Hiv cure research_ advances and prospects
Contents lists available at
journal homepage:
HIV cure research: Advances and prospects
Caroline P. Passaes ,, Asier Sáez-Cirión
a Unité de Régulation des Infections Rétrovirales, Institut Pasteur, 25–28 rue du Dr Roux, 75724 Paris Cedex 15, Franceb CEA, Division of Immuno-Virology, iMETI/DSV, 18 Route du Panorama, 92265 Fontenay-aux-Roses, France
Thirty years after the identification of HIV, a cure for HIV infection is still to be achieved. Advances of
Received 14 February 2014
combined antiretroviral therapy (cART) in recent years have transformed HIV infection into a chronic
Returned to author for revisions
disease when treatment is available. However, in spite of the favorable outcomes provided by the newer
therapies, cART is not curative and patients are at risk of developing HIV-associated disorders. Moreover,
Accepted 20 February 2014
universal access to antiretroviral treatment is restricted by financial obstacles. This review discusses the
Available online 11 March 2014
most recent strategies that have been developed in the search for an HIV cure and to improve life quality
of people living with HIV.
& 2014 Elsevier Inc. All rights reserved.
EradicationRemission of HIV infectionHIV reservoirsReactivation of latent virusRepression of provirusControl of infection
avoiding drug resistance and side effects. Due to advances inantiretroviral development, HIV infection can nowadays be handled
The introduction of improved combined antiretroviral therapy
as a complex chronic disease ). Nonetheless,
(cART) has dramatically improved the clinical outcome and life
despite all of the clinical benefits provided by drug therapy, cART
expectancy of HIV infected patients. The development of drugs that
alone is not able to eradicate the virus, which persists in reservoirs
inhibit different steps of viral replication allows clinicians to success-
that are thought to be the source for viral reemergence after
fully manage the disease, improving immunologic parameters, and
treatment interruption (). Inaddition, cART does not fully restore health – it increases the risk ofnon-AIDS disorders such as cardiovascular, kidney, liver and neuro-logical diseases. Moreover, persistent immune dysfunction and
n Corresponding author. Tel.: þ33 145 688 944; fax: þ33 145 688 957.
inflammation increase the risk of non-AIDS morbidity and mortality
E-mail addresses:
(C.P. Passaes), . Sáez-Cirión).
0042-6822 & 2014 Elsevier Inc. All rights reserved.
C.P. Passaes, A. Sáez-Cirión / Virology 454-455 (2014) 340–352
a cure for HIV infection is needed to bypass the limitations of the
Is a cure for HIV possible?
current therapy and restore health. Although a vaccine against HIVremains an unachieved aspiration, several recent findings suggest
Since the isolation and characterization of the HIV as the
that either a cure or a durable remission of infection might be
etiologic agent of AIDS (the search
for a cure has been considered a major research priority. The
Berlin patient
Radio/chemotherapy
Total body irradiation
Detectable viremia
Boston patient A
Boston patient B
Fig. 1. Schematic representation of the clinical course before and after allogeneic hematopoietic stem cell transplantation (HSCT) in the Berlin (A) and the Boston patients(B and C) as described in and . The most important events associated to the HSCT and HIV disease are indicated. Blue arrowsrepresent the periods of radio/chemotherapy. Red arrows represent total body irradiation. Periods of detectable viremia are represented by orange boxes. The period thatpatients were under antiretroviral treatment are indicated in grey below the timeline. The period between allogeneic HSCT and ATI in Boston patients are indicated bybrackets. AML: acute myeloid leukemia; ATI: analytical treatment interruption; cART: combined antiretroviral therapy; HL: Hodgkin lymphoma; HSCT: hematopoietic stemcell transplantation; GVHD: graft-versus-host disease; WT: wild type.
C.P. Passaes, A. Sáez-Cirión / Virology 454-455 (2014) 340–352
description of a unique case of HIV cure after hematopoietic stem
and/or lymphomas ). Nevertheless, in most of these studies
cell (HSC) transplantation has boosted remarkable optimism in the
HIV was detected after transplantation, either following therapy
field and rekindled the hope that a cure for HIV infection is
withdrawal or because the therapeutic regimen was not able to
possible. In 2007, the so-called "Berlin patient" – HIV positive and
completely eliminate the viral reservoirs. In addition, in several cases,
diagnosed with acute myeloid leukemia – received double allo-
the patients died after transplantation. The most recent study
geneic HSC transplant from an HLA-matched and unrelated donor
investigating the impact of cART on viral reservoirs in two patients
screened for homozygosity for the CCR5 Δ32 allele (
who received HSC transplantation – known as "the Boston patients"
This patient discontinued ART the day before the first
– described an important reduction of HIV DNA in long term,
transplantation and, after 6 years of follow up in the absence of
reaching undetectable levels . These observa-
therapy, he shows no trace of HIV in blood and tissue samples
tions are in agreement with another study which described that HIV
(revealing no evidence for persistent HIV. Levels of HIV-
DNA levels at month 24 post transplantation in HSC transplanted
specific antibodies have also declined, suggesting that HIV antigen
patients are lower than those observed at baseline
stimulation was very low or absent after transplantation
Altogether, these data suggest that HSC transplantation in
association with cART may reduce viral reservoirs in HIV infected
Several studies have aimed to use autologous or allogeneic HSC
patients. However, a recent report during the 6th International
transplantation in association with antiretroviral therapy as a strategy
Workshop on HIV Persistence, Reservoirs and Eradication Strategies
to eradicate HIV in seropositive patients diagnosed with leukemia
revealed that the Boston patients experienced a strong rebound in
Table 1Hematopoietic stem cell transplantation in HIV positive patients
Diagnosis Graft type
Strategy against HIV infection Effect on HIV persistence
High-dose zidovudine for
No detectable HIV RNA and DNA at
Death 47 days after
2 weeks before transplantation. day 32 after transplantation and at
Lower maintenance dose
Zidovudine, IFN-alpha 2 and
No detectable HIV RNA at day 30
Death 10 months after
anti-HIV-1-specific T cell
after transplantation and at autopsy. transplantation.
cART before and after
No detectable HIV RNA on cART
Alive after 42 months of follow
transplantation, with
from day 210 after transplantation.
interruptions due to side-effects.
