the airway. The procedure recommended depends on the location of the tumor and other factors. Options include: external beam radiotherapy brachytherapy (internal radiation) dilation of the airway with a balloon placement of a tubular device called a stent to hold the airway open cryoablation (freezing) electrocautery (electrical current) argon plasma cautery (APC) photodynamic therapy (PDT) surgery − used in special circumstances to remove obstructing tumors Treating Anemia Anemia can cause or worsen dyspnea. The cause of your anemia will be evaluated by your doctor and he or she will treat you accordingly. Severe anemia may require a blood transfusion. If the need for blood is not immediate, your doctor may recommend another form of treatment. See the Treatment Related Symptoms section of this chapter for additional information on treatments for anemia. Treating Malignant Pleural Effusion A malignant pleural effusion is an accumulation of fluid in the sac surrounding the lung. It is caused by cancerous invasion of the sac. Seven to fifteen percent of people with lung cancer develop a pleural effusion.3-5 Approximately 50-77% of the people with
a pleural effusion develop shortness of breath associated with the effusion.6
Dyspnea is the main reason to treat a pleural effusion. There are different ways to treat a malignant pleural effusion. • Drain the fluid by inserting a needle into the pleural sac. Pleural fluid tends to reaccumulate, which may make it necessary to repeat the drainage process. • Pleurodesis involves draining the pleural fluid and placing a substance (a sclerosing agent) in the pleural space to create irritation. The irritation causes the two sides of the pleural sac to stick together leaving no room for reaccumulation of fluid. Pleurodesis can be done two different ways. The chest tube method involves inserting a tube through the chest wall into the pleural space. The tube is attached to a suction device that gently draws out the pleural fluid. Once the fluid has been drained and a local painkiller has been administered, a sclerosing agent is injected into the pleural space. Alternatively, pleurodesis can be performed through an endoscope, which allows the surgeon to see the pleural space. The chest tube method is performed with a local painkiller and a sedating drug. The thoracoscopic method is done under general anesthesia. Talc is the most commonly used sclerosing agent, but there are other substances in use including bleomycin and tetracycline. • Other surgical procedures can be used to treat malignant pleural effusions that have not responded to less invasive treatments. Some people with dyspnea have found the following self-help techniques useful in controlling this troubling symptom. While these techniques may help alleviate your shortness of breath, be sure to discuss your dyspnea with your health care provider. Dyspnea may indicate a serious underlying problem that requires medical treatment. Controlled BreathingBreathing normally takes place outside your conscious awareness. Focusing attention on breathing and doing it in a controlled way may help alleviate shortness of breath. Begin by taking a normal breath in through your nose. Count the number of seconds you inhale. Breathe out through pursed lips for twice as long as you inhaled. Do not force the air; just breathe out in a controlled manner. Abdominal Breathing Abdominal breathing is a technique in which you use both your chest and abdominal (stomach) muscles to help you breathe more deeply. Babies and young children naturally breathe this way, which is why abdominal breathing is sometimes called baby breathing. As we grow older, we tend to change to chest breathing using primarily the muscles of the chest and the diaphragm (the large muscle under the lungs that separates the chest from the abdomen). Women are almost exclusively chest breathers whereas men tend to use both abdominal and chest breathing. With normal breathing, we typically use only 10-20% of our lung capacity. Abdominal breathing helps you use a much greater amount of your lung capacity with each Abdominal breathing is best learned while lying on your back with a pillow under your knees. Place one hand on your upper chest and the other on your abdomen below your ribs. Breathe out slowly through pursed lips. Squeeze your abdominal muscles upward and inward. Your abdomen will move inward toward your back. Breathe in through your nose. Your abdomen will rise. Once you have mastered abdominal breathing, you will be able to use it in any position. Abdominal breathing may greatly increase your ability to take in necessary oxygen. Some people with lung cancer have found this technique very helpful in reducing shortness of breath. Relaxation can help reduce dyspnea in two different ways. When you are anxious, as people who are short of breath often are, you tend to take short, shallow breaths. Short, shallow breaths are not an effective way to breathe. When you relax, your breathing slows and becomes deeper. Deep breathing brings more oxygen into the lungs with each breath. In addition, when you are anxious, your muscles are tense. Tense muscles use more oxygen than do relaxed muscles. Relaxing your muscles decreases their demand for oxygen, which helps reduce air hunger. People relax in different ways. Soothing music, dim lighting, or a warm bath works for some people. Other people practice techniques that can be used no matter where you are such as visualization or meditation. Chapter 11: Complementary Healing has additional information about these and other relaxation techniques. Posture and Body Position Posture and body position can affect how deeply you breathe. Notice your posture. Slouching with your shoulders rolled forward prevents your rib cage from fully expanding with each breath. Try bringing your shoulders up and back. This opens the chest cavity and allows you to bring more air into the lungs. Sit or lie down if you are short of breath. This decreases your need for oxygen to hold up your body weight and allows your muscles to relax. Sitting with your feet spread shoulder width apart while leaning forward with your elbows on your knees opens up the chest. Chest Discomfort
Up to 50% of people with lung cancer experience chest discomfort. The pain often comes
and goes. It is often vague rather than sharp pain. Some people experience aching pain. The chest discomfort caused by lung cancer is best alleviated by treating the underlying cancer. If the pain persists, your health care provider may recommend pain medication. Weight Loss
Unintentional weight loss is a common symptom of lung cancer. Someone with lung cancer
may lose weight for any of a number of reasons. The causes for weight loss often change over the course of the disease. The most distressing and serious type of cancer-related weight loss is part of a complex process known as cancer cachexia. Cachexia most often accompanies advanced stage disease. The hallmark of cachexia is substantial weight loss that involves not only fat but also lean body mass, that is, the non-fatty tissues of the body such as muscle and bone. Cachexia is usually accompanied by loss of appetite (anorexia) and weakness. Cachexia can be very upsetting to both patients and their loved ones. Loss of fat in the face can change its appearance. The eyes and cheeks may take on a sunken appearance, and the bones of the face tend to become more prominent especially around the eyes and the forehead. Many people have heard that cancer causes people to lose weight because the cancer uses all the nutrients a person takes in, starving the rest of the body. While on the surface this makes some sense, the mechanisms of cachexia are far more complex. Researchers have found cancerous tumors can produce substances that affect the body's metabolism. Other studies have shown that the body's reaction to cancer can also influence metabolism. While all the details are not yet worked out, it seems the weight loss associated with cancer cachexia is due to complex processes influenced by both substances produced by tumors and the
body's reaction to the tumors.7
Cachexia is notoriously difficult to treat. Simply increasing the number of calories in the diet often does not reverse true cachexia. The best treatment for cancer cachexia is to eliminate the cancer, if possible. While cachexia is quite serious and distressing, it is important to keep in mind that there are a number of less serious causes of weight loss for someone with lung cancer that are more easily and effectively treated. A persistent cough can interfere with eating, which in turn can lead to weight loss. In this situation, controlling the cough allows normal eating to resume. This arrests or reverses weight loss. Similarly, breathing difficulties can interfere with normal eating. If the breathing problem can be controlled so that normal eating is possible, weight loss can be stopped. In rare instances, lung tumors can interfere with swallowing. Again, treating the swallowing difficulty will prevent further weight loss and allow normal eating. Depression is relatively common among people with lung cancer and frequently causes reduced appetite and weight loss. If depression is the underlying cause of weight loss, successful treatment of depression will halt further weight loss. Medications can be used to counteract or stop the muscle wasting (loss of lean body mass) that accompanies substantial weight loss. The most commonly used drug for cancer-related
weight loss is megestrol acetate (Megace®).8 Megestrol acetate is a synthetic form of the
female hormone progesterone. It acts as an appetite stimulant. However, the weight gain most people experience while on megestrol acetate is primarily body fat, not lean body mass. Dronabinol (Marinol®) is another appetite stimulant and anti-nausea medication. Dronabinol is a prescription medicine that contains a synthetic form of one of the active ingredients in marijuana. Corticosteroids such as dexamethasone (Decadron®) and prednisone (Deltasone®, Orasone®) are sometimes used for short-term appetite stimulation. These steroids can only be used for four weeks or less because the appetite stimulating effect decreases over time. More importantly, these drugs actually promote muscle wasting over Anabolic steroids are related to the male sex hormone testosterone. Anabolic steroids promote muscle building and have been used to treat the muscle wasting associated with
cancer cachexia and other chronic illnesses.9, 10 Examples of anabolic steroids include
oxymetholone (Anadrol-50®), oxandrolone (Oxandrin®), and nandrolone decanoate (Deca-Durabolin®). Researchers are currently studying other treatments for cachexia including thalidomide and long-chain omega-3 fatty acids such as those contained in fish oil. Weight loss can be a symptom of local, locally advanced, or metastatic lung cancer. However, profound weight loss and cachexia are most commonly associated with advanced, metastatic disease. Weight loss is included in this section under symptoms associated with the primary tumor because it seems to be related to the body's reaction to the cancer itself. For additional information on weight loss and nutrition, see Chapter 12: Nutrition and Lung
SYMPTOMS ASSOCIATED WITH INTRATHORACIC SPREAD OF LUNG
When lung cancer spreads to other structures in the chest, it can cause specific symptoms
depending on the structures involved. Chest Pain
Pleuritic pain is sharp pain that occurs with breathing. It occurs when lung cancer invades the outer covering of the lung called the pleura. Cancer that has spread to the area in the center of the chest called the mediastinum can cause pain behind the breastbone. Pain in a specific spot on the chest (often called point tenderness) may indicate invasions of a tumor into the chest wall or a rib. Chest pain caused by lung cancer spread is best alleviated by treating the cancer. Pain medication and other pain control measures may also be used.
