Untitled
Management of Concussionand Post-Concussion Syndrome
Barry Willer, PhD*
John J. Leddy, MD
Address
*University at Buffalo, G 96 Farber Hall, 3435 Main Street,
Buffalo, NY 14214, USA.
E-mail: [email protected]
Current Treatment Options in Neurology 2006, Current Science Inc. ISSN 1092–8480
Copyright 2006 by Current Science Inc.
Concussion and mild traumatic brain injury (mTBI) are common clinical problems. However, the literature is not consistent in defining how concussion and mTBI are related. Although most patients with concussion recover within days to weeks, approximately 10% develop persistent signs and symptoms of post-concussion syndrome (PCS). There are no scientifically established treatments for concussion or PCS and thus rest and cognitive rehabilitation are traditionally applied, with limited effectiveness. This article presents a clinical model to suggest that concussion evolves to become mTBI after PCS has developed, representing a more severe form of brain injury. The basic pathophysiology of concussion is presented, followed by a recommended approach to the clinical evaluation of concussion in the emergency department and the physician's office. We evaluate the limited evidence-based pharmacologic treatment of acute concussion symptoms and PCS symptoms and also discuss return to activity recommendations, with an emphasis on athletes. Lastly, we suggest a promising new direction for helping patients recover from PCS.
Estimates of the number of individuals experiencing a ment. One purpose of this paper is to provide a frame- brain injury in the United States vary from 1.5 to 2 mil- work for understanding concussion and how it fits into lion each year [1, Class II]. Most of these injuries the continuum of injury to the brain. A second purpose (approximately 85%) are considered mild, but they is to provide a brief explanation of the pathophysiology may have long-term effects [2, Class II]. These estimates of brain injury. The final goal is to provide a description do not include concussions in which an individual did of current treatment options and likely directions for not sustain loss of consciousness (LOC) but which future treatment given our increasing understanding of nonetheless may affect the individual's health for 1 the pathophysiology of concussion.
week or more. Most individuals with concussion The most commonly accepted definition of mTBI is (approximately 75%) do not seek attention from a that of the Centers for Disease Control and Prevention medical facility or medical practitioner unless the symp- (CDC) and the American Congress of Rehabilitation toms worsen or persist.
Medicine: loss of consciousness for no more than 30 There is uncertainty about the definitions of mild minutes or amnesia as a result of a mechanical force to traumatic brain injury (mTBI) and concussion. There is the head, and a Glasgow Coma Scale (GCS) score of 13 further uncertainty about the definition of post-concus- to 15 [3••, Class III]. The most commonly accepted sion syndrome (PCS) and the cause and treatment of definition of concussion, developed by the American PCS. Although there has been much research on and Academy of Neurology (AAN), is a trauma-induced increased understanding of the pathophysiology of con- alteration in mental status that may or may not involve cussion and mTBI, there is need for a model to clarify loss of consciousness [4, Class III]. Although not explic- the diagnosis of each and ultimately a model for treat- itly stated in the AAN definition, there is the assumption
Psychiatric Manifestations of Neurologic Disease
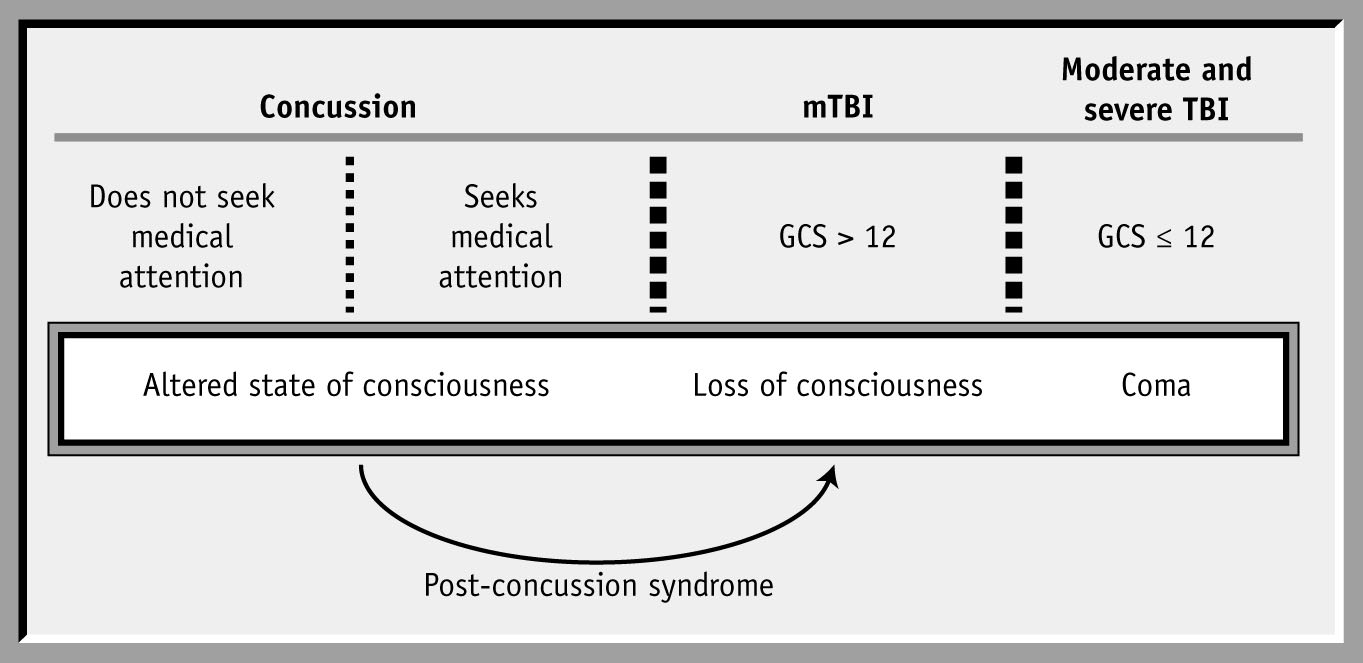
Figure 1. A model to describe the levels of
head injury from concussion (temporary
alteration of consciousness) to severe
(permanent brain damage). Concussion
effects are assumed to be transient with
signs and symptoms that do not last more
than 3 weeks. If signs and symptoms per-
sist beyond 3 weeks, then the diagnosis is
altered to reflect the more permanent
nature of the injury: post-concussion syn-
drome. Individuals with post-concussion
syndrome are more accurately diagnosed
as mild traumatic brain injury (mTBI).