Autologous cART before and after
No detectable HIV RNA on cART in
Five patients were alive.
three patients who survived.
Autologous cART before and after
The four patients were alive
No detectable HIV RNA after
after 12 months of follow up.
transplantation (two patients),viral load rebound (two patients).
Detectable HIV DNA at month 12after transplantation for allpatients.
cART before and after
Undetectable RNA and DNA on cART. Death 191 days after
transplantation, with
Detectable HIV RNA and DNA at day transplantation.
interruptions due to side-
16 after TI.
Donor homozygous for CCR5
No cART. No trace of HIV after
Alive after 6 years of follow up.
6 years of follow-up.
Considered the first case of
Autologous cART before and after
Alive, immunologic
transplantation, with
Detectable HIV RNA and DNA after
characteristics comparable to
interruptions due to side-
HIV negative patients.
effects (n¼8).
HIV DNA significantly lower atmonth 24 than those at baseline.
Autologous cART before and after
Alive with undetectable VL by
transplantation, with
Detectable HIV RNA (9/10
conventional methods, but with
interruptions due to side-
patients) and DNA (10/10
detectable proviral DNA.
effects (n¼3).
patients) after transplantation.
cART before and after
Undetectable HIV RNA on cART,
Alive 5 and 3 years after
detectable after TI.
transplantation, but viremia
Detectable HIV DNA early after
rebounded after TI.
transplantation and undetectablein long term follow-up.
Donor homozygous for CCR5
No detectable HIV after treatment
Died 2 months after
Δ32 deletion.
transplantation by a severe
ALL: acute lymphoblastic leukemia; AML: Acute myeloid leukemia; BL: Burkitt lymphoma; BM: bone marrow; F: Female; HL: Hodgkin lymphoma; M: male; NHL: non-Hodgkin lymphoma; NA: not available; PBMC: Peripheral blood mononuclear cells; PCR: polymerase chain reaction; TI: treatment interruption; VL: viral load.
C.P. Passaes, A. Sáez-Cirión / Virology 454-455 (2014) 340–352
plasma viremia several months after analytic treatment interruption
(1% of caucasians) (), what makes the search for a
(ATI) and C) (http://es.scribd.com/doc/189931630/12-06-13-
compatible donor with the protective genotype an additional
suggest that HIV hides in yet unidentified sanctuaries or at levelsthat are not detectable by current available techniques.
So far, HSC transplantation to eradicate the virus was success-
How can HIV infected patients achieve durable remission of
ful only in the Berlin patient. The mechanisms involved in HIV
eradication in this patient are not yet fully understood. Thispatient underwent severe particular transplant conditions
"HIV controllers" or "elite controllers" correspond to a small
(), such as double HSC transplantation
percentage of HIV infected patients that can naturally control viral
from the same CCR5 Δ32 donor, conditioning regimen (total body
replication below the levels of detection with standard clinical
irradiation) and the development of graft-versus-host disease
assays. Consequently, this group of patients is considered an
(GVHD), which may have contributed to cure. Comparison with
important model to understand the mechanisms underlying con-
the protocols applied in the case of the Boston patients
trol of infection in the absence of treatment (
) suggests that total body irradiation or the engraft-
The aim of a so-called "functional
ment with cells from a CCR5 Δ32 donor may have been critical
cure" would be similarly to HIV controllers, that is, to allow HIV
differential aspects in the case of the Berlin patient. As the
infected patients to achieve viral remission in which HIV remains
homozygous CCR5 Δ32 deletion offers a natural resistance to
in the body at low levels and it is controlled by the host in the
HIV infection ), this unique successful experi-
absence of cART. This status may be achieved by 5–15% of patients
ence has encouraged the search for new CCR5-based therapeutic
treated very early during primary HIV infection (PHI) for long
approaches for HIV cure interventions (see below). It is interest-
periods of time who experience treatment interruption afterwards
ing to notice that the Berlin patient and both Boston patients
were originally heterozygous for the CCR5 Δ32 allele, but this did
not confer any advantage to the Boston patients once treatment
These patients are known as "post-
was interrupted (A
recent effort to cure HIV infection in a 12-year old boy with acute
The VISCONTI study (Viro-Immunological Sustained CONtrol after
lymphoblastic leukemia consisted of an allogenic transplantation
Treatment Interruption) investigated whether the characteristics of
of HSC obtained from cord blood. Similar to the Berlin patient, the
14 post-treatment controllers were similar to those observed in HIV
donor was screened for homozygosity for the CCR5 Δ32 allele.