Dysphagia
Dysphagia is difficulty swallowing. If lung cancer spreads to the lymph nodes of the chest causing them to greatly enlarge, they can press against the esophagus (the tube that takes food and liquids from the mouth to the stomach). This can cause difficulty swallowing. This is a rather unusual symptom of lung cancer. It is treated by reducing the size of the involved lymph nodes with chemotherapy, radiotherapy, or less commonly, surgery. Facial Swelling
Lung cancer that spreads to lymph nodes near the trachea (the tube that takes air from the
nose and mouth to the lungs) can press against a large vein called the superior vena cava. If flow is partially blocked, a condition called superior vena cava obstruction (SVCO) develops. Blood backs up in the face, neck, and chest. The veins become dilated and are often very noticeable. Facial swelling is most noticeable around the eyes if the obstruction is mild, but can become severe and involve the entire face and neck. SVCO is sometimes accompanied by headache, dizziness, drowsiness, and/or blurred vision. SVCO can be treated by having a specialized radiologist (an interventional radiologist) place a tube (called a stent) in the superior vena cava to hold it open and permit normal blood flow. Radiation therapy to reduce the size of the enlarged lymph nodes is also used either alone or in combination with stenting. Hoarseness or Change in Voice
Sudden, persistent hoarseness not associated with a cold or sore throat, or another change in the voice may indicate your lung cancer has spread to the nerve that controls the vocal cords. This symptom is usually accompanied by difficulty clearing phlegm when coughing. Invasion of the nerve is usually addressed by treating the underlying cancer.
Shoulder Pain
A lung tumor in the uppermost part of the lung (the apex) can invade the nerves and blood vessels nearby. A tumor in this location is called a Pancoast tumor. This type of tumor often causes a specific set of symptoms known as Pancoast syndrome. The most common symptom is shoulder pain. This is often accompanied by numbness, tingling, or weakness in the arm and/or hand. The skin of the arm and/or hand may be cool to the touch. A group of three symptoms known as Horner's syndrome can also accompany a Pancoast tumor. Horner's syndrome involves a drooping eyelid, a small pupil in the affected eye, and lack of sweating on the affected side of the face. Pancoast tumors can often be successfully treated surgically after combined radiotherapy and chemotherapy. Surgery may reverse symptoms associated with the tumor.
SYMPTOMS ASSOCIATED WITH METASTATIC SPREAD OF LUNG CANCER
Lung cancer can metastasize to almost any organ of the body. The most common sites of lung cancer metastases are the brain, liver, bones, and adrenal glands. Symptoms associated with metastatic disease in these locations are discussed in this section. However, keep in mind that lung cancer may spread to other sites. Be sure to discuss any new symptoms with your health care provider.
Abdominal Pain
Metastatic liver tumors can cause pain on the right side of the body below the ribs. The pain is caused by tumor growth causing pressure in the liver. The liver is enclosed in a capsule that has little capacity to expand. Anything that increases the size of the liver causes increased pressure leading to pain. The adrenal glands are another common site of lung cancer metastasis. While adrenal tumors often do not cause symptoms, they can cause pain if they grow large or invade a blood vessel and cause bleeding into the gland. The pain associated with adrenal metastasis is typically located in the back, around waist-level, to the right or left of the spine. The best ways to alleviate the pain associated with liver or adrenal metastasis are treating the cancer and pain medicine. Bone Pain
Metastatic bone disease is usually accompanied by pain in the affected bone. Pain can range
from mild to severe. Any bone in the body can be a site of metastatic lung cancer. Bones invaded by cancer tend to be weak because some of the bone has been eroded away. Eroded bones are prone to breakage. Bone breaks associated with metastatic cancer are called pathological fractures. These fractures typically occur without any history of a fall or an impact, or are associated with a minor impact that would not normally cause a bone to break. Pain from bone metastasis is often treated with radiation therapy (RT) if the affected bone is in a suitable location. Corticosteroids such as prednisone may improve the pain relief provided by RT. If RT fails for provide adequate pain relief, other treatment options are available such as: • bisphosphonates such as etidronate (Didronel®), pamidronate (Aredia®), alendronate (Fosamax®), risedronate (Actonel®), and zolendronate (Zometa®) • calcitonin • radiopharmaceuticals including strontium 89 (Metastron R®), samarium 153 (Quadramet®), rhenium 186, and rhenium 188 If the long bones of the arms or legs have been eroded by bone metastases, your doctor may recommend surgery to stabilize the bone with metal rods or other reinforcements. The surgery is done to prevent a future fracture that could be painful and disabling. Pain medications are commonly used to treat metastatic bone pain. There are many pain medications available. If one medicine does not control your pain, a stronger medicine or a higher dosage can be used. When working toward pain control, close communication between you and your health care provider is very important. Do not be afraid to speak up when you are in pain. The only way your providers can help is if you are honest with them about your pain. See the section on Pain Control later in this chapter for more information about pain medicines.
Central Nervous System Symptoms
The symptoms of metastatic tumors in the brain vary depending on the size, location, and number of tumors present. Severe headaches, uncontrollable vomiting, and seizures are symptoms associated with increased pressure in the brain. Weakness or paralysis limited to a specific area of the body may indicate a tumor in the area of the brain that controls the affected part of the body. Changes in vision, difficulty speaking or swallowing, loss of balance or coordination, and confusion are other possible symptoms associated with metastatic brain disease. The symptoms associated with metastatic brain tumors are alleviated by treating the tumors. Steroids such as dexamethasone can be used short-term to reduce brain swelling that often accompanies metastatic tumors. Steroids are particularly useful for alleviating symptoms such as headaches and uncontrollable vomiting. Brain tumors can also be treated with whole brain radiation therapy (WBRT). This therapy is often used for people who have more than one metastatic brain tumor. WBRT is usually effective at relieving the symptoms associated with these tumors. Stereotactic radiosurgery (SRS) is another form of radiation treatment for brain tumors. SRS is generally used on people who have one small brain tumor (less than 3 cm or 1¼ inches). SRS usually involves placing a device on the head called a skeletal fixation device. This allows the radiologist to direct high-energy radiation toward the tumor in a very accurate way that limits the radiation exposure and potential damage to normal brain tissue. Unlike WBRT that takes place over a number of days, SRS is performed in a single treatment. There are three forms of SRS: cobalt 60 or photon systems, linear accelerator systems, and particle beam or proton systems. Photon systems are widely available in specialized treatment centers. The most common SRS photon system is known by the brand name Gamma Knife®. Linear accelerator systems are also widely available and are often referred to with the abbreviation ‘linac.' Brand names of specific linac systems include X-Knife®, CyberKnife®, and Clinac®. Proton systems are in limited use in the United States. In some cases, metastatic brain tumors are surgically removed. Your doctors will consider several factors in deciding what treatment is best for your situation. The number of tumors and their location, your overall condition, current quality of life, and likely quality of life after the treatment are important factors in deciding on treatment options. Any treatment involving the brain involves a risk of brain injury. All treatment options and possible outcomes must be carefully considered. Lung cancer can metastasize to the outer covering of the spinal cord. These tumors press on the spinal cord causing pain, numbness, and/or weakness in a specific area of the body. In severe cases, these tumors can cause paralysis. Losses of bowel and bladder control are other possible symptoms of this condition known as spinal cord compression. Radiation therapy is the most common treatment for this condition. Steroids may be given along with radiation therapy. In special circumstances, surgery may be an option. Your doctors will evaluate the location of the tumor and possible outcomes before recommending a specific treatment. Discuss these options with your doctor, including possible side effects of treatments and the probability of regaining lost function.
PARANEOPLASTIC SYNDROMES
Paraneoplastic syndromes (PNPs) are not due to the physical effects of cancerous tumors. They are caused by substances produced by the tumors acting on tissues in the body. Approximately 10% of people with lung cancer experience symptoms of a paraneoplastic syndrome over the course of their illness.1, 2 There are many different PNPs with a great
variety of symptoms. In this section, some of the more common PNPs and their symptoms are discussed. However, many other symptoms can occur as part of a paraneoplastic syndrome. Be sure to discuss any new symptoms with your health care provider. Cushing Syndrome
Cushing syndrome is caused by abnormally high levels of adrenocorticotropic hormone (ACTH).
