1477-7819-1-6.fm
World Journal of Surgical OncologyTechnical Innovations
Holmium Laser Enucleation of the Prostate (HoLEP):
A Technical Update
Ramsay L Kuo*1, Ryan F Paterson1, Samuel C Kim1, Tibério M Siqueira Jr1,
Mostafa M Elhilali2 and James E Lingeman1
Address: 1Methodist Hospital Institute for Kidney Stone Disease and Indiana University School of Medicine Indianapolis, Indiana, USA and 2The Department of Urology McGill University Faculty of Medicine Montreal, Quebec, Canada Email: Ramsay L Kuo* - [email protected]; Ryan F Paterson - [email protected]; Samuel C Kim - [email protected]; Tibério M Siqueira Jr - [email protected]; Mostafa M Elhilali - [email protected]; James E Lingeman - [email protected] * Corresponding author Published: 6 June 2003 Received: 6 February 2003Accepted: 6 June 2003 World Journal of Surgical Oncology 2003, 1:6
2003 Kuo et al; licensee BioMed Central Ltd. This is an Open Access article: verbatim copying and redistribution of this article are permitted in all media for any purpose, provided this notice is preserved along with the article's original URL.
Benign prostatic hyperplasiaHolmiumLasers Introduction: Holmium laser enucleation of the prostate (HoLEP) combined with mechanical
morcellation represents the latest refinement of holmium:YAG surgical treatment for benign
prostatic hyperplasia (BPH). Utilizing this technique, even the largest of glands can be effectively
treated with minimal morbidity. The learning curve remains an obstacle, preventing more
widespread adoption of this procedure. This paper provides an outline of the HoLEP technique as
is currently used at two centers in hopes of easing the initial learning curve.
Technical considerations: Detailed descriptions of the major steps of the HoLEP procedure are
provided with attention to critical steps such as identification of the surgical capsule, median and
lateral lobe enucleation, and morcellation of enucleated tissue.
Conclusions: HoLEP is a promising alternative for the surgical treatment of BPH which allows
complete removal of intact lobes of the prostate. Obstruction is relieved immediately with superior
hemostasis, no risk of TUR syndrome, and a minimal hospital stay.
to avoid or treat long-term sequelae such as urinary reten- Benign prostatic hyperplasia (BPH), which is prevalent in tion, urinary tract infections, and bladder calculi.
up to 43% of men over the age of], continues to be aleading cause of voiding difficulties. Symptoms generally When surgical treatment is considered, transurethral worsen with age, with men experiencing a mean increase resection of the prostate (TURP) is still the standard to of the American Urological Association (AUA) symptom which all other modalities are compared. Although the score of 0.18 points per year of follow-uphough morbidity associated with TURP can be low when per- symptoms can often be handled adequately with medical formed by experienced surgeons, complications such as therapy, patients who continue to suffer significant void- TUR syndrome and bleeding can still occur. For this rea- ing problems will eventually require surgical intervention son, many alternative energy modalities have been devel-oped in an attempt to not only provide an effective (page number not for citation purposes) World Journal of Surgical Oncology 2003, 1
surgical treatment for BPH, but also to minimize the risk by vaporization of an adequately sized channel using hol- of complications and the length of hospital stays.
mium energy. Unfortunately, this combination procedurewas still associated with significant indwelling catheteri- One such technological advance involves the hol- zation times postoperatively, ranging from 4.1 to 7.1 mium:YAG laser. This laser has found widespread uro- addition, many patients required re-catheter- logic applications, especially in the treatment of ization for urinary retention and also had irritative void- urolithiasisse the laser's wavelength is highly absorbed by], it is also an effective tool for theablation and cutting of soft tissue. These characteristics As more clinical experience with the holmium laser was naturally extend into applications for BPH.
gained, it became apparent that the laser had sufficienthemostatic effects when used to vaporize soft tissue on its Use of the holmium:YAG laser in the treatment of BPH own, without the addition of the Nd:YAG compon has changed significantly over the past five years. As tech- Further evidence of the effectiveness of the holmium laser niques have been refined and equipment improved, the on prostate tissue was provided by canine and human spectrum of treatment has progressed from simple vapor- studies by Kabalin, who showed that hemostatic vaporiza- ization of tissue to the complete removal, or enucleation, tion occurred using high powers ranging from 50 to 80 of intact lobes of prostatic adenoma. At the present time, As a result, holmium laser ablation of the holmium laser enucleation of the prostate (HoLEP) com- prostate, termed HoLAP, was developed, which elimi- bined with mechanical morcellation represents the latest nated many of the short-term voiding problems associ- refinement of the resection technique. By utilizing this ated with use of the Nd:YAG laser.