GCS—Glasgow Coma Scale.
that concussion effects are transient, whereas mTBI is
damaged brain is borne out by recent animal research
considered permanent or semi-permanent. The use of
[7, Class II].
the different terms, mTBI and concussion, to describe
Individuals who experience symptoms for more
the same injury is confusing for clinicians. Instead, clini-
than 15 minutes or experience a brief loss of conscious-
cians tend to use the term concussion to describe
ness, convulsions, or vomiting as a result of a concus-
instances in which an individual experiences transient
sion are much more likely to seek immediate attention.
alteration in mental status, especially from a sports-
These levels of concussion correspond to grades 2 and 3
related head injury. mTBI is used to categorize patients
of the AAN guidelines. Recent research indicates there is
with more serious head injury in which there was a
little point in distinguishing between grade 2 and 3 con-
(brief) loss of consciousness and a GCS score of 13 or 14
cussions because there is no apparent prognostic value
at some point after the injury.
[8, Class II]. For our purposes, such a concussion
Figure 1 describes the continuum of injury to the
becomes an mTBI if the loss of consciousness exceeds 5
brain as experienced by individuals with a head injury.
minutes as per the criteria of the American Psychiatric
Most people who sustain a head injury experience an
Association (DSM IV) but less than 30 minutes as per
altered state of consciousness for a brief period but may
the CDC and the American Congress of Rehabilitation
not define the experience as a concussion [5, Class II]. In
Medicine [3••, Class III]. Management of the concussed
the world of sport this is often referred to as a "ding" or
individual in the emergency department is discussed
"bell ringer." The practice guidelines of the AAN describe
briefly in the treatment section.
a grade 1 concussion as symptom duration for no more
On rare occasions, an individual can appear to have
than 15 minutes and no loss of consciousness. Athletes
experienced a grade 1 concussion when symptoms abate
will often deny theses symptoms in order to continue
after only a few minutes but then have a return of symp-
playing their sport, even though their performance is
toms some time later. As researchers learn more about the
often affected. If the injury occurs in a sports event it is
metabolic changes that characterize concussion, we real-
likely to be observed by others, and there is a better
ize this delayed presentation of symptoms is quite possi-
chance that medical services will be sought. However,
ble and explainable. In these instances, the categorization
research on adolescents in particular indicates that
of concussion should be upgraded to grade 2 or 3. One
approximately 75% of those with such injuries do not
should also be cognizant of any other signs or symptoms
seek attention from a physician unless symptoms persist
of the patient's condition worsening in order to be alert to
more that 24 hours [6, Class II]. The recommended
a possible intracranial hemorrhage. There are increasing
response of the physician during the initial visit of some-
recommendations in the sports concussion literature to
one with post-concussion is discussed later in this text.
define concussion severity in terms of the number, sever-
Recent research on grade 1 concussions indicates
ity, and duration of symptoms after concussion rather
that concussed individuals, even at this seemingly
than the immediate signs and symptoms such as loss of
minor level, may experience impaired memory and
consciousness [9•, Class III].
renewed symptoms within 36 hours of the injury [5,
Recent research on the metabolic changes that
Class II]. Renewed symptoms included headache, nau-
accompany concussion indicates that the brain should
sea, disturbed sleep, and balance problems. Current
return to normal in 7 to 10 days [10, Class II]. Concur-
recommendations for on-field assessment are that ath-
rent research on the cognitive changes that occur as a
letes with grade 1 concussions should not be allowed
result of concussion also shows a return to normal for
to return to play, even if they report being symptom
most individuals in 7 to 10 days [11]. Adolescents
free. There is significant risk of a second, more debili-
appear to take slightly longer to recover from concus-
tating injury. The extreme vulnerability of the slightly
sion than do adults [11]. All patients generally report
Management of Concussion and Post-Concussion Syndrome
Willer and Leddy
that their symptoms are gone (3–4 days post-concus-
female gender, age (> 40 years), and prior history of
sion) before they demonstrate physical and cognitive
affective disorder such as depression [16, Class II]. Pre-
homeostasis. During the period when the patient denies
dictors related to injury severity, such as length of post-
symptoms but metabolic changes are still in effect,
traumatic amnesia and cognitive difficulties (as demon-
symptoms may be induced by rigorous exercise. There-
strated on the digits forward and backward test), are
fore, team physicians use exercise as a "symptom stress
clearly associated with symptoms at 1 month but less so
test" to determine whether a player is ready to return to
at 6 months after injury [17, Class II].
play [12••, Class III].