controllers that spontaneously control HIV replication (
This procedure was performed at the University of Minnesota in
In this study, cART duration after primary infection was
April 2013, but the pediatric patient died two months after
3 years, and after treatment interruption, post-treatment controllers
transplantation by a severe GVHD (
presented a sustained control for a median of 7 years. During acute
phase, post-treatment controllers had higher viremia levels and
lower CD4þ T cell counts than patients who naturally control
Despite the impact of HSC transplantation on reducing HIV
infection afterwards. In addition, these groups of patients have a
reservoirs, this kind of treatment is not a viable option for the
different genetic background – while HIV controllers cohorts are
majority of HIV infected patients, since it is a risky and expensive
enriched by the protective HLA-B27 and B57
procedure that is recommended only for those who develop
the risk alleles B07 and
cancer. Furthermore, CCR5 Δ32 homozygous donors are rare
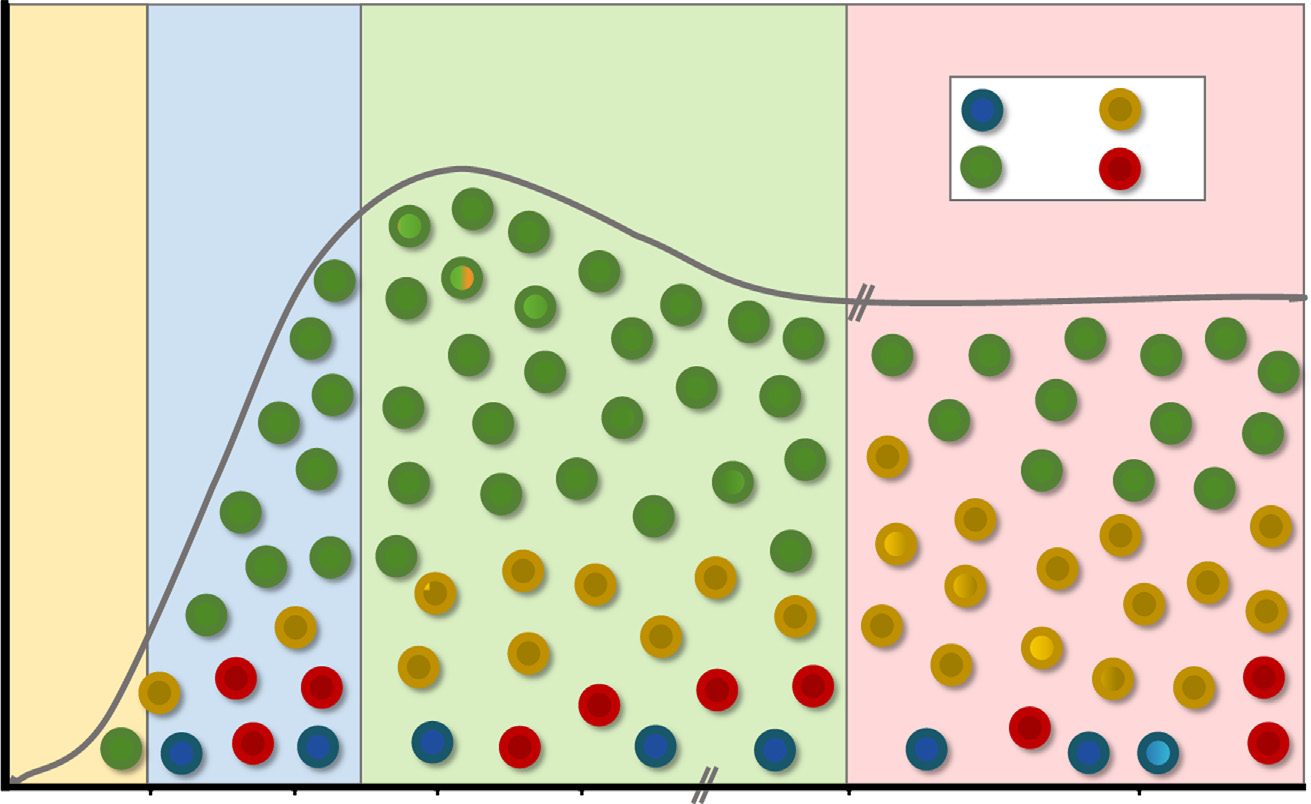
Fiebig I-III
Fiebig IV-V
infection
Naive TCM
HIV Reservoir
(T cell subsets)
Days after HIV infection
Fig. 2. Schematic representation of the HIV acute infection and the contribution of each T cell subset to the establishment of the HIV reservoir. Early treatment during Fiebigstages I–III may limit the number of infected cells and protect TCM cells from infection. Treatment during Fiebig stages IV-V may decrease the contribution of long-lived TNand TCM cells to the reservoir due to low relative abundance of these cell subsets. Frequency of TCM normalizes during chronic infection increasing the contribution of thesecells to the reservoir.
C.P. Passaes, A. Sáez-Cirión / Virology 454-455 (2014) 340–352
were prevalent among the 14 post-treatment
additional studies will be needed to understand the mechanisms
controllers. HIV-1 specific CD8þ T cell responses and immune
that may lead to a long-lasting viral remission in post-treatment
activation differ between post-treatment controllers and HIV con-
trollers (post-treatment controllers have weak CD8þ T cell responsesand a low level of immune activation during the control phase).