ACTH is normally produced by a small structure in the brain called the pituitary gland. ACTH acts on the adrenal glands, stimulating them to produce and release steroid hormones called glucocorticoids. Cortisol is the main glucocorticoid produced by the adrenal glands. Cortisol has many actions throughout the body. Paraneoplastic Cushing syndrome is most commonly seen in people with small cell lung cancer. Normally, the adrenal production of ACTH is closely controlled by the pituitary gland. However, in lung cancer-related Cushing syndrome, cancer cells produce ACTH in an uncontrolled way. Excess ACTH can lead to signs and symptoms such as weakness, muscle wasting, a round appearance to the face, weight accumulation in the trunk of the body, high blood glucose, low blood potassium, high blood pressure, increased body hair, drowsiness, and confusion. The signs and symptoms of Cushing syndrome usually disappear when the underlying cancer is treated. The drug ketoconazole (Nizoral®) is sometimes used to control the signs and symptoms of Cushing syndrome. Digital Clubbing and Hypertrophic Osteoarthropathy
Digital clubbing is rounding of the ends of the fingers accompanied by a flattening of the
normal angle between the nail and the nail bed (see Figure 1). Clubbing can occur in a single finger, only on the fingers of one hand, or can involve both hands. The toes can also be affected. Clubbing may be accompanied by a warm sensation in the affected fingertips.


Clubbing can be found alone or in combination with
hypertrophic osteoarthropathy (HOA). In HOA, the outer layer of the long bones of the arms and/or legs is inflamed causing
pain and swelling in the ankles, wrists, and knees. This inflammation can be seen on x-rays. Clubbing is more
common than the combination of clubbing and HOA. Clubbing and HOA, both alone and in combination, can be
seen with several conditions other than lung cancer.
Figure 1: Digital Clubbing*
Cancer-related clubbing and HOA may partially or complete
resolve with successful treatment of the underlying lung cancer. Pain medications are used
to control joint pain associated with HOA.
Hypercalcemia
People with lung cancer can have high levels of blood calcium (hypercalcemia) because of
metastases to bones or a paraneoplastic syndrome. The paraneoplastic syndrome that leads to hypercalcemia is caused by production of a hormone-like substance by lung cancer cells.
This paraneoplastic syndrome is most commonly seen with squamous cell carcinoma. Symptoms of hypercalcemia include thirst, dehydration, abdominal pain, decreased appetite,
nausea, vomiting, constipation, excessive urination, muscle weakness, fatigue, irritability, and confusion.
Paraneoplastic hypercalcemia can be treated with medicines such as pamidronate (Aredia®),
plicamycin (Mithracin®), calcitonin, and gallium nitrate. Treating the underlying cancer is the best way to resolve paraneoplastic hypercalcemia.
Neurologic Syndromes
There are several neurologic paraneoplastic syndromes, and any part of the nervous system can be affected. While these neurological syndromes are relatively rare, when they do occur,
it is usually in conjunction with small cell lung cancer. PNP neurological syndromes are thought to be due to antibodies produced by the body against its own nerve tissues. These
*Copyright 2005 Nucleus Medical Art (www.nucleusinc.com). All rights reserved.
neurologic syndromes sometimes appear before the diagnosis of lung cancer is made.
Symptoms include numbness, burning or prickly sensations in the hands and feet, weakness, muscle aches, muscle stiffness or cramps, dry mouth, constipation, inability to empty the
bladder completely, impotence, loss of balance, light sensitivity, night blindness, personality changes, confusion, and memory loss.
The primary treatment for PNP neurologic syndromes is treatment of the underlying cancer.
Syndrome of Inappropriate Antidiuretic Hormone (SIADH)
Antidiuretic hormone (ADH) is normally released into the body by a small gland in the brain called the pituitary gland. ADH acts on the kidneys to control water balance in the body. Its
production is normally tightly controlled. Paraneoplastic SIADH is caused when lung cancer cells produce ADH in an uncontrolled way. This syndrome is most commonly seen in
people with small cell lung cancer. The abnormally high amount of ADH causes a low blood sodium level and excess water accumulation in the body. Symptoms of SIADH
include weakness, fatigue, headache, loss of appetite, and nausea. If the sodium level is extremely low, there can be confusion, seizures, and coma.
Mild SIADH can be treated by cutting back fluid intake. The medicine demeclocycline
(Declomycin®) and intravenous salt solution may also be needed. Treatment of the underlying cancer usually results in rapid resolution of this paraneoplastic syndrome.
Other Manifestations of Paraneoplastic Syndromes
Several other uncommon paraneoplastic syndromes can accompany lung cancer. Following is a list of some of the signs and symptoms that may indicate the presence of a
paraneoplastic syndrome.11
Hormonal Problems
breast enlargement (especially in men)
low blood sugar
high thyroid hormone
high female hormones
decreased urine production
rashes itching hives
Blood and Blood Vessel Problems
inflamed blood vessels (vasculitis)
high blood platelets (thrombocytosis)
low blood platelets (thrombocytopenia purpura)
red blood cells (anemia)
high white blood cells (leukocytosis)
OTHER CANCER RELATED SYMPTOMS
Anemia is a condition in which the number of red blood cells circulating in the body is abnormally low. Lung cancer can cause anemia as part of the cancerous process. The
mechanisms that cause anemia in people with cancer are complex. Lung cancer treatments can also lead to anemia.
Anemia can cause many different symptoms including shortness of breath, fatigue,
sleeplessness, and weakness. The treatments for cancer-related anemia and treatment-related anemia are generally the same. This information is discussed in the section on Treatment
Related Symptoms.
Blood Clots
People with lung cancer have an increased risk for developing blood clots in their veins.
This is particularly true for people with adenocarcinoma or large cell lung cancer. It is less common in people with squamous cell carcinoma or small cell lung cancer. Blood clots
usually form in the veins of the legs. Unexplained swelling in your foot or lower leg may indicate the presence of a clot. Blood clots can also develop in the arms. This is especially a
risk for people who have a long-term intravenous access device such as a central line (a
Groshong® catheter or Hickman® line), a port (Portacath®), or a PICC line. Contact your
doctor immediately if you develop unexplained swelling in one of your extremities, neck, or face.
Blood clots are a potentially serious problem because pieces of the clot called emboli can break off and travel through the bloodstream to the lungs, heart, or brain causing damage to
these vital organs. All these situations are serious and can be life threatening if they are not treated immediately.
A blood clot in a vital organ is often treated with a medicine that will dissolve the clot and restore normal blood flow. These drugs are called thrombolytics or clot busters. Examples of
these drugs include reteplase (r-PA, Retavase®), alteplase (t-PA, Activase®), urokinase (Abbokinase®), streptokinase (Streptase®), and anisoylated purified streptokinase activator
complex (APSAC, anistreplase, Eminase®).
People who develop blood clots in the veins (deep venous thrombosis or DVT) are often treated
with anti-clotting medicines called anticoagulants or blood thinners. These medicines do not dissolve the clot but keep it from getting larger. Blood thinners also help prevent new clots
from forming elsewhere. Three anticoagulants are used to treat venous blood clots.
Heparin (unfractionated)
Heparin is a naturally occurring anticoagulant. It is administered through an intravenous line (IV). People on heparin often have to be in the hospital.
Low Molecular Weight Heparins (LMWH) This is a newer form of heparin therapy than unfractionated heparin. LMWH stays
in the body for a longer period than standard heparin. This makes it possible to give LMWH in a shot under the skin once or twice per day rather than in a continuous
IV. LMWH can often be administered at home rather than in a hospital.
Warfarin (Coumadin®)
Warfarin is taken by mouth but does not become effective until 4-5 days after beginning treatment.
Treatment of a DVT usually begins with heparin therapy (either standard or LMWH).
Warfarin is usually started at the same time. Heparin therapy is continued until the warfarin takes effect. Once the warfarin has taken effect, heparin therapy is stopped. Your health
care providers must closely monitor your blood when you are on anticoagulant therapy. A PTT blood test (partial thromboplastin time) is used to monitor the effects of heparin. A PT
test (prothrombin time) is used to monitor the effects of warfarin. Your blood will be tested frequently while you are on anticoagulant therapy to make sure you are getting enough
medicine to prevent clots without putting you at risk for bleeding. People who have had a DVT typically stay on anticoagulant therapy for six months or longer. During this time, the
body's normal mechanisms often partially or completely dissolve the original clot.
Constipation
The weakness, fatigue, lack of appetite, and reduced activity that many people with lung
cancer experience can lead to constipation. Many pain medications also cause constipation. Increased activity can help relieve constipation. Walking is a relatively non-strenuous activity
that can alleviate constipation. Abdominal breathing (described under Dyspnea in this section) can help improve bowel activity. Changes in diet may also be useful. Fruits,
vegetables, and fiber often help improve bowel activity. Be sure to drink plenty of water. Low fluid intake can significantly worsen constipation. If needed, your health care provider
can recommend medications or herbs that can alleviate constipation.