The differential diagnosis of PCS includes factitious
Although most concussed individuals will recover
disorder, anxiety disorder, chronic fatigue syndrome,
completely within the 7- to 10-day period, approximately
and chronic pain syndrome. In many instances, espe-
10% will display signs and symptoms of concussion past
cially automobile crashes, one can see more than one
the usual period. After 3 weeks, patients begin to worry
condition in the same patient. Our advice is that if there
about when they will recover, and by 6 weeks, if symp-
is evidence for PCS, treat the PCS and then see if the
toms persist, PCS can alter how individuals live their lives.
depression or anxiety remains. We find that factitious
PCS is defined by the DSM IV as 1) cognitive deficits in
disorder is quite rare, and such patients do not generally
attention or memory, and 2) at least three or more of the
like to follow the recommended treatment plan for PCS
following symptoms: fatigue, sleep disturbance, head-
described in the following text.
ache, dizziness, irritability, affective disturbance, apathy,or personality change [13••, Class II]. The DSM IV diag-
PATHOPHYSIOLOGY OF CONCUSSION
nostic criteria are quite conservative. Most patients with
Concussion is the result of rapid deceleration of the
PCS have only a few symptoms, headache and fatigue
brain within the skull that imparts shearing or torsional
being the most common. The fatigue is related to changes
forces to neural tissue followed by metabolic and
in cognitive function and is most demonstrable for stu-
mechanical changes [3••, Class III]. The mechanical
dents (related to learning demands) and employees in
changes are generally referred to as diffuse axonal
whom work places demands for attention and concentra-
injury. The vulnerable cellular structure is the axon and
tion. A recent study found that use of the broader defini-
in particular the long axons, that is, axons involved with
high-level associative functions. In more severe brain
Organization [WHO] International Classification of Dis-
injury, diffuse axonal injury is visible on MRI because of
ease [ICD] 10 clinical criteria—three or more of the fol-
eventual cell death. With concussion the effects are less
lowing symptoms: headache, dizziness, fatigue,
obvious. Diffuse axonal injury is considered instrumen-
irritability, insomnia, concentration difficulty, or memory
tal in causing cognitive sequelae such as memory diffi-
difficulty) was six times more sensitive for identifying PCS
culties and problems with concentration.
patients [13••, Class II].
The forces that produce a concussion combined with
In the model of brain injury and concussion pre-
the stretching of axons result in what has been called a
sented in Figure 1, we suggest that patients with PCS have
cascade of neurochemical changes. In animal studies,
semipermanent brain injury and therefore move from a
this cascade occurs over a period of hours rather than
diagnosis of concussion to a diagnosis of mTBI. The
minutes and thus explains why some signs and symp-
assumption is that metabolic and structural changes in
toms of concussion may be delayed [10, Class II]. The
the brain of the concussed individual have not returned to
metabolic cascade is characterized by an initial depolar-
homeostasis. The diagnosis of PCS is controversial. The
ization of neuronal membranes and the release of excita-
symptoms of PCS, such as headache, fatigue, and depres-
tory amino acids, particularly glutamate, which produce
sive symptoms, are common in the general population.
fluxes of calcium and potassium ions across neural and
PCS is a common complaint of individuals involved in
vascular tissue resulting in at first a hypermetabolic glyco-
litigation after an injury. Individuals with PCS often
lytic state as the neurons attempt to restore equilibrium.
appear as confused about their symptoms as are the prac-
There follows a calcium ion–induced vasoconstriction
titioners treating them. Individuals with PCS are often
that reduces cerebral blood flow and glucose delivery
depressed, whether from neurologic insult related to the
with a resultant state of "metabolic depression" as the
concussion or in reaction to cognitive and somatic
brain energy demand is not met by the vascular energy
changes resulting from the concussion. Differential diag-
supply, which may last from days in animals to weeks in
nosis is not straightforward.
humans [10, Class II]. This complex cascade has also
Differential diagnosis is determined, in part, by care-
been shown to render neural tissue more susceptible to
ful history taking. Individuals with multiple concus-
further injury [7, Class II], which may explain the clinical
sions are more likely to sustain another concussion.
observation that patients with a history of concussions
Recent research suggests that a significant risk factor for
are at greater risk for recurrent concussion and for the
the development of PCS is three or more prior concus-
development of PCS. Recently, Korn et al. [18•, Class II]
sions [14,15, Class II]. Other predictors of PCS are
showed areas of focal cortical dysfunction in conjunction
Psychiatric Manifestations of Neurologic Disease
Table 1. Common acute symptoms of cerebral concussion
Feeling "slowed down"
Feeling "in a fog" or "dazed"
Difficulty concentrating
Difficulty remembering
Sensitivity to light/noise
Sleeping more than usual
Trouble falling asleep
Blurred vision/diplopia/flashing lightsTinnitus
Table 2. Common acute physical signs of cerebral concussion
Impaired conscious state or brief loss of consciousnessConfusionVacant stare/glassy eyedAmnesia: retrograde or anterogradeSlow to answer questions or follow directions; easily distracted/poor concentrationPoor coordination or balance; unsteady gaitPersonality change; inappropriate emotion (laughing or crying)Slurred speechIn athletes during competition, one may also observe:
Unaware of period, opposition, or game scoreInappropriate playing behavior, eg, running in the wrong directionSignificantly reduced playing ability
with blood-brain barrier disruption and reduced regional
altered brain metabolic milieu after concussion can per-
cerebral blood flow in patients months to years after
sist for a long time in some patients.
mTBI. Thus, the accumulating data suggest that the
Emergency department evaluation
• The history should include a description of the mechanism and force of the
head trauma and the number and severity of symptoms experienced by the patient. Table 1 presents common symptoms and Table 2 presents com-mon physical signs observed acutely after concussion. Symptoms may be delayed for several hours or days after even a seemingly mild head injury [5, Class II]. The physician should ask about the presence and duration of loss of consciousness, any convulsive activity, and any balance problems. Although dramatic and a signal to perform neuroimaging, post-concussive seizures are usually benign [19].