Another recent incident that suggests that a very early treat-
Is it better if we intensify ART?
ment may lead to HIV remission is the case identified as "theMississipi baby" (This infant born to a
Therapeutic intervention during PHI appears to be valuable
seropositive mother started receiving cART 30 h after birth. HIV-
in inducing viral remission in a certain number of HIV infected
1 RNA was detectable at 31 h, days 6, 11 and 19, and reached
patients. However, just a small percentage of patients are diag-
undetectable levels at day 29. cART was discontinued sometime
nosed during PHI. Most of them will know their seropositive status
between months 18 and 23. At 36 months of age and after therapy
only during the chronic phase of HIV infection. For the great
withdrawal, HIV-1 RNA, proviral DNA and HIV-1 antibodies remain
majority of HIV infected patients, other strategies to achieve viral
consistently undetectable or extremely low in blood and tissues in
remission must be developed. Combined antiretroviral therapy
this pediatric patient.
dramatically reduces viremia to levels below the detection limit of
The study of post-treatment controllers may give valuable
current assays ( o50 copies/mL), but low-level residual viremia
information to guide the search for a successful strategy for
persists and is usually detectable by ultra-sensitive tests in
inducing viral remission. However, some open questions remain.
patients undergoing successful ART ). Residual
For instance: which are the mechanisms underlying control? and
viremia may partially be the cause of persistent immune activation
how can we increase the probability of HIV infected patients to
), which increases the risk of non-AIDS
become a post-treatment controller? Recent studies suggest that
morbidity and mortality in treated patients
both the timing to initiate therapy (;
There are two probable sources of
residual viremia (i) long-lived, latently
and the duration of cART ()
infected cells whose provirus became transcriptionally active, with
might play a key role in the achievement of a durable HIV control.
intermittent or continuous viral release; and (ii) ongoing low-
In addition, baseline viral load and immune activation may predict
levels of HIV replication with de novo viral infection, due to partial
success (). Whether the therapeutic regi-
suppression and/or to inadequate drug penetration. In the latter
men used during PHI may impact the outcome is still to be
case, therapy intensification should reduce the residual viremia
investigated. In any case, in the absence of markers predicting
and associated persistent inflammation. Moreover, in the long
success after treatment interruption, this procedure is not recom-
term, it would be expected to decrease HIV reservoir levels.
mended outside structured protocols for patients undergoing
Previous studies of therapy intensification with protease and
suppressive cART.
reverse transcriptase inhibitors were contradictory in determining
Treatment during PHI seems to result in broad and strong HIV-
whether or not ongoing replication is the source of persistent
1 specific immune responses (
). The development of new classes of antiretroviral drugs
allowed the exploration of the impact of treatment intensification
activation (immune restoration in the
with drugs targeting other steps of HIV replication cycle. Treatment
gastrointestinal mucosa and limited viral
intensification with Raltegravir (RAL), a potent integrase inhibitor,
evolution Additionally, initiation of
offered a unique opportunity to study the dynamic of ongoing low-
cART during PHI may limit the establishment of viral reservoirs
level replication. As RAL blocks HIV integration, residual replication
could be assessed by the increase of 2-LTR circles (
). Central memory
Most studies of RAL treatment intensification showed no impact on
CD4 þ T cells (TCM) are a key component of the long-lasting HIV
residual viremia, immune activation or in promoting CD4þ T cell
reservoir and recent studies have demon-
reconstitution. Collectively, these data suggested that residual
strated that very early cART limits the seeding of the HIV reservoir
viremia does not originate from ongoing cycles of HIV replication
in long-lived TCM (Ananworanich et al., 2013. 20th
Conference on Retroviruses and Opportunistic Infections, San
). In contrast, the study
Francisco, USA). Reservoirs levels in post-treatment controllers
of Buzon et al. (identified a transient increase in the levels of
during the control phase were very low and it was mostly
2-LTR HIV DNA within two to four weeks after intensification, but
associated to the transitional memory CD4 þ T cell subset, due to
no significant decrease in low-level viremia was observed. In
a skewed distribution of quiescent CD4 þ T cell subsets in these
addition, only those patients with high levels of immune activation
at baseline presented a decrease in these markers. These findings
Treatment interruption in patients who started cART during
strongly suggested that RAL intensification was blocking new
chronic phase leads to viral rebound within weeks, with viral loads
rounds of infection in these patients and that consequently ongoing
frequently reaching pretreatment set-point levels (
replication was taking place. Nonetheless, other studies failed to
detect 2-LTR increase in RAL intensified-treated patients (
Notwithstanding, some patients that started cART during chronic
). It is possible that differences in
phase were also described to maintain controlled levels of viremia
patients' characteristics, cART regimens at baseline, and/or the time
after therapy discontinuation ). For all these
of therapy intensification with RAL had an impact in the discre-
studies describing cases of a potential "functional cure", long
pancies observed among these studies. An important observation in
period follow-up is needed to evaluate whether long HIV control
the Buzon et al., study was the fact that 61% of the patients with
can be maintained and the mechanisms involved in the long-term
detectable 2-LTR were taking a protease inhibitor-based regimen
suppression after treatment interruption. Collectively, these stu-