procedure, even extremely large glands which previouslywould have required an open simple prostatectomy can The main advantage of HoLAP was the ease in learning the be treated effectively, with only an overnight stay for the procedure. One disadvantage, however, was the lack of tis- patient. In our experience, the largest gland we have sue availability for pathologic analysis. In addition, the treated successfully with HoLEP had a specimen weight of procedure was considered cumbersome, mainly because 376 grams after morcellation (unpublished data).
of the slow process of tissue vaporization. In a rand-omized comparison of holmium vaporization versus Although HoLEP is a promising alternative for the surgical TURP, Mottet, et al, showed that the laser procedure treatment of BPH, the learning curve for the procedure required a significantly longer time (75 vs. 56 minutes) to remains a significant obstacle. The purpose of this paper achieve prostatic defects comparable to those in the TURP is to review the development of HoLEP and present a step- patientFor this reason, HoLAP was considered use- wise outline of the procedure, with a complete list of nec- ful only for smaller glands. In order to achieve more effi- essary equipment and attention to critical points during ciency, attention then turned to developing a method of the enucleation process. It is hoped that this description removing larger portions of adenoma.
of HoLEP will help to flatten the learning curve for urolo-gists interested in learning this procedure.
The first description of holmium laser resection of theprostate (HoLRP) was reported by Gilling, et al in 1996s technique was the first to utilize the cutting Historical development of HoLEP
properties of the holmium laser to detach large sections of The holmium:YAG laser (2140 nm) acts through a pre- adenoma tissue. A major advantage is that normal saline dominantly photothermal mechanism.[ecause it is could be used as the irrigation fluid, which eliminates the capable of vaporizing soft tissue, application of the hol- risk of TUR syndrome during resection. During a HoLRP, mium laser for BPH first focused on sequential ablation of the median lobe is resected first, followed by the lateral tissue in order to enlarge a channel through the prostate.
lobes. Because tissue needs to be retrieved endoscopically, Initially, treatment with the holmium laser was per- the lobes are divided into manageable pieces while being formed in association with the neodymium (Nd:YAG) freed from the surgical capsule. Larger fragments are then laser, in a technique known as combination endoscopic recovered from within the bladder using a modified resec- laser ablation of the prostate (CEL It was hoped toscope loop that engages and holds the tissue against the that the holmium laser would be able to reduce the short- resectoscope sheath, while smaller fragments can be term sequelae of Nd:YAG coagulation prostatectomy, removed using an Ellik evacuator.
which included prolonged catheterization and delayedsymptomatic improv Many centers have published HoLRP series with favorableresultsIn all of these series, no patients required With CELAP, a circumferential coagulation of prostatic tis- transfusions or developed dilutional hyponatremia. In a sue was first performed using the Nd:YAG laser, followed randomized trial comparing HoLRP to TURP with two (page number not for citation purposes) World Journal of Surgical Oncology 2003, 1
year follow-up data, there were no significant differences followed by appropriate prostate biopsies before proceed- in AUA symptom scores, quality of life scores, peak flow ing with HoLEP. A coagulation profile is not routinely rates, or complications; however, TURP patients had sig- obtained at our institutions unless a history of bleeding nificantly longer mean catheterization times and hospital diathesis is present.
Because size estimates from digital rectal exams can be Operative time remains an issue for HoLRP, with TURP inaccurate, obtaining a transrectal ultrasound (TRUS) being completed at significantly fastere issue prostate volume pre-operatively is recommended. This is contributing to the overall length of the procedure is the an important data point, as one should aim to start with retrieval of the resected tissue. First of all, the size of the smaller glands (i.e. < 40 cc) when first learning the proce- tissue fragments is limited by the urethral caliber. In addi- dure. Further, TRUS provides a clearer estimation of the tion, the resectoscope must be removed in its entirety each time required for the procedure when arranging operative time a fragment is removed, thus slowing the process.
schedules. In addition, flexible cystoscopy is performed Questions have also been raised about the ability to on all patients as part of their workup in order to exclude obtain accurate pathologic diagnoses with HoLRP, citing other forms of obstruction such as urethral strictures.
an abundance of cauterization artifact from analyzedspecimen Lastly, informed consent must be obtained from thepatient. Particular emphasis must be placed on the possi- In order to address the previous concerns with HoLRP, a bility of retrograde ejaculation after the procedure, which prototype transurethral tissue morcellator was devised by had previously been documented to occur in up to 96% of Fraundorfeating tissue HoLRP patientin our experience, occurs in most within the bladder, the resection technique could be mod- HoLEP patients.
ified to allow complete enucleation of the median and lat-eral lobes of the bladder, without the time-consuming process of tailoring the lobes into manageable fragments.