Physical examination and amnesia/cognitive tests
• The Sport Concussion Assessment Tool (SCAT) [12••, Class III] developed
by the 2004 Prague International Conference on Concussion in Sport is a standardized tool for patient education and physician evaluation of con-cussion. The SCAT includes a graded symptom checklist, cognitive assess-ment drills, and a brief physical examination. The patient is asked to recall five words immediately and then again after performing concentration
Management of Concussion and Post-Concussion Syndrome
Willer and Leddy
drills of stating the months of the year in reverse and a series of digits back-wards tests. The physical examination includes speech fluency, a cranial nerve examination, and pronator drift and gait assessment. The Romberg test and vestibular testing should also be performed because balance and vestibular deficits may persist for up to 10 days after concussion [20, Class II], with improvement correlating with recovery from concussion [21••, Class II]. Any focal neurologic deficits mandate rapid neuroimaging and neurosurgical consultation [3••, Class III].
Risk factors for hemorrhage and neuroimaging decision
• Risk factors for hemorrhage reported in the literature include GCS < 15,
amnesia, headache, vomiting, neurologic deficit, seizure, (older) age, race (black), mechanism of injury, drug/alcohol intoxication, and historical items (defined as pretrauma epilepsy, neurosurgeries, coagulation disor-ders, and shunted hydrocephalus) [22, Class I]. However, no single variable provides adequate positive prediction of the risk for intracranial lesions after mTBI. Two widely used clinical decision rules for the use of head CT in the emergency department are the Canadian Head CT Rule and the New Orleans Criteria. In a recent prospective comparison of these rules for pre-dicting the need for neurosurgical intervention after mTBI [23], both were found to be 100% sensitive, but the Canadian rule was significantly more specific. Nevertheless, physicians were not comfortable using the rules in all cases. The application of clinical decision rules was influenced by clinician thresholds, the prevailing local emergency department practices, and the legal climate.
• Wake-ups and rest
– It has been recommended that the concussed patient be awakened
every 3 to 4 hours during sleep to evaluate for signs of intracranial bleeding. No documented evidence suggests what severity of injury requires this approach, and there is debate as to whether this is neces-sary [24, Class III]. A good rule of thumb is if the patient has experi-enced loss of consciousness, prolonged amnesia, or is still experiencing significant symptoms, he or she should be awakened. The use of oral and written instructions increases the compliance rate for purposeful awakening during the night [25, Class III].
– Evidence from basic animal research suggests that an initial period of
physical and cognitive rest is therapeutic after concussive injury [10, Class II], but in a randomized human trial complete bed rest was ineffective in reducing symptoms [26, Class I]. The literature is in general agreement that relative rest (ie, avoiding studying and physi-cal exertion but resuming normal activities of daily living as soon as possible [24, Class III]) for the first 2 to 5 days after concussion is important because strenuous cognitive and physical activity may exacerbate symptoms and delay recovery [12••, Class III].
– Acetaminophen is a logical choice for immediate treatment of post-
concussion headache because there is a theoretical risk early after the injury (within 48–72 hours) of inducing or exacerbating cerebral hemorrhage with aspirin or other nonsteroidal anti-inflammatory drugs [24, Class III], although there are no controlled trials demon-strating this.
Psychiatric Manifestations of Neurologic Disease
– Many patients are discharged from the emergency department with
no specific recommendations for follow-up [2, Class II]. Two ran-domized trials have shown that routine follow-up after mTBI reduces the number and severity of post-concussion symptoms [27, Class II; 28, Class I]. Thus, it is important that these patients receive specific instructions to see their primary physician or a neurologist after emer-gency department discharge. Several European neurological societies have developed clinical guidelines that recommend routine follow-up for these patients [2, Class II].
– Although infrequent, the potential for neurologic deterioration after
mTBI exists [29, Class II]. Caregivers should be given specific written instructions regarding signs and symptoms to watch for. Written instructions are superior to verbal explanations, in terms of compli-ance with instructions and for retaining the information, but there are only limited scientific studies that identify what variables are the most important to monitor.
Initial physician visit
Classification of concussion severity
• The 2004 Prague International Conference on Concussion in Sport classi-
fies concussions as simple or complex [12••, Class III]. A simple concus-sion resolves within 7 to 10 days, with no residual deficits or complications, and does not require sophisticated imaging or testing. Simple concussions represent the most common form of this injury and can be managed by pri-mary care physicians. A complex concussion is characterized by persistent post-concussion symptoms, signs, cognitive dysfunction, and complica-tions (eg, convulsions). Patients with prolonged loss of consciousness (> 1 minute) or those who suffer multiple concussions over time or with pro-gressively less impact force may also be included in this category. Formal neuropsychological testing and neural imaging should be considered for complex concussions, and management generally requires a multidisci-plinary team (primary care/team physician, neurologist, neurosurgeon, and neuropsychologist).
History and examination
• The progression of initial symptoms and the appearance of any new symp-
toms must be assessed, and a thorough neurologic examination must be performed, emphasizing memory, concentration, cranial nerves, and bal-ance/vestibular function. The physician should elicit more detail about the number of prior concussions, the specific symptoms associated with each and time to resolution, any treatment, neuroimaging, and medication (pre-scription and nonprescription). Information about all prior head, face, or neck injuries is also relevant because patients often do not recognize that a concussion may have occurred on these occasions. Research on the signifi-cance of prior concussions indicates that subsequent concussions occur with decreasing levels of impact [12••, Class III].