(PI). More recently, Hatano and colleagues also detected the
dies suggest that HIV remission is possible to be achieved with the
transient increase of 2-LTR, which was also more accentuated in
help of therapeutic interventions in patients without a favorable
patients taking PI In addition, a significant
genetic background to naturally control HIV infection. Certainly,
reduction in D-Dimer levels, a coagulation biomarker, was observed,
C.P. Passaes, A. Sáez-Cirión / Virology 454-455 (2014) 340–352
indicating that RAL intensification may lead to reduction in inflam-
had many undesirable effects, associated with exacerbated
immune activation and cytokine release, induction of anti-OKT3
Because HIV-1 might replicate in tissue reservoirs where drug
antibodies and severe long-lasting depletion of CD4 þ T cells
concentrations are suboptimal (such as
lymph nodes, gut associated lymphoid tissues, bone marrow and
HDAC inhibitors were next proposed as optimal candidate to
the central nervous system, some RAL intensification studies
flush HIV reservoirs due to their potential to activate HIV transcrip-
assessed the immunologic and virologic responses in tissues. Yukl
tion without inducing generalized immune activation. Chromatin
et al., showed reduction in unspliced HIV RNA, T cell activation and
condensation is regulated by the level of acetylation/deacetylation
a trend towards CD4 þ T cell increases in ileum, suggesting that
of the histones that constitute the core of the nucleosomes. Histone
this tissue may be an important site for ongoing replication in
acetyl transferases (HAT) mediate the addition of acetyl groups to
some patients on cART ). In contrast, therapy
histones, reducing chromatin condensation and promoting tran-
intensification with RAL did not impact cerebrospinal viral loads
scription. Histone deacetylases (HDAC) remove the acetyl groups
or isolated HIV semen shedding (
and repress transcription. The balance of HAT/HDAC activities is
thus thought to be a key component of HIV latency. The first
Based on previous observations that Maraviroc (MVC), a CCR5
molecule with HDAC inhibitory activity to be assayed in vivo was
antagonist, promotes a gain of CD4þ T cells in viremic HIV-infected
valproic acid (VPA). A first study reported a decrease in the
patients it was hypothesized
frequency of circulating resting CD4þ T cells carrying replication
that the immunomodulatory effects of this drug could decrease
competent HIV-1 in four patients receiving cART after 16 weeks of
immune activation and improve CD4þ T cell counts in patients under
additional treatment with VPA ). However,
suppressive cART with insufficient immunological restoration. As
subsequent randomized clinical studies could not confirm these
observed in RAL intensification trials, no impact in residual viremia
results and no significant effects of VPA were evidenced
or HIV reservoir was achieved. Data regarding CD4þ T cell gain was
also controversial in these trials
Failure of VPA was eventually associated to a poor capacity of
). Some unexpected effects,
this molecule to inhibit HDAC3, the HDAC isoform that is thought to
however, were observed in MVC intensification trials, such as
play a preponderant role in HIV latency (). In a
increased activation levels in blood and rectal mucosa
proof of concept study, the more potent HDAC inhibitor vorinostat
increase in plasma LPS, sCD14 and sCD163
has shown capacity to increase levels of HIV mRNA transcripts after
) and increased 2-LTR levels
a single dose, without affecting overall HIV DNA cellular levels
suggesting that MVC intensification might
(). Preliminary results of the NCT01365065 trial
induce viral replication. The mechanisms underlying these effects
presented in the 20th Conference on Retrovirus and Opportunistic
are still unclear, but some evidences suggest that MVC promotes an
Infections (.) also reported an increase of cell
increase in the circulating levels of CCL3 (MIP-1α), CCL4 (MIP-1β) and
associated unspliced HIV mRNAs in 15/17 patients on cART who
CCL5 (RANTES), natural ligands of CCR5, which may activate T cells
received daily doses of vorinostat for 14 days. Another clinical trial
and monocytes/neutrophils through CCR3/CCR4 and CCR1 signaling,
(NCT01680094) is evaluating the impact on HIV reservoirs of
respectively ). Further studies are
panobinostat, which has been described as an even more potent
necessary to carefully evaluate the immunomodulatory effects of MVC
HDAC inhibitor ().
in vivo and the benefits of therapy intensification with CCR5 antago-
The use of HDAC inhibitors in the context of HIV cure face several
nists in HIV-infected patients.
hurdles. Among them, the lack of specificity of HDAC inhibitors may
Despite some evidence that therapy intensification may have
impact the transcription of a large fraction of all cellular genes
positive effects on residual replication, its potential to eradicate
(). Also, it has been recently shown
the virus appears limited. These results highlight the importance
that viral reactivation with HDAC inhibitors will not necessarily
of designing new strategies to eliminate persistent HIV reservoirs.
be followed by viral-induced cell death, and that immune responsesmay need to be boosted in parallel to recognize and eliminate thesenew viral-producing cells (see below). It is also unlikely that HDAC
HIV persistence as a challenge for a cure
inhibition by itself will be able to induce efficient viral reactivation inthe absence of the factors necessary to ensure full viral transcription.
HIV replication and persistence depend on the integration of
The current belief is that it will be necessary to combine treatment of
the viral DNA in the host genome. Although most proviruses
HDAC inhibitors with other molecules able to provide the additional
integrate in transcriptionally active genomic regions, in most cases
stimuli required for HIV transcription. PKC agonists, such as prostra-
these proviruses remained repressed Our knowl-
tin ) and bryostatin
edge of the complex mechanisms underlying establishment and
), or TLR agonists that activate NF-kB
maintenance of HIV latency has been enormously improved in the
have been proposed as good potential combinatorial candidates.