Depression and Anxiety
Many people with lung cancer are depressed at some point in their illness. When most
people talk about being depressed, they are describing the experience of feeling very sad. People who are depressed often cry, lack interest in normal activities, and/or experience low
energy or tiredness. Depression is a completely normal response to a sad, disappointing, unexpected, and/or stressful situation. Health care providers often use the term reactive
depression to describe this normal response to any of a number of stressful life situations. Most people who experience reactive depression also have symptoms of anxiety. Anxiety is
described as a lingering feeling of uneasiness, worry, and/or being on edge. You may feel your mind is racing and have difficulty focusing. Anxiety can also be experienced as a sense
of dread. Again, both anxiety and depression are normal responses to learning you have
lung cancer. However, these normal responses have the potential to interfere with your life
and health if they become prominent. Some symptoms you may experience with depression and anxiety are shown in the following lists.
Symptoms Associated with Depression12
• persistent sad, anxious, or empty mood • feelings of hopelessness or pessimism • feelings of guilt, worthlessness, or helplessness • loss of interest or pleasure in hobbies and activities that you once enjoyed
• decreased energy, fatigue, or feeling slowed down • difficulty concentrating, remembering, or making decisions • difficulty sleeping or sleeping too much • appetite and/or weight loss, or overeating • thoughts of death or suicide • restlessness or irritability • persistent headaches that are not attributable to another cause and do not
respond to treatment
Symptoms Associated with Anxiety
• sweating • dizziness • racing heart or irregular heart beat • shakiness • difficulty relaxing • headaches • irritability • upset stomach, nausea, and/or diarrhea • sleeping problems • difficulty concentrating
• excessive watchfulness • being easily startled
While depression and anxiety are normal reactions to stressful situations, they can become problems if they begin to interfere with your ability to function. If you or one of your loved
ones notice one or more of these symptoms are disrupting your life, discuss the situation with your health care provider. He or she may recommend counseling, medication, or
another form of therapy such as relaxation techniques to help relieve your symptoms. The important message is that you should not ignore these symptoms, nor should you suffer
from them for a prolonged period. Talk to your doctor or nurse. Anxiety and depression are normal reactions. They do not mean you are losing control of your mind, and they are
not signs of weakness. However, they do need to be controlled if they are interfering with your ability to function or your quality of life.
Some symptoms of depression may be alleviated by talking through your feelings and
concerns with others, whether it be in a support group, with family members, or in appointments with a counselor. Psycho-oncology is a field of psychology that focuses
exclusively on people with living with cancer. Oncology social workers also specialize in working with and counseling people who have cancer. Chapter 9: Living with Lung Cancer has
additional information on coping with lung cancer.
For many people with lung cancer, counseling and self-help measures are not enough to adequately control depression. This is nothing to be ashamed of; it is not a sign of
weakness. Discuss your feelings with your health care providers. Medication may be recommended to help control your depression and anxiety. Many medications are available
for these purposes. Some people worry that medications used to control anxiety and/or depression will put them to sleep or make them feel otherwise not themselves. While many
older medications had some of these unwanted side effects, newer medications are greatly improved. Commonly used antianxiety medications include lorazepam (Ativan®),
alprazolam (Xanax®), diazepam (Valium®), and many others. Fluoxetine (Prozac®), sertraline (Zoloft®), bupropion (Wellbutrin®), zaleplon (Sonata®), paroxetine (Paxil®), citalopram
(Celexa®), and venlafaxine (Effexor®) are just a few of the many medications available to
control depression and its symptoms. If one medication does not work for you, you can try another. Many people who are not helped by the first medication they try are happily
surprised when their symptoms are alleviated with another medication – so don't give up.
Fatigue
Fatigue can be the most debilitating symptom associated with lung cancer and its treatment.
Fatigue associated with lung cancer is different from everyday tiredness. It is an overwhelming, sustained sense of exhaustion. It is often accompanied by a decreased
capacity for physical and mental work. Fatigue can have a profound impact on your ability to carry out normal life activities. While lung cancer itself can cause fatigue, treatments for
lung cancer can also cause fatigue. This can make fatigue temporarily worse during treatment.
Fatigue varies in severity from one person to another, and often waxes and wanes over the
course of the disease. At times, your fatigue may be mild and alleviated by simple measures such as napping during the day or cutting back on your most strenuous activities. At other
times, fatigue can be severe and may force you to significantly alter your lifestyle and activities.
Fatigue can be difficult to treat. Lung tumors can reduce your breathing capacity. Lung
cancer surgery involves removal of both diseased and healthy lung tissue, which also reduces breathing capacity. Both of these situations can cause fatigue because reduced breathing
capacity decreases the amount of oxygen taken in by the lungs with each breath. The reduced ability to deliver oxygen to body tissues results in becoming easily fatigued with
exertion. Anemia can worsen this problem by reducing the blood's capacity to carry the oxygen taken in by the lungs. Your health care provider will monitor your blood regularly to
check for anemia. Treating anemia often helps alleviate fatigue.
Table 1, Suggestions for Energy Conservation, offers a number of simple, practical suggestions for how to conserve energy in your everyday life when you are experiencing fatigue.
Table 1: Suggestions for Energy Conservation*
• Spread chores out over the week rather than trying to do them all in one day.
• Do a little bit at a time; rest when you get tired. • Have someone help you with strenuous tasks and heavy lifting.
• Use a cart or apron to carry your supplies. • Do whatever you can while sitting down.
• Use long-handled dusters, mops, and dust pans to avoid a lot of stooping.
SHOPPING
• Make a shopping list; organize it by the store aisles.
• Combine errands to reduce the number of trips you need to make.
• Use a scooter cart if available to allow you to sit while you shop. • Ask for assistance taking your purchases to and loading them into the car.
• Shop when the store is not busy to limit the amount of time at the store. • Shop with a friend or ask a friend to shop for you.
PREPARING MEALS
• Assemble your ingredients before you begin. • Use mixes and prepackaged, microwavable, heat-and-eat, ready-to-eat and other food
products that reduce preparation and cooking time.
• Use appliances to reduce work and preparation time such as electric mixers, blenders, food
choppers, and food processors.
• Use lightweight utensils. • Use a jar opener.
• Use a rubber mat or wet towels to steady mixing bowls during stirring. • Transport large items on a rolling cart.
• Serve food from the stove rather than carrying large serving dishes to the table. • Store frequently used items in easy-to-reach places.
• Line your oven and drip pans with aluminum foil for easy clean up.
• Sit while preparing food. • Use a dishwasher.
• Let the dishes soak instead of scrubbing. • Let dishes air dry.
• Prepare double recipes and freeze half for later use.
• Use placemats for easy clean up. • Use a wheeled garbage can.
• Use a laundry cart with wheels to move clothes. • Sit while transferring clothes.
• Have others carry their dirty clothes to the laundry area. • Ask others to put away clean clothes.
• Use pre-treaters and stain removers to a avoid scrubbing stains.
• Wash bras, pantyhose, and stockings in a lingerie bag to avoid tangling. • Drain hand-washables and press dry rather than wringing them out.
• Sit while ironing. • Use a lightweight iron.
• Hang clothes on a doorknob rather than at the top of the door. • Wear clothes that do not require ironing.
Table 1: Suggestions for Energy Conservation, continued
CHILDCARE
• Plan activities such as doing puzzles, playing board games, coloring, reading, etc. that can be
• Plan outings that will allow you to sit down such as going to a movie, storytelling, a play, etc. • Take a nap when your child naps.
• Have ready-to-eat snacks available that don't require preparation. • Have your child crawl into your lap rather than picking him or her up.
• Engage children in household chores by making them into a game. • Place toy containers at the children's level so they can pick up their own toys.
• Take advantage of carpools to limit transporting the children to activities and school.
• Utilize programs that give mothers time off during the day. • Delegate some childcare responsibilities among trusted family members and friends.
WORKPLACE
• Plan your workload around the times when you have the most energy. • Arrange your workplace so that it's energy efficient; keep frequently used items within easy
• Sit when you can.
• Take regular rest breaks.
• Use the telephone, intercom, e-mail, faxes and other telecommunications to limit
unnecessary trips to other locations.
• Discuss the possibility of working from home, if your job allows for this option. • Discuss the possibility of a flexible work schedule or a reduction in your work hours.
ALLOWING OTHERS TO HELP
• Put someone else in charge of organizing the ‘To Do' list and assigning the tasks. • Do not forget to include the ‘little' things on the ‘To Do' list that others can do, for
example: walk the dog, pick up the dry cleaning, weed the garden, do the mending, take the trash to the street, rake leaves, shovel snow, pick up or mail packages, etc.
• Do not feel the need to entertain your helpers; they are there to help. • Try to get used to allowing others to help; you may actually be doing your loved ones a
favor by allowing them to feel useful rather than helpless.
• Make plans, but don't be afraid to change them. If you've made plans to do something but
aren't up to it when the day arrives, let others know how you're feeling – they will
• Do not worry about keeping up with thank you notes. Your loved ones are trying to reduce
your workload not create more tasks for you to accomplish. Your family may want to post a general thank you in a church bulletin, local newspaper, or a group e-mail message.
* Adapted in part from the ""Suggestions for Energy Conservation" Eileen Donovan, P.T. The University of Texas M.D. Anderson Cancer Center. Used with permission.
Other tips to help manage fatigue include:
• Avoid unneeded bed rest.