• Because some patients may have persistent or worsening symptoms that
may be associated with intracranial lesions or subdural bleeding, clinicians must decide whether neuroimaging is indicated. In most patients who have a simple concussion, conventional neuroimaging is normal [12••, Class III]. CT or MRI is recommended if the patient is clinically worsening, but what constitutes deterioration is a clinical judgment. Newer imaging
Management of Concussion and Post-Concussion Syndrome
Willer and Leddy
modalities such as positron emission tomography, single photon emission computed tomography (SPECT), and functional MRI promise greater utility for concussion assessment but await prospective studies of their sensitivity, specificity, and predictive value.
• Activity
– Once the patient is asymptomatic at rest, he or she is advised to
progress stepwise from light aerobic activity such as walking or sta-tionary cycling up to sport or work-specific activities (see following text) [12••, Class III]. However, there is no evidence-based research to quantify specific activity type, intensity, and progression rate.
– The most common symptom for which medication is indicated is
post-concussion headache [30, Class III]. As many as one third of patients report increased headaches 1 year after head trauma [31]. Generally the headache (eg, tension, migraine) is similar to the type of headache the patient typically had before the trauma [30, Class III], with most (85%) being described as steady, aching, tension-type headaches [32, Class III]. Migraine headaches with or without aura have been reported with less frequency after concussion [32, Class III]. Adolescents participating in sports with repetitive minor head trauma such as football, hockey, and boxing can develop "footballer's migraine" [32, Class III]. The headaches are thought to be attributed to myofascial injuries, intervertebral disc damage, facet joint injury, temporomandibular joint injury, and muscle spasms in the superior trapezius and semispinalis capitis muscles in the suboccipital region [30, Class III].
– One study of depressed post-mTBI patients found that amitriptyline
was ineffective [33, Class II], whereas in another study amitriptyline reduced headache symptoms in patients without depression [34]. Intravenous dihydroergotamine has been shown to improve head-ache and to reduce sleep disturbance and dizziness in post-mTBI patients [35, Class II]. A randomized trial showed that cervical spinal manual therapy reduced headache pain at 5 weeks after head injury, versus the application of cold packs to the neck, but did not reduce the use of analgesics [36, Class II]. As discussed in a recent systematic review of treatments for mTBI, there is insufficient scientific evidence to support the use of specific pharmacologic interventions in the treatment of post-concussion headache [37••, Class III].
Return to activity
• Young athletes who return to competition before the symptoms of concus-
sion have resolved may be at risk for catastrophic cerebral edema and death, known as the second impact syndrome [38, Class III]. Although ear-lier guidelines from the AAN allowed patients with a grade I concussion (symptoms that resolve within 15 minutes; no loss of consciousness or amnesia) to return to play that contest, more recent guidelines recommend that all athletes who demonstrate signs or symptoms of concussion be withheld from participation and see a physician before returning to play [12••, Class III]. During the initial 2 to 5 days of recovery, patients must avoid symptom-inducing physical and cognitive activity. A stepwise approach for returning athletes to sport after concussion is now
Psychiatric Manifestations of Neurologic Disease
recommended [12••, Class III]. This stepwise approach allows athletes to proceed to increasing levels of activity if asymptomatic. If any symptoms occur, the patient returns to the previous asymptomatic level and tries to advance again after 24 hours. The advice to avoid at-risk situations that might produce symptoms (eg, strenuous exercise, flying, stress) should be provided to individuals injured in any circumstance.
Treatment of PCS
Diagnosis of PCS
• There is considerable controversy regarding PCS and whether these patients
are experiencing depression, somatization, chronic fatigue syndrome, chronic pain, vestibular dysfunction, or some combination of these condi-tions. Patients often present with considerable insecurity as to why they are experiencing PCS symptoms, which typically include headache, fatigue, sleep disturbance, vertigo, irritability, anxiety, depression, apathy, and diffi-culty with concentration. Symptoms are often subtle and difficult to link directly to the head trauma. However, recent research has demonstrated that most individuals complaining of PCS symptoms have neurologic changes as demonstrated by abnormal functional neuroimaging (SPECT) [39, Class II], neurochemical imbalances (eg, S100B) [40, Class II], and electrophysiological indices of impairment [41; 42, Class II].
• Diagnosis of PCS and description of relevant signs and symptoms are best
done using the WHO's ICD 10 criteria. The criteria require three or more of the symptoms described in the preceding paragraph. An interview format is available at no charge from the authors of an excellent review and investi-gation of the various criteria for diagnosis of PCS [13••, Class II]. We also recommend an assessment of postural stability using a procedure such as the Balance Error Scoring System [21••, Class II]. Postural instability is much more likely to be present when the other signs and symptoms are indeed the result of organic-based PCS. The overlap between symptoms of PCS and the competing diagnoses makes diagnosis difficult, but the best approach, in our opinion, is to assume that the individual has PCS unless there is 1) no response to treatment, or 2) compelling evidence to support an alternate diagnosis.
• Neurocognitive rehabilitation therapy is the most widely used treatment for
severely brain injured patients, but empirical investigations to date have not shown conclusive evidence of efficacy in improving outcome, and there are no published clinical trials of this treatment for mTBI or concussed patients. Nonetheless, research has demonstrated limited effectiveness of cognitive rehabilitation on cognitive functioning and activities of daily living using sin-gle-group design studies [43; 44, Class II]. A review indicates that neuropsy-chologists use the following intervention strategies with the greatest frequency: education of the patient regarding PCS, support and reassurance, graded increase in activity, and cognitive restructuring [45•, Class III]. Many neuropsychologists also recommended antidepressant medication.