last years (see for a thorough
Purging viral reservoirs is undoubtedly the only solution to
review). Repressed HIV proviruses integrated in long-lived cells
achieve HIV eradication. However, letting aside the mechanistic
constitute the persistent HIV reservoir, which is not recognized by
issues, activating every single latently infected cell in the organism
immune responses, not eliminated under cART, and is the main
still appears a gargantuan endeavor. Taking the example of natural
obstacle to achieving an HIV cure. Since the description of HIV
HIV controllers or the post-treatment controllers from the VISCONTI
reservoirs despite long-term cART, attempts to purge this reservoir
study, durable HIV remission may be a more reasonable goal in the
have been tried. The first one consisted in the infusion in three
medium term. In this setting, limiting and controlling the viral
patients under cART of the anti-CD3 OKT3 antibody in the
reservoirs would be the main objectives. With this in mind, our
presence of IL2, in an effort to mimic in vivo a well-established
current knowledge, albeit incomplete, of HIV latency and transcrip-
in vitro reactivation protocol ). OKT3 þIL2
tion might be turned to devise strategies aiming to repress, rather
treatment was accompanied by very strong activation of T cells,
than activate, viral transcription. As alternatives to HDAC inhibitors,
and transient increases of HIV RNA levels were observed in plasma
HAT inhibitors such as garcinol derivatives )
or lymph nodes of these patients. However, no decrease in the
and curcumin have been shown to inhibit HIV
frequency of infected cells could be reported and the treatment
transcription in vitro. Transcriptional elongation of the viral
C.P. Passaes, A. Sáez-Cirión / Virology 454-455 (2014) 340–352
promoter depends on the recruitment of the HIV transactivator
the mammalian target of rapamycin (mTOR), a protein kinase that
factor Tat to the transactivation-responsive element (TAR) located at
control cell cycle, proliferation and survival, and plays a critical
the end of initial HIV transcripts ).
role in the differentiation of T cells. Rapamycin has been shown to
Compounds such as Celastrol ) directly block
be able to block HIV infection in vitro ) by
Tat function by altering its structure. An analogue of Cortistatin A, a
decreasing the expression of CCR5, and also interferes with the
natural steroidal alkaloid, has shown to block HIV transcription
synthesis of HIV transcripts ). Through its capacity
initiation and elongation by binding specifically to the TAR-binding
to suppress activation and proliferation of T cells, rapamycin has
domain of Tat and impairing the interaction of Tat with viral RNAs
also the potential to block HIV infection by reducing the number of
. This promising molecule showed potent
target cells and to dodge the maintenance of viral reservoirs
inhibitory capacity in vitro at very low concentrations (nM-pM).
through homeostatic proliferation. Rapamycin is commonly used
Zinc-finger domains, small protein domains that can be designed to
to avoid organ rejection in kidney transplantation when there are
bind specific DNA sequences, can be fused to appropriate effector
complications associated with calcineurin inhibitors. Interestingly,
domains of transcription factors to specifically regulate the expres-
a clinical report on a group of 14 HIV infected patients who
sion of targeted genes. Zinc-finger transcription factors targeting
received kidney transplantation showed that the patients who
different regions of the LTR promoter and carrying the repression
switched to rapamycin monotherapy after transplantation were
domain of the KOX1 protein were able to repress transcription from
able to better control HIV replication than those who kept
the LTR in infected cells in vitro ). Overall these
calcineurin inhibitors Another recent
results suggest that different opportunities exist and may be
study, which analyzed a larger group of HIV-infected kidney
exploited to specifically repress HIV transcription.
recipients, has shown that those who received rapamycin experi-enced, two years after transplantation, some reduction in thelevels of cell associated DNA when compared to patients receiving
other immunosuppresors
Another compound with cytostatic activities that has been tried
The apparent cure of the Berlin patient after receiving HSCT from
in the context of HIV infection is hydroxyurea. Hydroxyurea is an
a CCR5Δ32 homozygous donor and the impossibility of applying this
inhibitor of ribonucleotide reductase (RNR) a key
protocol in a large scale have inspired attempts to generate HIV-
enzyme responsible for dNTP synthesis that has been shown to play
resistant cells through gene therapy One of
an important role in regulating HIV infection (
the most promising gene therapy strategies against HIV infection
Hydroxyurea, other than maintaining cells in a quiescent state,
aims to disrupt the CCR5 gene by expressing an engineered zinc-
reduces the levels of intracellular dNTPs thus inhibiting HIV DNA
finger nuclease (ZFN). Evidence that ZFN could inactivate CCR5 in
synthesis during reverse transcription. Although the impact of
primary human CD4þ T cells and in CD34þ hematopoietic stem
hydroxyurea in HIV reservoirs has not been evaluated, hydroxyurea
cells limiting HIV replication was first obtained in mouse models
was shown to act synergically with the nucleoside analogue dida-
The results of a Phase I clinical
nosine to reduce HIV viral loads in patients
trial showed that HIV-infected patients treated with ZFN CCR5
. Despite its promises, hydroxyurea treatment was
modified CD4þ T cells (SB-728-T) have sustained increases in the
shown to provoke complications, such as blunted CD4þ T cell
CD4þ T cells, mostly TCM and TTM with low PD-1 expression. Viremia
recovery and severe toxicity, in HIV infected patients (
was controlled after treatment interruption for some patients, but
). Recent studies suggest that these undesirable
cART was resumed by most of them due to dual-tropic infection or
effects were due to a too high dose of the drug, and that both the
viral load rebound Phase II clinical trials are
antiviral and the cytostatic activities of hydroxyurea may contribute
currently ongoing to evaluate the efficacy of SB-728-T. In a recent
to control HIV when used at lower concentrations (
development of these studies, ZFNs have been designed to be
JQ1 is an agonist of the bromodomain protein BRD4, which
combined and simultaneously target CCR5 and CXCR4. This approach
promotes cell cycle progression (BRD4 is also a
resulted in human primary CD4þ T cells that were resistant to R5
positive regulator of P-TEFb that competes with Tat for binding to
and X4 viruses in vitro and also in vivo when introduced in
this complex at the HIV promoter ). JQ1
humanized mice ). This strategy would tackle
dissociates BRD4 from the HIV promoter and allows Tat recruit-
the risk of tropism switching.