The only absolute contraindications to the HoLEP proce- This enables the surgeon to achieve a degree of tissue dure are a lack of surgical clearance from a cardiopulmo- removal approximating that of an open simple prostatec- nary standpoint or an inability to position the patient in tomy while maintaining a minimally invasive nature. As the dorsolithotomy position. In general, bleeding diathe- such, the latest modification of the holmium resection ses are not a contraindication to HoLEP; however, we do technique is now known as holmium laser enucleation of not recommend treating patients with uncorrected bleed- the prostate (HoLEP), combined with mechanical morcel- ing diatheses during the initial learning curve. In general, lation. HoLEP can be utilized for virtually any BPH con- if patients are on anti-coagulants (i.e. warfarin) for entities figuration or size. Further, concomitant bladder calculi, if where the medication can be safely stopped (deep venous present, are easily vaporized by the holmium laser at the thrombosis or atrial fibrillation), they should be taken off time of HoLEP. Using this technique, even the largest of their medication 3–5 days prior to surgery. The medica- glands can be safely enucleated, with superior results tion can be restarted post-operatively at the normal dose.
when compared to the alternative approach of open sim- When anticoagulation cannot be held (i.e. cardiac valves), ple prostateary of the published HoLEP can be performed on fully anticoagulated patients.
HoLEP results are detailed in ta A list of important equipment required for HoLEP isdetailed Currently, we use HoLEP exclusively in our respectiveinstitutions for the surgical treatment of BPH. The follow- ing is a description of our HoLEP technique, detailing the Step 1 – Urethral calibration pre-operative work-up, necessary equipment, and step- The patient is placed in a dorsolithotomy position, with wise breakdown of the procedure.
the thighs abducted maximally to allow appropriatemanipulation of the resectoscope during apical dissection of the lateral lobes. After sterile preparation and draping is completed, the patient's urethra is calibrated using Van As with any surgical procedure, the HoLEP pre-operative Buren sounds up to 30 F. Only the anterior urethra should work-up consists of a detailed history and physical, which be calibrated and care should be taken to avoid traumatiz- should include an AUA symptom score and also a flow ing the prostatic lobes, which can lead to bleeding and an rate and post-void residual to objectively document the impaired visual field. The urethra must be able to accept severity of obstruction. Laboratory tests consist of a com- calibration up to 30 F easily; if not, urethrotomy should plete blood count, serum chemistries, PSA level, and uri- be considered to widen the distal urethra. This minimizes nalysis with urine culture. Any PSA elevation should be (page number not for citation purposes) World Journal of Surgical Oncology 2003, 1
Table 1: Summary of HoLEP Results
Fraundorfer, et al] * Includes enucleation and morcellation time # Patients with > 100 gram prostates the possibility of urethral stricture from subsequent resec- ating a lateral lobe initially (Step 4B). The laser should be set at an energy of 2 J and frequency of 50 Hz.
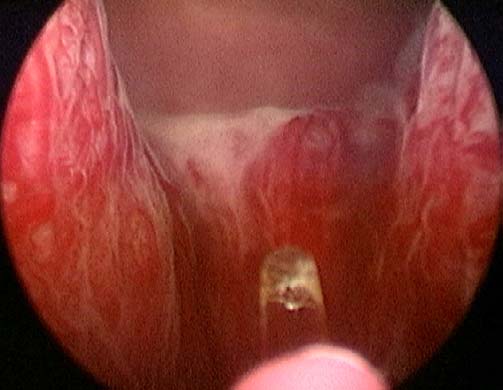
Step 2 – Insertion of the resectoscope Step 4A – Enucleation of the median lobe A 26–28 F continuous flow resectoscope is inserted into In the case of trilobar hypertrophy, the surgeon will be the urethra with the Timberlake obturator. The inner able to visualize two sulci at approximately the 5 and 7 sheath, with 7 F laser fiber stabilizing catheter in place, is o'clock positions, formed by the junctions of the lateral then locked into the resectoscope. Because of the high and median lobes (Fginning at the level of the power (up to 100 W) utilized for HoLEP, a video system bladder neck at the 7 o'clock position, a groove is formed is mandatory for the surgeon's optical protection. The by cutting with the laser along the sulcus, to a point just camera is placed on the lens, and the handpiece loosened lateral and proximal to the verumontanum. This groove is such that the resectoscope can be rotated easily while deepened to the level of the surgical capsule. As the groove holding the camera in a stationary position.