• The most common medications prescribed by neurologists for PCS are
antidepressants [45•, Class III]. The selective serotonin reuptake inhibitors (SSRIs) have become the primary treatment for head injury–associated depression because of perceived clinical efficacy and relatively few side effects. However, most of the evidence for their use comes from small, uncontrolled/open studies and case reports rather than large randomized
Management of Concussion and Post-Concussion Syndrome
Willer and Leddy
trials. With this caveat in mind, these studies suggest that SSRIs are effica-cious in reducing depression and cognitive impairments. For example, in an 8-week, nonrandomized, single-blind trial of sertraline (starting at 25 mg/day and increasing stepwise up to 100–200 mg/day), Fann et al. [46, Class II] found that 87% of patients had significant reductions in depres-sion symptoms accompanied by improvements in cognitive variables of psychomotor speed and recent verbal and visual memory [46, Class II; 47, Class III]. Thus, treating depression after mTBI may also improve the cogni-tive deficits that afflict these patients.
• Over the past decade, a new group of antidepressants with a mixture of
effects on serotonin, norepinephrine, and dopamine has been developed. None of them has been scientifically evaluated for the treatment of PCS or post-concussion depression. Trazodone has been used in the brain-injured population to treat sleep disorders that can accompany head injury because it has been shown to be efficacious in depressed patients with insomnia [48, Class II]. However, it has anticholinergic and cardiovascular side effects, and priapism may limit its use.
• Cholinergic dysfunction is thought to underlie the memory impairment
seen in patients with Alzheimer's disease (AD). Because the deficits in attention and memory for new information seen after head injury mimic those in AD [49, Class III], memory deficits in TBI might be responsive to cholinergic treatment. Physostigmine and donepezil are acetylcholinest-erase inhibitors that temporarily increase brain acetylcholine levels, whereas lecithin and CDP-choline are precursors that increase brain acetyl-choline levels. In controlled trials, physostigmine improved neuropsycho-logical test performance when used alone [50, Class II] or in combination with lecithin [51, Class II] after TBI. However, its short half-life, non-oral route of administration, and problematic side effects limit its potential for human treatment. A 1-month placebo-controlled trial of CDP-choline [52, Class II] after mTBI showed improved neuropsychological test performance and reduced post-concussion symptoms, but the duration of improvement after medication termination was not reported.
• Donepezil, a longer-acting oral anticholinesterase inhibitor that is rela-
tively well tolerated, has been shown to improve cognition in AD patients [53, Class I], and two recent open-label controlled trials in patients with severe head injury [54,55, Class II] demonstrated improvements in func-tion [54] and in short- and long-term memory [54, Class II]. Donepezil also reduced measures of anxiety, depression, and apathy in some head-injured patients [54, Class II]. Thus, there is accumulating evidence that cholinergic agents may alleviate some of the cognitive deficits suffered by head-injured patients, but there is a need for large randomized trials of these agents in patients with concussion or mTBI.
Emerging therapy for PCS
• Most athletic team physicians have been using graded increased activity as a
standard procedure while monitoring the recovery of athletes with PCS. They discover that if the athlete returns to vigorous exercise too soon there is an immediate return of symptoms. In addition, because most athletes have learned to push themselves through pain, they often continue with the exercise until they become quite ill. Exercise-induced symptoms may last several days or even weeks, usually leaving the athlete quite discouraged (depressed).
• We have been monitoring athletes after concussion in a more systematic
manner. The athlete with PCS performs graded stationary cycle exercise under close observation, attempting to reach a heart rate target of 85% of
Psychiatric Manifestations of Neurologic Disease
age-predicted maximum. Blood pressure and perceived state of effort are measured every 2 minutes, and the athlete is instructed to stop the activity the moment he or she feels any symptoms of concussion. Typical symp-toms at the threshold are localized headache, feeling pressure in the head or the eyes, visual disturbance, and foggy thinking. The symptom-free exer-cise duration and intensity become the threshold for symptom regenera-tion, and we have the athlete return to the laboratory to exercise at 15% below threshold for 2 or 3 weeks. The opportunity to exercise is perceived as a very positive activity (often leading to an immediate reduction in depressive symptoms). It is imperative that the athlete not go beyond the new exercise limit, which most athletes are keen to do. After the 2 or 3 weeks of subthreshold exercise, the athlete is reassessed to see if the thresh-old has changed. The exercise program is then realigned to be 15% less than the new threshold. In our experience thus far, symptoms disappear within several months. Regular subthreshold exercise should help the indi-vidual become better conditioned and may have a fairly immediate effect on fatigue level and mood. We hypothesize that controlled, graded symp-tom-free exercise may restore to normal the cerebral autoregulatory system responsible for maintaining cerebral blood flow during changing states of systemic blood pressure, which may be dysfunctional in concussed patients [56, Class II].
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as:•
Of major importance
Kraus JF, Sorenson S: Epidemiology. In Neuropsychiatry
9.• Guskiewicz KM, Bruce SL, Cantu RC, et al.: Research
of Traumatic Brain Injury. Edited by Silver JM, Yudofsky
based recommendations on management of sport
SC, Hales RE. Washington, DC: American Psychiatric
related concussion: summary of the National Athletic
Press Inc.; 1994:3–41.
Trainers' Association position statement. Br J Sports
Bazarian JJ, McClung J, Cheng YT, et al.: Emergency
Med 2006, 40:6–10.
department management of mild traumatic brain
Important recent study.
injury in the USA. Emerg Med J 2005, 22:473–477.