ment and subsequent HIV elongation In addition,
Other strategies consist of transducing CD34þ or CD4þ T cells
JQ1 appears also to alter chromatin organization and downregu-
with vectors expressing (i) shRNA interfering with CCR5 or other key
lates T cell activation genes ).
factors associated with the HIV life cycle including
A different strategy has been explored with auranofin, a gold-
its promoter ); and (ii) small peptides with capacity
based compound that has been evaluated in vivo in SIV infected
to inhibit HIV entry into the cells ). Another
macaques. This compound was shown in vitro to promote differ-
encouraging gene therapy approach directly targets the viral reservoir
entiation of CD27 þ memory CD4þ T cells to more terminal short-
and is based on the ability of a tailored site-specific recombinase (Tre)
lived stages () preceding increased cell death.
to excise HIV provirus from host genome ). Recently,
Administration of auranofin to a group of SIVmac251 infected
successful expression of Tre-recombinase in human cells was demon-
rhesus macaques with viral loads suppressed by cART, induced
strated. In addition, an important antiviral effect was observed in
indeed a decreased in the frequency of TCM and TTM CD4þ T cells,
humanized mice, suggesting that this approach may be valuable for
the cells thought to contribute the most to persistent reservoirs
future HIV eradication strategies
). Interestingly, auranofin treatment wasaccompanied by a transient decrease of viral reservoirs and adelayed rebound of viremia after interruption of auranofin and
Innovative approaches to eliminate HIV reservoirs
antiretroviral treatment (In a follow-up study,auranofin treatment in two macaques combined with cART and
Several experimental and proof-of-concept studies aim to
buthionine sulfoximine, a glutathione-depleting agent that has
interfere with cell cycle and survival of HIV infected cells to
been proposed to favor selective death of infected cells in vitro
facilitate their elimination or avoid their persistence by homeo-
favored control of infection at relatively low
static proliferation. Rapamycin is an immunosuppresor that blocks
levels after treatment interruption (
C.P. Passaes, A. Sáez-Cirión / Virology 454-455 (2014) 340–352
How these interventions may impact (positively or negatively)
due to the dual role that IFNα (and immune activation) may play at
T cell immune defenses against HIV has not been thoroughly
different stages of infection.
addressed, and the translation of current formulations of these
Immune activation is a major determinant of HIV pathogenesis,
drugs to clinical intervention is unlikely due to toxicity and
and increased levels of inflammation markers are associated with
possible harmful unspecific effects. However, the proof-of-
faster progression to disease and CD4þ T cell loss
principle studies described above suggest that targeting T cell
) including in HIV controllers with undetectable viremia (
proliferation and survival deserves further attention in the search
). Therefore, targeting the harmful
for an HIV cure.
immune activation appears to be a necessary element in ensuring along-life remission of HIV infection. Some of the molecules target-ing HIV reservoirs described in this review have also immunosup-pressive effects, and their impact is being evaluated. Other
Immunotherapies to treat HIV infection
molecules such as chloroquine analogues or statins specificallytarget inflammation. So far, studies employing these and other
There is a consensus in the scientific community on the need to
anti-inflammatory molecules have rendered contrasting results
potentiate immune responses in the context of combinatory
(). Thus, chloroquine administration has been shown
approaches to reach an HIV cure. Such responses would contribute
to decrease levels of T cell activation but
to either control or eliminate HIV infected cells. A study performed
produce faster CD4þ T cell loss when used for longer periods of
by the Siliciano group showed that reactivation of latent viruses
time (). A better knowledge of the best timing to
would not automatically entail the elimination of the infected cells
implement interventions aimed at decreasing persistent immune
by viral-replication-driven apoptosis (). Efficient
activation is warranted.
CD8 þ T cell responses, such as those found in HIV controllers,react to very small amounts of antigens and eliminate HIVproducing cells (
Concluding remarks
In contrast, responses from non-controllerpatients would not have such capacity. Anti-exhaustion strategies
Achieving HIV cure at a global scale through the eradication of
try to reverse negative signaling provided by immunoregulatory
HIV reservoirs seems still far off. In contrast, durable HIV remission
molecules such as PD-1 to restore T cell function, in particular,
with low levels of infected cells being controlled by host mechan-
the capacity to kill infected cells ().
isms seems more plausible at medium-term horizon. The first step
Blockage of PD-1 interactions with PD-1 ligands on SIV-infected
in such strategy would be to limit the size of the viral reservoirs.