is developed, it should also be undermined and widenedto allow separation of the right lateral lobe and median Lastly, the 550 µ laser fiber is placed. Approximately 3 to lobe. The process is then repeated to create a groove at the 4 inches of cladding from the distal portion of the fiber 5 o'clock position.
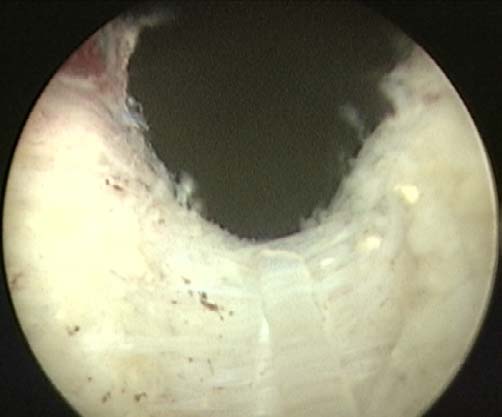
should be stripped off. It is helpful to thread the redun-dant portion of the fiber through mosquito clamps During the initial learning curve, it is often difficult to dis- attached to the drape, thus keeping it out of the surgeon's cern the level of the plane between the adenoma and sur- working space. The fiber can then be inserted into the 7 F gical capsule when deepening the groove. To facilitate the stabilizing catheter. Normal saline irrigant is then run development of the correct plane, one should first attempt through TUR tubing into the resectoscope. The outflow to deepen the groove proximally, as the surgical capsule in valve should be connected to a piece of tubing to allow this region is more easily defined by its characteristic drainage into the cystoscopy drape trap and left open, to white circular fibers (Figs the incision progresses prevent overdistension of the bladder.
along the sulcus to the mid-portion of the prostatic fossa,the level of the capsule can be more difficult to define. The Step 3 – Visualization of the anatomy groove should end just laterally to the verumontanum. If With the resectoscope in the bladder, the urethral orifices the surgeon is unsure about the depth of the more distal should be located if possible, though an extremely large portion of the groove, an initial undermining of the floor median lobe may preclude this. The resectoscope is then of the lateral lobe just lateral to the verumontanum can pulled back into the prostatic fossa and the extent of lobar help to define the proper plane. To begin this dissection, hypertrophy assessed. Lastly, the location of the verumon- one should guide the laser fiber in a transverse fashion lat- tanum and external sphincter is confirmed. The initial erally from the verumontanum. The beak of the resectos- step of resection depends on the degree of median lobe cope can then be angled under the lateral lobe as the plane hypertrophy. If the median lobe is enlarged, it is best to between the adenoma and the surgical capsule develops.
enucleate this structure first, in order to provide more The appearance of the capsule here is a smooth, glistening room for the lateral lobe dissection (Step 4A). If the surface with occasional diaphanous, cobweb-like attach- median lobe is not greatly enlarged, one can begin enucle- ments to the adenomatous tissue. At times, the capsulemay be thinned to the point where fat is visible. The (page number not for citation purposes)
World Journal of Surgical Oncology 2003, 1
Table 2: Essential equipment list
Video tower and cameraHolmium laser unit (must have 80–100 watt maximum power)550 µ holmium laser fiber550 µ laser fiber stripper26 to 28 F continuous flow resectoscope sheath with modified inner sheath (containing laser fiber stabilizing bridge)30 degree cystoscope lens7 F laser fiber stabilizing catheter (Cook Urological, Incorporated, Spencer, Indiana)Van Buren soundsEllik evacuatorStone basket, model FG-24SX-1 (Olympus)11 F Alligator grasper (Karl Storz)Offset rigid nephroscope (Karl Storz)Morcellator (Lumenis)Normal saline irrigant (3 liter bags)20 F, 2-way Foley catheter (30 cc balloon)Catheter guide
Figure 1
Sulci between median and lateral lobes (at 5 and 7 o'clock)
appearance of fat should alert the surgeon to continuedeveloping a plane just superficial to this level. However,these areas seal post-operatively without sequela and are
ing the lateral lobe from the capsular floor by moving the
not an indication to abort or shorten the procedure, as in
laser fiber in a transverse, side-to-side motion while using
the case of TURP.
the beak of the resectoscope to leverage the lobe upwards.