Giza CC, Hovda DA: The neurometabolic cascade of
3.•• Bazarian JJ, Blyth B, Cimpello L: Bench to bedside: evi-
concussion. J Athl Train 2001, 36:228–235.
dence for brain injury after concussion--looking
Pellman EJ, Lovell MR, Viano DC, Casson IR: Concus-
beyond the computed tomography scan. Acad Emerg
sion in professional football: recovery of NFL and
Med 2006, 13:199–214.
high school athletes assessed by computerized neu-
Bazarian et al. provide an excellent summary of the recent
ropsychological testing--part 12. Neurosurgery 2006,
research on emergency care of those with mTBI and a precise
description of the pathophysiology of mTBI.
12.••McCrory P, Johnston K, Meeuwisse W, et al.: Summary
Kelly JP, Rosenberg JH: The development of guidelines
and agreement statement of the 2nd International
for the management of concussion in sports. J Head
Conference on Concussion in Sport, Prague 2004.
Trauma Rehabil 1998, 13:53–65.
Clin J Sport Med 2005, 15:48–55.
Lovell MR, Collins MW, Iverson GL, et al.: Grade 1 or
The authors provide an excellent description of the signs and
"ding" concussions in high school athletes. Am J Sports
symptoms of concussion and how to assess these on the field
Med 2004, 32:47–54.
and in the examining room.
Thurman DJ, Branche CM, Sniezek JE: The epidemiol-
13.••Boake C, McCauley SR, Levin HS, et al.: Diagnostic cri-
ogy of sports-related brain injuries in the United
teria for postconcussional syndrome after mild to
States: recent developments. J Head Trauma Rehabil
moderate traumatic brain injury. J Neuropsychiatry Clin
Neurosci 2005, 17:350–356.
Longhi L, Saatman KE, Fujimoto S, et al.: Temporal win-
This paper provides a current discussion and research on the
dow of vulnerability to repetitive experimental con-
varying criteria for defining and diagnosing PCS.
cussive brain injury. Neurosurgery 2005, 56:364–374.
Iverson GL, Gaetz M, Lovell MR, Collins MW: Cumula-
Lovell M, Iverson G, Collins M, et al.: Does loss of con-
tive effects of concussion in amateur athletes. Brain Inj
sciousness predict neuropsychological decrements
after concussion? Clin J Sport Med 1999, 9:193–198.
Management of Concussion and Post-Concussion Syndrome
Willer and Leddy
Iverson GL, Brooks BL, Lovell MR, Collins MW: No
Solomon S: Posttraumatic headache. Med Clin North
cumulative effects for one or two previous concus-
Am 2001, 85:987–996, vii–viii.
sions. Br J Sports Med 2006, 40:72–75.
Weight DG: Minor head trauma. Psychiatr Clin North
McCauley SR, Boake C, Levin HS, et al.: Postconcus-
Am 1998, 21:609–624.
sional disorder following mild to moderate traumatic
Hall RC, Hall RC, Chapman MJ: Definition, diagnosis,
brain injury: anxiety, depression, and social support
and forensic implications of postconcussional syn-
as risk factors and comorbidities. J Clin Exp Neuropsy-
drome. Psychosomatics 2005, 46:195–202.
chol 2001, 23:792–808.
Saran A: Antidepressants not effective in headache
Bazarian JJ, Atabaki S: Predicting postconcussion syn-
associated with minor closed head injury. Int J Psychia-
drome after minor traumatic brain injury. Acad Emerg
try Med 1988, 18:75–83.
Med 2001, 8:788–795.
Tyler GS, McNeely HE, Dick ML: Treatment of post-
18.• Korn A, Golan H, Melamed I, et al.: Focal cortical dys-
traumatic headache with amitriptyline. Headache
function and blood-brain barrier disruption in
patients with postconcussion syndrome. J Clin Neuro-
McBeath JG, Nanda A: Use of dihydroergotamine in
physiol 2005, 22:1–9.
patients with postconcussion syndrome. Headache
Important recent study.
McCrory PR, Berkovic SF: Video analysis of acute
Jensen OK, Nielsen FF, Vosmar L: An open study com-
motor and convulsive manifestations in sport-related
paring manual therapy with the use of cold packs in
concussion. Neurology 2000, 54:1488–1491.
the treatment of post-traumatic headache. Cephalalgia
Peterson CL, Ferrara MS, Mrazik M, et al.: Evaluation of
neuropsychological domain scores and postural sta-
37.••Comper P, Bisschop SM, Carnide N, Tricco A: A system-
bility following cerebral concussion in sports. Clin J
atic review of treatments for mild traumatic brain
Sport Med 2003, 13:230–237.
injury. Brain Inj 2005, 19:863–880.
21.•• Guskiewicz KM: Assessment of postural stability fol-
This review of the literature on treatment of mTBI is useful for
lowing sport-related concussion. Curr Sports Med Rep
various reasons but most specifically for the concise review of
This study describes a test of postural ability after concussion
Cobb S, Battin B: Second-impact syndrome. J Sch Nurs
and highlights the important role of this type of assessment in
the neurologic examination.
Agrawal D, Gowda NK, Bal CS, et al.: Is medial tempo-
Dunning J, Stratford-Smith P, Lecky F, et al.: A meta-
ral injury responsible for pediatric postconcussion
analysis of clinical correlates that predict significant
syndrome? A prospective controlled study with single-
intracranial injury in adults with minor head trauma.
photon emission computerized tomography. J Neuro-
J Neurotrauma 2004, 21:877–885.
surg 2005, 102(Suppl 2):167–171.