While it is important to get the sleep you need, staying in bed when you do not need to can actually worsen fatigue. Inactivity leads to muscle weakness and decreased
energy. We have all heard the phrase, "use it or lose it." This is very good advice. In general, the less you do, the less you will feel like doing.
• Try to get some form of exercise each day.
On the surface, this advice may not seem to make sense. However, inactivity leads to muscle loss and weakness that contribute to fatigue. Continue whatever form of
exercise you enjoyed before your diagnosis. You may need to reduce the time or intensity of your exercise program, but do not give it up altogether. If you were not
getting exercise before your diagnosis, talk with your health care providers about beginning a gentle exercise program. Many people find walking is an enjoyable form
of exercise that is not too strenuous.
Exercise can help you in many ways. Regular exercise helps maintain your muscle mass and tone. It also helps keep your respiratory muscles in shape, which may help
alleviate dyspnea. Exercise has also been shown to be useful in alleviating depression. Exercise can take a variety of forms including such things as gardening,
bowling, biking, walking, golfing, weight lifting, dancing, and yoga. Anything that gets you up and moving is exercise. Be sure to discuss your activities and exercise
plan with your health care providers to ensure that your program is safe and effective for you.
• Take a break.
Short rest periods and quiet times throughout your day can help you regain your
strength and energy for the things you need and want to do.
• Limit stress and emotionally draining situations.
Stress and emotionally difficult situations can quickly drain your energy. Examine
your personal situation and try to determine what causes you the most stress. Once you have identified these stressors, work with family, friends, support groups, or
counselors to find ways to minimize these stressors. Refer to Chapter 9: Living with Lung Cancer for additional information about coping with the stresses of living with
• Rest your mind.
There are many things to think about and many decisions to be made when you have lung cancer. These demands can lead to mental fatigue, a feeling of being unable to
think clearly. Mental fatigue can often be relieved by giving your mind a break, much as you give your body break when you are physically tired. Listening to music,
reading, watching a movie, bird watching, meditation, visualization, a warm bath, getting a massage, or any other activity that allows you to mentally relax can give
your mind the rest it needs.
• Eat a well-balanced diet.
The food you eat provides the nutrients and calories (energy) you need. Eating a well-balanced diet with an adequate number of calories can help reduce fatigue. See
Chapter 12: Nutrition and Lung Cancer for information on eating a healthy, energy-rich diet.
Discuss your fatigue with your health care providers and family. Your health care providers
can make recommendations or provide treatments to help reduce your fatigue. You family and friends may be able to help by taking over some of your energy-draining chores.
Weakness
Weakness (asthenia) is a common symptom of lung cancer. It is often associated with dyspnea, fatigue, anemia, and/or weight loss. Activity is generally the best way to counteract
weakness. Even mild exercise can help rebuild lost muscle tone and increase strength. Discuss any weakness you experience with your health care provider. He or she will take
into account other signs and symptoms you may be experiencing and make recommendations about how best to rebuild your strength. Several different treatment
approaches may be recommended including such things as mild exercise, dietary changes, supplemental oxygen, anemia treatments, respiratory therapy, and physical therapy.
TREATMENT RELATED SYMPTOMS
Lung cancer and its treatments can cause anemia, a reduced number of red blood cells circulating in the body. Red blood cells carry oxygen from the lungs to all the cells of the
body. A shortage of red blood cells can deprive the body of needed oxygen, resulting in a variety of symptoms. Fatigue, shortness of breath, dizziness, cold hands and feet, rapid
heartbeat, sleeplessness, and inability to concentrate are some of the symptoms associated with anemia.
Lung cancer treatments can cause anemia or worsen existing anemia. Lung cancer surgery
can cause significant blood loss. Chemotherapy can cause anemia by destroying cells in the bone marrow that produce red blood cells. Certain chemotherapy drugs can also cause
circulating red blood cells to die or be prematurely destroyed. If areas of the body that produce red blood cells are radiated, this can also contribute to anemia.
Your health care providers will monitor your blood counts throughout the course of your
illness, but will monitor you mostly closely when you are on treatment. It is important to treat anemia not only to alleviate symptoms but also to reduce the effects of low tissue
oxygen on the body. Low tissue oxygen can reduce the effectiveness of radiation therapy.13
Anemia is treated in a variety of ways. Iron-rich foods can help replenish body iron if you have a deficiency. Blood transfusions are used if your red blood cell count is extremely low.
Transfusions provide temporary relief of symptoms while other measures are used to promote red blood cell production by your body. Your doctor may recommend treatment
with a man-made (synthetic) form of erythropoietin (Procrit®, Epogen®). Erythropoietin is a hormone produced by the kidneys that stimulates red blood cell production. The synthetic
form of this hormone stimulates the same response in the body. Darbepoetin alfa (Aranesp®) is very similar to erythropoietin but is not taken as often as other synthetic
erythropoietins.
Cognitive Problems
People undergoing treatment for lung cancer can experience cognitive problems. Cognitive functioning refers to the brain's ability to focus attention, and process, store, and retrieve
information. The most common cognitive problems encountered by people with cancer during treatment are:
• short-term memory difficulties • easy distractibility • trouble performing arithmetic • difficulty focusing attention • difficulty performing more than one task at a time
One study found approximately 20% of people undergoing chemotherapy experienced some
form of cognitive side effects.14 These problems are sometimes referred to as chemo-brain,
chemofuzzies, or mental fatigue. Radiation therapy to the brain can also cause cognitive side
effects similar to those seen with chemotherapy. Symptoms of mental fatigue include:
• difficulty maintaining the attention necessary to read • problems with everyday arithmetic such as balancing a checkbook or calculating a tip • forgetting what you were talking about • losing track of things such as your keys, purse, wallet, etc. • repeating yourself
Discuss any cognitive problems you are experiencing with your health care providers. While cognitive problems can be understandably distressing, they are rarely permanent. Following
are some suggestions that may help you minimize the effects of mental fatigue while you are receiving lung cancer treatment.
• Take mental breaks such as listening to calming music, relaxing in your favorite
armchair, taking a bath, etc.
• Plan ahead whenever possible. • Make lists to help you stay organized.
• Make sure you are getting enough sleep. Consider taking short naps during the day if
• Try not to get upset over forgetfulness or other lapses in mental clarity. Anxiety can
worsen mental fatigue.
• Take things one step at a time. • Keep your brain active by participating in mentally challenging activities such as
solving puzzles, playing a musical instrument, doing crafts, writing letters or journal entries, playing board or computer games, playing cards, etc.
• Try to reduce unnecessary stress, which can worsen mental fatigue. • Stay physically active. Physical activity encourages mental clarity.
Constipation
Lung cancer treatments can directly or indirectly cause constipation. Decreased appetite,
nausea, inactivity, fatigue, surgery, and pain medications contribute to constipation. A variety of measures can be taken to alleviate or avoid constipation. Drinking plenty of fluids
is a simple measure many people overlook. Your diet can also affect constipation. Large quantities of dairy products such as milk, ice cream, cheese, and yogurt can contribute to
constipation. Fresh fruits and vegetables, whole grain cereals, nuts, and juices help prevent constipation by keeping the bowels active. Regular exercise also helps keep the bowels
Your doctor may prescribe a stool softener and/or a mild laxative especially if you are taking pain medication. Talk with your health care provider if you have not had a bowel movement
in two or more days. You may need a higher dose of laxative or an enema.
Hair Loss
Hair loss (alopecia) can be one of the most traumatic side effects of cancer treatment for
some people. From a medical standpoint, this side effect is considered minor since it does not cause any physical problems. However, it can be emotionally difficult to handle. Hair
loss may be a constant reminder of your illness. It also makes it apparent to the people you encounter every day that something is amiss.
Chemotherapy can cause hair loss by weakening the hair follicles. This causes the hair to fall
out at a much higher rate than normal. However, not all chemotherapy drugs used to treat lung cancer cause hair loss. Your health care provider can tell you if the drugs you are taking
are likely to cause hair loss. Whole brain radiation treatments can also cause hair loss.
Hair loss associated with cancer therapy varies. Some people experience only thinning of the hair on their heads. Others lose all the hair on their heads along with their eyebrows,
eyelashes, and other body hair. Hair loss from chemotherapy is not immediate. Most often, hair loss begins 2-6 weeks after chemotherapy has begun.
Treatment-related hair loss is usually not permanent. Hair lost during chemotherapy usually
grows back. However, it may grow back with a slightly different texture or color than the hair you lost. Hair lost because of radiation therapy also usually grows back, but it may not
grow back as thick as it was before your treatment. Hair regrowth after cancer treatment usually takes from 6 to 12 months.
While some people are not bothered by temporary hair loss, it is very upsetting to others.
Some people use a wig or hairpiece during treatment. Having a hairpiece or wig available before treatment begins may make it less traumatic when your hair begins to fall out. Select
local offices of the American Cancer Society have wigs available to loan. Hats and scarves are also options you may want to consider.