macaques resulted in the expansion of CD8 þ T cells with
Early treatment initiation has been shown to provide immunolo-
improved functionality, longer survival, lower viral loads and
gical and virological benefits to HIV infected patients, and early
delayed viral rebound after antiretroviral treatment interruption
treated patients may be more prone to positively respond to cure
). However, another report suggests that mere
therapies. Moreover, treatment is prevention ()
expansion of polyfunctional CD8 þ T cell responses through PD-1
and, thus, early diagnosis and treatment initiation appears as a
blockade may not suffice to sustainably decrease viremia
priority in the global fight against HIV. Approaches trying to purge
A key aspect may be the association of
the viral reservoirs, including activation with HDAC inhibitors or
the efficient responses found in HIV controllers with the selection
PKC agonists face the difficulty of trying to circumvent complex
of particular TCR clonotypes in these cells. In this sense, PD-1
mechanisms of repression with non-specific drugs that may cause
blockade may be a useful adjuvant in vaccination protocols
undesirable effects. An alternative strategy may be to further
) helping to induce efficient responses. This
reinforce latency and repression mechanisms with specific mole-
review will not summarize therapeutic vaccine strategies cur-
cules targeting Tat-dependent transcription of HIV products. Gene
rently in development. However, recent results showing that (i)
therapy offers also the possibility to target specific genes to render
non-conventional CD8 þ T cell responses were associated with
cells resistant to HIV infection and even to excise integrated
control of infection and viral clearance in a group of macaques
provirus. Enhancing susceptibility to apoptosis of HIV infected
vaccinated with a cytomegalovirus vector
cells or impairing homoeostatic proliferation and persistence of
) despite profound viral dissemination during
these cells are also proposed as potential strategies to tackle HIV
primary infection; and that (ii) passive transfer of broadly neu-
reservoirs. However, such approaches need to carefully evaluate
tralising antibodies allows control of infection in chronically SIV-
the impact they may have in immune responses of treated
infected macaques ), suggest that therapeutic
individuals. HIV remission will require efficient host responses to
vaccines should be an important element in the global plan to
control infected cells and to prevent harmful HIV-related inflam-
achieve HIV cure or remission.
mation. These areas of research need to be explore in parallel to
So far, interventions based on the administration of gamma-
strategies targeting the reservoirs.
chain cytokines such as IL-2, IL-7 or IL-15, which tried to improve Tcell function and restore T cell homeostasis
),have not shown, at least by themselves, significant benefits in HIVtreatment. Indeed, improved immune reconstitution with IL-7 is
Our work receives financial support from the ANRS, Sidaction,
also accompanied by a significant increase in the total number of
amfAR and Total Foundation. C.P.B.P. has postdoctoral funding
HIV-harbouring CD4 þ T cells
from the ANRS.
). It is not excluded, however, that these cytokines mayhave an important adjuvant effect in vaccine strategies. Therapies
based on IFNα administration have been shown to decreaseviremia during chronic infection and reduce viral reservoirs after
treatment interruption (
However, these effects were not observed in all
situations (which may be
C.P. Passaes, A. Sáez-Cirión / Virology 454-455 (2014) 340–352
Ananworanich J., Vandergeeten C., Chomchey N., Chomont N., Early ART interven-
tion restricts the seeding of the HIV reservoir in long-lived central memory CD4
T cells., 20th Conference on Retroviruses and Opportunistic Infections, 2013,
Atlanta, GA, USA.
Ando D., Lalezari J., Blick G., Rodriquez, J., Hsu R., Hawkins T., Parks D., Zeidan J.,
Sekaly R-P., Deeks S., Functional Control of Viremia in CCR5-Δ32 Heterozygous
(Δ32HZ) HIV+ Subjects Following Adoptive Transfer of Zinc Finger Nuclease
CCR5 Modified Autologous CD4 T-cells (SB-728-T). 53rd Interscience Confer-
ence on Antimicrobial Agents and Chemotherapy, 2013, Denver, CO, USA.
C.P. Passaes, A. Sáez-Cirión / Virology 454-455 (2014) 340–352
Elliott J., Solomon A., Wightman F., Smith M., Palmer S., Prince M., Watson J., Hoy J.,
McMahon J, Lewin S.R., The safety and effect of multiple doses of Vorinostat on
HIV transcription in HIV-infected patients receiving combination antiretroviral
therapy., 20th Conference on Retroviruses and Opportunistic Infections, 2013,
Atlanta, GA, USA.
C.P. Passaes, A. Sáez-Cirión / Virology 454-455 (2014) 340–352
Mbonye, U., Karn, J., Transcriptional control of HIV latency: Cellular signaling
pathways, epigenetics, happenstance and the hope for a cure. Virology,
C.P. Passaes, A. Sáez-Cirión / Virology 454-455 (2014) 340–352
Stock P., Barin B., Hatano H., Rogers R., Roland M., Lee T.-H., Busch M., Deeks S.,
Impact of immunosuppressive therapies on HIV persistence during kidney
transplantation. 2013, 19th International AIDS conference, Kuala Lumpur,
C.P. Passaes, A. Sáez-Cirión / Virology 454-455 (2014) 340–352
Source: http://israb.se/wp-content/uploads/2016/03/Cure-for-HIV-1.pdf
u-f-s.eu
Le Mot de la Présidente . 3 Editorial du Consul Général. 5 Une affaire de frères . 7 Rétrospective des évènements de l'année 2013.11 Parmi les évènements de l'année, une première .12 Informations utiles .13 L'école française de Sarrebruck et Dilling.14 Des nouvelles de l'AFDES .17 Gingko Biloba.18 Décorations .21 Un mémorable anniversaire .23
physioinfo.co.za
Management of Patellofemoral PainTargeting Hip, Pelvis, and Trunk MuscleFunction: 2 Case Reports Catherine L. Mascal, PT, BSc1Robert Landel, DPT, OCS2Christopher Powers, PT, PhD3 Study Design: Case report.Objective: To describe an alternative treatment approach for patellofemoral pain.Background: Weakness of the hip, pelvis, and trunk musculature has been hypothesized toinfluence lower-limb alignment and contribute to patellofemoral pain. Two patients who had a