Stiell IG, Clement CM, Rowe BH, et al.: Comparison of
Stalnacke BM, Bjornstig U, Karlsson K, Sojka P: One-
the Canadian CT Head Rule and the New Orleans Cri-
year follow-up of mild traumatic brain injury: post-
teria in patients with minor head injury. JAMA 2005,
concussion symptoms, disabilities and life satisfac-
tion in relation to serum levels of S-100B and neu-
Guskiewicz KM, Bruce SL, Cantu RC, et al.: Recommen-
rone-specific enolase in acute phase. J Rehabil Med
dations on management of sport-related concussion:
summary of the National Athletic Trainers' Associa-
Gaetz M, Weinberg H: Electrophysiological indices of
tion position statement. Neurosurgery 2004, 55:891–
persistent post-concussion symptoms. Brain Inj 2000,
895; discussion 896.
de Louw A, Twijnstra A, Leffers P: Lack of uniformity
Arciniegas DB, Topkoff JL: Applications of the P50
and low compliance concerning wake-up advice fol-
evoked response to the evaluation of cognitive
lowing head trauma. Ned Tijdschr Geneeskd 1994,
impairments after traumatic brain injury. Phys Med
Rehabil Clin N Am 2004, 15:177–203, viii.
de Kruijk JR, Leffers P, Meerhoff S, et al.: Effectiveness of
Ho MR, Bennett TL: Efficacy of neuropsychological
bed rest after mild traumatic brain injury: a ran-
rehabilitation for mild-moderate traumatic brain
domised trial of no versus six days of bed rest. J Neurol
injury. Arch Clin Neuropsychol 1997, 12:1–11.
Neurosurg Psychiatry 2002, 73:167–172.
Cicerone KD: Remediation of "working attention" in
Ponsford J, Willmott C, Rothwell A, et al.: Impact of
mild traumatic brain injury. Brain Inj 2002, 16:185–195.
early intervention on outcome following mild head
45.• Mittenberg W, Canyock EM, Condit D, Patton C: Treat-
injury in adults. J Neurol Neurosurg Psychiatry 2002,
ment of post-concussion syndrome following mild
head injury. J Clin Exp Neuropsychol 2001, 23:829–836.
Wade DT, King NS, Wenden FJ, et al.: Routine follow up
Important study.
after head injury: a second randomised controlled
Fann JR, Uomoto JM, Katon WJ: Sertraline in the treat-
trial. J Neurol Neurosurg Psychiatry 1998, 65:177–183.
ment of major depression following mild traumatic
Lee ST, Liu TN, Wong CW, et al.: Relative risk of deteri-
brain injury. J Neuropsychiatry Clin Neurosci 2000,
oration after mild closed head injury. Acta Neurochir
(Wien) 1995, 135:136–140.
Psychiatric Manifestations of Neurologic Disease
Zasler ND: Mild traumatic brain injury: medical
Levin HS: Treatment of postconcussional symptoms with
assessment and intervention. J Head Trauma Rehabil
CDP-choline. J Neurol Sci 1991, 103(Suppl):S39–S42.
Rogers SL, Doody RS, Mohs RC, Friedhoff LT: Donepezil
Zafonte RD, Cullen N, Lexell J: Serotonin agents in the
improves cognition and global function in Alzheimer
treatment of acquired brain injury. J Head Trauma
disease: a 15-week, double-blind, placebo-controlled
Rehabil 2002, 17:322–334.
study. Donepezil Study Group. Arch Intern Med 1998,
Griffin SL, van Reekum R, Masanic C: A review of cho-
linergic agents in the treatment of neurobehavioral
Masanic CA, Bayley MT, VanReekum R, Simard M:
deficits following traumatic brain injury. J Neuropsychi-
Open-label study of donepezil in traumatic brain
atry Clin Neurosci 2003, 15:17–26.
injury. Arch Phys Med Rehabil 2001, 82:896–901.
Cardenas DD, McLean A Jr, Farrell-Roberts L, et al.: Oral
Whelan FJ, Walker MS, Schultz SK: Donepezil in the
physostigmine and impaired memory in adults with
treatment of cognitive dysfunction associated with
brain injury. Brain Inj 1994, 8:579–587.
traumatic brain injury. Ann Clin Psychiatry 2000,
Levin HS, Peters BH, Kalisky Z, et al.: Effects of oral
physostigmine and lecithin on memory and attention
Henninger N, Dutzmann S, Sicard KM, et al.: Impaired
in closed head-injured patients. Cent Nerv Syst Trauma
spatial learning in a novel rat model of mild cerebral
concussion injury. Exp Neurol 2005, 195:447–457.
Source: http://concussion.ubmd.com/wp-content/uploads/2014/04/management-of-concussion-and-post-concussion-syndrome.pdf
Microsoft word - blanqueamiento.doc
Blanqueamiento de dientes con decoloraciones severas Dr. Salvador Alonso Pérez Prof. Colaborador de Materiales Odontológicos. Facultad de Odontología Universidad de Barcelona. Doctor en Medicina. Médico Especialista en Estomatología y en Cirugía Dra. Soledad Espías Gómez Prof. Colaborador de Materiales Odontológicos. Facultad de Odontología Universidad de
Ifm visiÓn, filosofÍa, principios
Ideas, perspectivas y principios que nos deben acompañar, caracterizar y unir. © Copyright 2012, ifm electronic gmbh, Friedrichstraße 1, 45128 Essen Queda prohibida la reproducción, total o parcial, distribución, comunicación pública y transformación de esta obra sin la autorización escrita de ifm electronic gmbh este libro está impreso en papel blanco libre de cloro