Mouth Sores and Other Oral Problems
Some chemotherapy drugs and whole brain radiation treatments for lung cancer cause mouth sores and other problems with your gums and teeth. The lining of the mouth is
normally replaced every 10-14 days. Therefore, the cells that make up the lining of the mouth must replace themselves rapidly. When certain chemotherapy drugs or radiation
treatments to the head are given, the division of these cells is slowed. When the lining of the mouth is shed, the slowed cell division makes it difficult to grow new tissue to replace it. As
a result, sores or ulcers can develop in the mouth. This condition is called mucositis or stomatitis. Mucositis usually begins approximately two weeks after treatment begins. It can
be very painful. The sores often heal slowly because cell production is decreased.
Open sores in the mouth can cause infections because the mouth is normally home to many
microscopic organisms. These tiny organisms do not usually cause problems because the lining of the mouth serves as a barrier, keeping them from invading the body. However,
open sores in the mouth can provide an entry point into the body for these organisms to invade and cause infection. This is particularly problematic for people receiving cancer
therapy because treatments can reduce your ability to fight infections.
Dry mouth is another common symptom in people being treated for lung cancer. This occurs when the salivary glands do not produce a normal amount of saliva (spit). Dry
mouth can cause any of the following symptoms.
• bleeding gums • a sore tongue • cracked lips and/or sores at the corners of the mouth • difficulty wearing dentures • altered sense of taste • difficulty swallowing • tooth decay
You can help avoid problems associated with cancer treatment by having your teeth cleaned before beginning therapy. It is best to have this done a month before beginning
chemotherapy or radiation treatments, if you have the time. This will give your mouth time to heal before treatment begins.
During treatment, the following practices can help you avoid or reduce mouth problems.
• Brush your teeth at least four times per day. Floss at least twice per day. • If possible, use toothpaste with fluoride to protect your teeth. If commercial
toothpaste burns your mouth, use a solution of ½ teaspoon of salt and 2 tablespoons
of baking soda in 8 ounces of warm water instead of toothpaste.
• Use a soft or extra-soft toothbrush to avoid small abrasions of the mouth and gums.
Children's toothbrushes are usually extra-soft.
• Apply fluoride gel to your teeth at bedtime.
• Rinse your mouth with a solution of ½ teaspoon of salt and 2 tablespoons of baking
soda in 8 ounces of warm water at least 4-6 times per day. Follow the solution with
a clear water rinse.
• Sip water or suck on ice chips throughout the day to reduce dryness. Adding a few
drops of food grade glycerin (glycerin USP) to your water will help the water
lubricate your mouth. You can also use glycerin swabs or a saliva substitute. Your health care provider can advise you about getting these items.
• Keep a spray bottle of water or water/glycerin solution nearby. Spray your mouth
whenever it feels dry.
• Chew sugarless gum or suck on sugarless hard candy to keep your mouth wet by
stimulating saliva production.
• Keep your lips moist with lip balm or petroleum jelly. Do not share these items with
other people as they can spread infections.
• Avoid spicy foods that may increase the burning sensation in your mouth. • Avoid carbonated beverages, orange juice, grapefruit juice, and acidic foods such as
citrus fruits, vinegar, pickled foods, and ketchup.
• Avoid salty foods that can dry your mouth and lips. • Avoid very hot liquids or foods that could burn your mouth or tongue. • Avoid alcohol in beverages, foods, or other products such as mouthwash or fluoride
rinses. Alcohol will cause burning and may increase the severity of mouth sores.
• Avoid eating foods with sharp edges that may scratch your mouth such as potato
chips, hard breads, and some crackers.
• Avoid smoking and/or chewing tobacco. • Eat foods that are soft, moist, and easy to chew. Yogurt, cooked cereals, rice, pasta,
potatoes, applesauce, pudding, cooked carrots, peas, cheeses, eggs, soups, and
casseroles are a few examples.
• Brush your teeth and rinse your mouth after eating foods or liquids with high sugar
People on chemotherapy whose white blood cell counts drop substantially may experience
an overgrowth of yeast in the mouth and/or throat. This is condition is called thrush. The
yeast often causes a white, beige, or yellowish coating on the tongue and/or gums. Eating active-culture yogurt or rinsing your mouth with hydrogen peroxide (3%) may help control
the growth and spread of thrush. Your doctor may prescribe an antifungal solution to gargle with, or antifungal medication to take by mouth.
Low Blood Counts (Myelosuppression)
Blood cells in the circulation come from the bone marrow, the soft center of the large bones in the body. Immature blood cells in the bone marrow produce red blood cells (RBCs),
white blood cells (WBCs), and platelets when they are needed in the circulation. Many chemotherapy drugs that kill cancer cells also interfere with the production of RBCs, WBCs,
and platelets. Reduced production of these cells is called myelosuppression. Low RBCs is called anemia. Low WBCs is called leukopenia or neutropenia. Low platelets is called
thrombocytopenia.
Myelosuppression can be caused by chemotherapy or radiation therapy. Radiation treatments for lung cancer usually cause only mild myelosuppression because the bones in
the treatment fields are responsible for only a small amount of the body's blood cell production. Myelosuppression associated with chemotherapy for lung cancer is often more
severe than that seen with radiation therapy. Myelosuppression is one of the major causes of reducing the dose of chemotherapy, altering the chemotherapy treatment schedule, or
stopping treatment altogether. Health care providers take myelosuppression very seriously because it can be life threatening. However, reducing the dose of chemotherapy drugs or
prolonging the interval between treatment cycles to allow the blood cell levels to return toward normal gives cancer cells time to grow and multiply.
Hematopoietic growth factors (HGFs) stimulate the bone marrow to increase production of blood cells. Therefore, HGFs are often given along with chemotherapy to maintain the
optimal dose and timing of chemotherapy. The three forms of myelosuppression are discussed on the following pages along with specific HGFs.
While anemia is one component of myelosuppression, there are other mechanisms for anemia related to lung cancer and its treatments. Please see the listing Anemia in
this section for a detailed discussion of this common cancer-related problem.
Leukopenia/Neutropenia/Granulocytopenia
Leukopenia is an abnormally low number of WBCs in the blood. Neutrophils are a specific type of WBC in a group of blood cells called granulocytes. Neutrophils play an
important role in fighting bacterial infections. An abnormally low number of neutrophils in the blood is called neutropenia. The term granulocytopenia is often used
interchangeably with neutropenia.
Granulocyte colony-stimulating factor (G-CSF, Neulasta®, Neupogen®) stimulates
the bone marrow to increase its production of granulocytes. This stimulation can help counteract the myelosuppressive effects of chemotherapeutic drugs, allowing
the full dose to be given according to schedule.
Anyone on chemotherapy is at increased risk for infections regardless of whether G-
CSF is also being taken. Therefore, you need to be aware of possible signs and symptoms of infection such as:
• fever greater than 100º F • chills or sweats • cough or sore throat • redness or swelling around skin sores or at injection sites • loose bowels or diarrhea • burning sensation during urination • unusual vaginal discharge or itching • feeling not quite "right"
Call your doctor immediately if you experience any of these signs or symptoms. If you cannot reach your doctor, go to your nearest emergency room.
There are steps you can take to reduce your risk of infection while on chemotherapy.
A list of precautionary measures includes:
• Avoid crowds and people with the flu or colds during the time your WBCs
are at their lowest. Ask your doctor or nurse when this is most likely to
occur with your treatment.
• Wash your hands frequently, especially before eating. • Eat fully cooked foods. Wash fresh fruits or vegetables well before eating
them. Peeling fruits can also reduce your risk.
• Use the hottest water cycle in your dishwasher. • Do not share towels, drinking glasses, or dishes with others.
Thrombocytopenia
Thrombocytopenia is an abnormally low number of platelets in the blood. Platelets are one of the elements necessary for blood clotting. Drugs that cause
myelosuppression can cause thrombocytopenia. A mild drop in your platelet count does not usually cause symptoms. Severely depressed platelet counts can cause easy
bruising, nosebleeds, bleeding from the gums, prolonged bleeding from minor cuts or scrapes, and/or a pinpoint rash of tiny purplish spots called petechiae. Contact
your health care provider immediately if you experience any of these signs or symptoms.
A transfusion of platelets may be needed if your platelet count drops significantly.
This will provide short-term relief of symptoms. The platelet growth factor oprelvekin (Neumega®) stimulates the production of platelets. It is usually given
only to people who have experienced dangerously low platelet levels in response to therapy.
Nausea and Vomiting
Many people have the idea that all chemotherapy causes severe nausea and vomiting. This is simply untrue. Not all chemotherapy drugs cause nausea and/or vomiting. Further, several
highly effective drugs are available to prevent and control nausea and vomiting associated
with chemotherapy. Fortunately, the days of uncontrollable nausea and vomiting associated
with chemotherapy are long gone.
Health care providers refer to the nausea and vomiting associated with chemotherapy as CINV (chemotherapy-induced nausea and vomiting). Different chemotherapy drugs have
different levels of risk for CINV. In general, a combination of drugs is more likely to cause CINV than is a single agent. CINV can be acute (occurring within the first 24 hours of
treatment) or delayed (occurring several days after treatment). The risk of CINV is predictable based on the drugs you are taking. Your health care provider will recommend
treatment that matches the risk profile of the drugs you are taking. Table 2 shows the risk of CINV associated with chemotherapy drugs commonly used to treat lung cancer. Drugs that
are FDA-approved for the treatment of small cell or non-small cell lung cancer appear in italics. However, your doctor may prescribe other drugs on the list. The choice of
chemotherapy drugs is individualized to meet your specific circumstances and needs.
Table 2: Risk of Chemotherapy-Induced Nausea & Vomiting (CINV)
Associated with Common Lung Cancer Chemotherapy Drugs
Generic Name
Trade Name
Risk of CINV
(without
medication)
carboplatin Paraplatin®
cisplatin Platinol®
moderate to high
doxorubicin Adriamycin®
moderate to high
fluorouracil 5-FU mild
ifosfamide Ifex®
irinotecan Camptosar®
methotrexate Mexate®
mitomycin Mutamycin®
vinblastine Velban®
vincristine Oncovin®
If there is a risk of CINV associated with your chemotherapy regimen, you will be pre-
medicated with drugs to prevent these side effects before chemotherapy is administered. It is much easier to prevent nausea and vomiting than it is to get it under control once it starts.
Often, a combination of drugs is used because combined treatment has been found to be more effective than use of any single drug.
Drugs currently used to control CINV are shown in the following list. The choice of drugs
used and their dosing will depend on your chemotherapy regimen.
alprazolam (Xanax®)
aprepitant (Emend®)
dexamethasone (Decadron®)
diphenhydramine (Benadryl®)
methylprednisolone (Medrol®)
dolasetron (Anzemet®)
dronabinol (Marinol®)
droperidol (Inapsine®)
prochlorperazine
In addition to medications, self-help techniques can be useful in controlling nausea and/or
• Eat small amounts throughout the day rather than three large meals. Filling your
stomach increases the likelihood of nausea and vomiting.
• Eat slowly and chew your food well. • Be sure you drink enough fluids. Dehydration can cause nausea and vomiting. • Avoid spicy and greasy foods. Greasy foods are hard to digest and stay in the
stomach for extended periods, sometimes up to 12 hours.
• If cooking odors bother you, eat cold meals or ask someone else to prepare your
meals and bring them to you on difficult days. Avoid foods with strong odors.
• If you feel nauseous, get some fresh air and take deep breaths. • Rinse your mouth often if it is dry or has a bad taste. • Suck on ice chips or hard candy.
Talk with your health care providers if you are having problems with nausea and/or
vomiting. Many options are available to control these symptoms effectively. There is no reason to suffer. If you are taking medication but are still experiencing breakthrough nausea
or vomiting, your treatment can be changed to another regimen that works better for you.
Peripheral Neuropathy
Some chemotherapy drugs can injure the peripheral nerves of the body, that is, those outside
the brain and spinal cord. The condition that results from damage to peripheral nerves is called peripheral neuropathy. While peripheral nerves are located throughout the body,
peripheral neuropathy usually affects only the hands and/or feet. There are many causes of peripheral neuropathy other than chemotherapy drugs.
Chemotherapy-induced peripheral neuropathy is usually experienced as:
• tingling, burning, or pain in the affected areas • loss of sensation (numbness) • loss of balance (if the feet are affected)
Peripheral neuropathy can cause clumsiness. Normal coordination depends on the
peripheral nerve messages to the brain telling it the position of your arms, legs, hands, and feet. Peripheral neuropathy can interrupt these messages. The result is clumsiness or loss of
coordination. Loss of information about the position of the limbs is called loss of position sense. You may have trouble buttoning your shirt without looking. You may also trip more
than usual or have a tendency to drop things.
Peripheral neuropathy is not a side effect of all chemotherapy drugs. Chemotherapy agents commonly used to treat lung cancer that can cause peripheral neuropathy include carboplatin
(Paraplatin®), cisplatin (Platinol®), paclitaxel (Taxol®), docetaxel (Taxotere®), etoposide (VePesid®), topotecan (Hycamtin®), vinblastine (Velban®), vincristine (Oncovin®),
vinorelbine (Navelbine®), and gemcitabine (Gemzar®). Of these drugs, peripheral neuropathy occurs most commonly with paclitaxel, docetaxel, cisplatin, and vincristine.
Peripheral neuropathy can occur at different times during the course of therapy depending
on the drug(s) being used. The toxic effects of chemotherapy on peripheral nerves are cumulative. This means once symptoms occur, they tend to get worse as additional
treatments are administered. In cases of severe peripheral neuropathy, the dosage of the chemotherapy drugs may have to be decreased. In rare instances, treatment with the
offending drug must be stopped. In most instances, chemotherapy-induced peripheral neuropathy gradually goes resolves after treatment has been completed. In some cases,
symptoms only partially resolve. There can be residual symptoms.
There is some evidence that peripheral neuropathy may be at least partially preventable.
Studies using the supplements glutamate15 and glutathione16 have shown some promise in
preventing or reducing the severity of chemotherapy-induced neuropathy. The drugs amifostine (Ethyol®) and carbamazepine (Tegretol®) have also shown promise in protecting
against chemotherapy-induced neuropathy.17, 18 However, no agents are currently in routine
use to prevent chemotherapy-induced peripheral neuropathy.
Loss of position sense can make you prone to injuries. Some simple measures can help
reduce the risk of injuries.
• Keep the rooms in your home well lit. When you have lost some position sense, the
brain automatically begins to rely on your other senses to help coordinate
movements. Good lighting helps give your brain good visual information.
• Keep a nightlight on to light your way should you need to get up during the night. • Wear shoes that tie, buckle, or have Velcro® fasteners instead of slip-on shoes. It is
easy to slip out of a shoe that is not firmly adhered to your foot. This can lead to falls and potential injuries. High heels should be avoided.
• Consider lowering the temperature on your hot water heater to avoid accidentally
burning yourself. Test bath water with your elbow before getting in the tub.
• Watch your hands when you are working with a sharp object. In this way, you are
using your eyes to provide information to your brain for what you may be lacking due to peripheral neuropathy.
• Consider having someone else drive for you if you experience numbness in your
• Use potholders or hot mitts if you are uncertain of the temperature of something
• Wear mittens or gloves to prevent frostbite in cold weather. Early symptoms of
frostbite are very similar to the symptoms of peripheral neuropathy and can be easily missed. Keep your feet warm and dry for the same reason.
• Use the railing when walking up or down stairs. Watch your feet.
Prescription medications are available that may help control the symptoms of peripheral
neuropathy. You may need to try more than one of these medications to find one that works for you. Options include topical lidocaine, gabapentin (Neurontin®), carbamazepine
(Tegretol®), phenytoin (Dilantin®), lamotrigine (Lamictal®), amitriptyline (Elavil®), and others. Over-the-counter and prescription pain relievers can also be used. The drug causing
the problem may need to be discontinued if your symptoms become severe.
Weight Loss
Weight loss is a common side effect of lung cancer treatments including surgery,
chemotherapy, and radiation therapy. The key factors in cancer treatment-related weight loss are:
• loss of appetite • nausea and/or vomiting • diarrhea • taste changes and/or sensitivity to odors • fatigue
Weight loss is discussed in detail in Symptoms Associated With Primary Lung Tumors in this
chapter. There are also suggestions for managing weight loss associated with lung cancer treatments included in Chapter 12: Nutrition and Lung Cancer.
PAIN CONTROL
Pain is one of the most feared symptoms of cancer. Chronic pain can significantly reduce
your quality of life and make even simple tasks seem overwhelming. Pain can be caused by the effects of cancer in your body or may be a side effect of treatment. Regardless of the
cause, good pain control is possible in nearly every situation. Many effective treatment options are available to control pain. Cancer pain has been well researched. Pain control
has become a sophisticated science. Many advances have been made in the field of pain management in recent years. Oncology doctors and nurses are well trained in the both the
assessment and treatment of pain.
The first step toward effective pain control is telling your doctor or nurse about your pain. Although this may seem obvious, many people do not tell their providers about their pain
until it becomes intolerable. Do not fall into the trap of thinking that telling your provider about your pain is a sign of weakness. Your health care team wants you to live your life as
fully and normally as possible. While pain is an important way for the body to let you know something is wrong, chronic pain serves no useful purpose and can significantly disrupt your
life. There is no reason to tolerate chronic pain in silence. Be sure to tell your health care provider about any new or changing pain you experience.
Pain often changes over time. The location and severity of pain can be highly variable.
Different types of pain require different treatments. In general, it is easier to achieve good pain control if the pain can be addressed early in its course rather than later when the pain
becomes severe. The treatments, drugs, and dosages of drugs used to control pain are individualized to your specific symptoms. The goals of pain management are to minimize
the experience of pain while limiting unwanted side effects from pain control treatments.
When you talk with your health care provider about your pain, you will need to describe your pain. This helps your provider decide how best to treat you. Consider keeping a log of
your pain, especially if your pain comes and goes. Important aspects of your pain should be recorded.
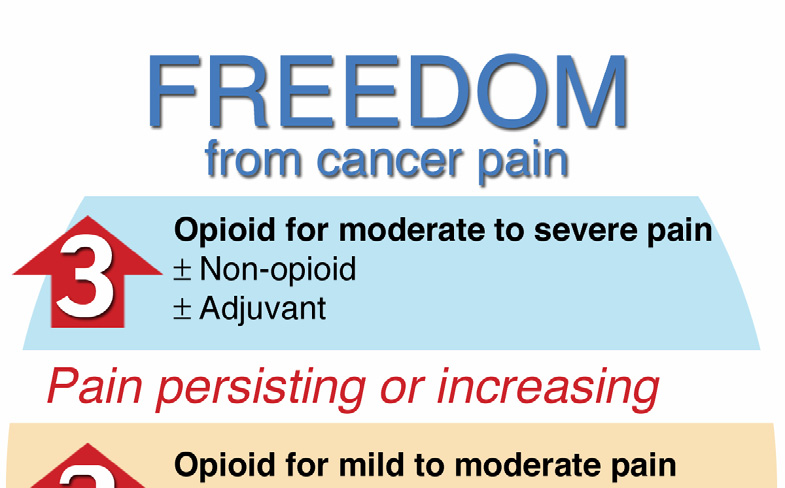
• Where is the pain located? • What does the pain feel like? (sharp, dull, achy, stabbing, burning, etc.) • What, if anything, brings on the pain? • What, if anything, alleviates the pain? • How long does the pain last? • On a scale of 1 to 10 (with 10 being the worst pain you've ever experienced), how
would you rate the pain?
The World Health Organization (WHO) developed a pain control model called the
Analgesic Ladder19, 20 (see Figure 2). Analgesic is another word for a pain relieving medicine.
The model helps providers rate pain and use appropriate medicines to control it. The WHO
approach instructs health care providers to match the intensity of pain with the potency of the drug: the more severe the pain, the stronger the pain reliever. Treatment of severe pain
does not begin at the bottom of the ladder. Strong pain relievers are given immediately. Combining low potency pain relievers with stronger pain relievers often increases pain
control. The goal is to maintain a constant level of pain relievers in the body so that pain cannot ‘break through.' In other words, pain medications are taken on a regular schedule
rather than only in response to pain. The three levels of the WHO Analgesic Ladder are summarized on the following pages.
Mild to Moderate Pain: 1-3 on a scale of 10
Non-opioids (drugs not related to morphine) are used. Examples include aspirin, acetaminophen
(Tylenol®), ibuprofen (Advil®, Motrin®, Nuprin®), naproxen (Naprosyn®), and others. Drugs such
as corticosteroids that are not pain relievers themselves are added if they help treat the
underlying cause of the pain. These drugs are referred to as adjuvants.
Figure 2: WHO Analgesic Ladder
for Pain Control
Copyright 2005 Nucleus Medical Art (www.nucleusinc.com). All rights reserved.
Moderate to Severe Pain: 4-6 on a scale of 10
People reporting moderate pain or people whose pain was not controlled using the measures from the lower step on the ladder should be treated with an opioid (a drug related to
morphine) for moderate pain. Drugs that may be used include codeine, hydrocodone (Vicodin®, Lortab®), dihydrocodeine (DHC), oxycodone (Percodan®, Percocet®, Tylox®,
Roxiprin®), propoxyphene (Darvon®, Darvocet®), and tramadol (Ultram®). Acetaminophen is often used with these drugs. Adjuvants are used to enhance pain control.
Severe Pain: 7-10 on a scale of 10
People who report severe pain or have not gotten sufficient pain relief from less potent medicines are treated with strong opioids. Morphine (MSIR, MS-Contin®, Roxanal®,
Oramorph-SR®), oxycodone (Oxycontin®, Roxicodone®), hydromorphone (Dilaudid®, Hydrostat®), levophanol (Levo-Dromoran®), methadone (Dolophine®, Methadose®), and
fentanyl (Duragesic®, Fentanyl Oralet®, Sublimase®, Innovar®) are examples of strong opioids. Non-opioid drugs and adjuvant drugs are also used to enhance pain control.
Pain control medications come in many forms including tablets, liquids, patches, suppositories, and solutions for injection. Your health care provider will work with you to
determine what form of pain medication works best for you.
Barriers to Pain Control
Misunderstandings and other factors can stand in the way of good pain control. Some
barriers to good pain control are related to concerns people with cancer have about pain medicines.
"I don't want to complain."
People are sometimes hesitant to tell their health care providers about their pain. You may be concerned about your doctor thinking you are a ‘complainer.' You may
worry that talking about your pain will make your providers think less of you. These concerns are understandable but misplaced. Keep in mind that one of your doctor's
jobs is to make you as comfortable as possible. Your health care providers cannot help you with your pain if they are not aware of it. You did not ask for your pain,
and you do not need to suffer in silence. Be open and honest with your doctors and
nurses when discussing your pain.
"I'm afraid I'll get addicted."
Many people worry about becoming addicted to pain medications. While people
who abuse pain relievers for recreational purposes may become addicted to them, people who use pain relievers to control pain rarely become addicted. This fact has
been proven in scientific studies.21-25 The dose needed to control your pain may need
to be gradually increases if you are on pain medicine for a prolonged period. This is
not an indication that you have become addicted to your pain medication. It is a normal body response called tolerance, which means your body requires more
medication to produce the same effect.
"I don't want to sleep all the time or feel doped-up."
Opioid pain medicines cause sleepiness when you first start taking them, but this side
effect only lasts a few days. Opioids can also cause you to feel somewhat odd, a feeling many people describe as being similar to being slightly intoxicated. However,
this side effect also diminishes over a few days. People who are in chronic pain usually find the side effects from opioid pain medicines are much less disruptive to
their lives than chronic pain is.
"If I start taking pain medicine now, there won't be anything left to treat my
pain if it gets worse later."
Opioid pain medicines do not lose their effectiveness over time. Your dose can be increased if your pain becomes more severe over time. There are always options
available for pain control regardless of how long you have been on pain medication.
"I don't want to give in to the cancer."
You may feel that admitting you are in pain is somehow giving in to your cancer.
This is not the case. Pain can interfere with your ability to sleep and eat normally. Sleep deprivation and poor nutrition can interfere with your quality of life and your
body's ability to respond to cancer treatment. Controlling pain improves your
quality of life and puts you in a better position to tolerate and respond to treatment.
Most health care providers working with people who have cancer are comfortable with assessing and treating pain. However, some are less adept at this aspect of cancer care than
others are. If your oncologist seems hesitant to prescribe pain medicines, ask him or her for a referral to someone who is more comfortable with this aspect of cancer care. Alternative,
talk with your oncology nurse or social worker about resources in your community. Many cities have pain management centers that specialize in the treatment of chronic pain. Pain
control is a very important part of cancer care, and should never be overlooked.
Non-Pharmacologic Pain Control Measures
There are pain control measures other than drugs that many people with cancer have found
helpful. Surgery may be used if a tumor is pressing on an organ or nerve causing pain. Radiation therapy can be highly effective for controlling bone pain. Several self-help
techniques may also be useful to you.
Biofeedback is a technique where a technician helps you learn to voluntarily relax your muscles. Pain often causes people to tense their muscles, which can worsen pain.
Biofeedback helps people take voluntary control over this response. Biofeedback is often used along with pain medications.
Visualization and imagery are techniques to help take your mind off your pain by focusing
on a pleasant mental picture. This distraction can cause relaxation, which may decrease the intensity of your pain. Less formal means of distraction such as watching a movie or
television or listening to music can be used to accomplish the same goal of taking the focus off the pain. Visualization and other distraction measures are often most effective when
used along with pain medicines.
Regular massages may help control your pain. Massage helps many people relax, which can reduce the intensity of their pain. No scientific studies have proven that massage is effective
for pain control, but many people find it helpful. Chapter 11: Complementary Healing has
additional information about these techniques.
There are many possible symptoms and side effects associated with lung cancer. Left
untreated, these symptoms can rob you of your quality of life and ability to function. Supportive care can have a very positive impact on your quality of life while living with lung
You are encouraged to discuss your symptoms with your health care providers as soon as they appear. Working together with your providers, you can eliminate or control nearly
every symptom caused by your lung cancer or its treatment. New supportive care treatment options are emerging every day. I hope you will benefit from these advances and enjoy your
life as symptom-free as possible.
Source: http://www.lungcancerguidebook.org/lcguidebook_aug05/ch10_0605.pdf
Single sell sheet.qxp
Product Data - DIO SERIES DIETS Report Repeat Revise The "Original" High-Fat Diets for Diet Induced ObesityFormulated by E. A. Ulman, Ph.D., Research Diets, Inc., 8/26/98 and 3/11/99. Research Diets, Inc. formulated the "original" high-fat diet for diet induced obesity (DIO) studies in 1996. Today, our high-fat diets are the research standard for DIO mice and rats worldwide.
Untitled
THE EFFECTS OF ADVERTISING USING GLOBAL APPEAL VS CHINA- SPECIFIC APPEALS: A STUDY OF CHINESE CONSUMERS IN HONG KONG AND CHINA Fung Sze Man A Project Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Arts in Communication Supervisor: Dr. Vivian Sheer