It is important to avoid rotating the resectoscope too early,
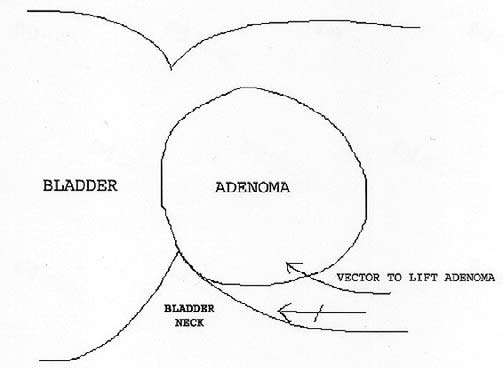
At this point, undermining of the median lobe is begun
as this will cause the fiber tip to arc into the adenoma pre-
just proximal to the verumontanum. The laser fiber is
maturely and potentially cause loss of plane definition.
swept in a transverse fashion between the two grooves,staying in the plane between the surgical capsule and the
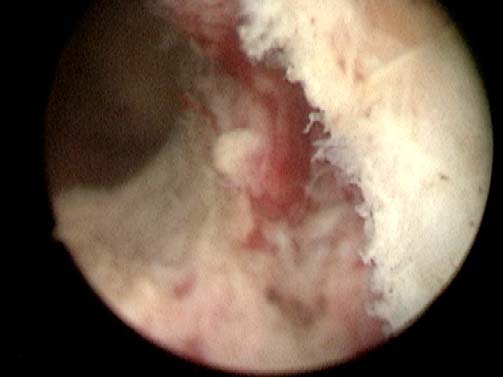
Step 5 – Right apical and lateral dissection (from floor)
adenoma. As the distal portion of the median lobe begins
The plane between the capsular floor and right lobe
to separate away from the capsule, the beak of the resecto-
should be developed proximally toward the bladder. At
scope should be used as a leverage point to assist in lifting
some point, the surgeon will notice that leverage under
the median lobe upward. This helps define the plane
the lateral lobe is impaired by the lateral attachments of
between the adenoma and the capsule. Again, the capsule
the lobe, making further proximal progression difficult.
tends to be smooth and shining, with cobweb-like attach-
Dissection should then proceed to detach the lateral
ments to the adenoma. The surgeon should take care to
attachments near the apex of the right lateral lobe.
follow the capsule as it slopes gently anteriorly toward theregion of the bladder neck, to prevent undermining of the
The laser settings are adjusted to a power of 2 J and fre-
trigone. Once the level of the bladder neck is reached, the
quency of 40 Hz during the process of apical dissection, to
proximal attachments of the median lobe are freed, and
prevent thermal injury to the sphincter. The resectoscope
the entire median lobe is pushed into the bladder.
is retracted distally, and the location of the external ure-thral sphincter confirmed by visualizing the area where
Step 4B – Separation of the right lobe from the capsular floor
urethral coaptation occurs. After moving the resectoscope
If the median lobe does not have significant hypertrophy,
proximally to the sphincter, the most lateral point of the
a midline groove can be created at the 6 o'clock position
previously dissected plane between the floor and right
beginning at the bladder neck and ending just proximal to
lobe is located. Dissection in this plane is continued, this
the verumontanum. Again, the groove should be defined
time staying between the apical tissue of the right lobe
initially with the tip of the laser fiber and then widened
and the capsule by rotating the resectoscope in a clockwise
and deepened down to the level of the surgical capsule.
direction during cutting. There is limited space for the tip
Dissection of the right lobe can then be performed by pro-
of the resectoscope during this portion of the dissection,
ceeding lateral to the verumontanum in a transverse fash-
restricting the field of view. Therefore, the tip of the laser
ion. Once the initial plane is developed under the right
fiber should be retracted to the point where it is barely vis-
lobe, the surgeon continues in a proximal direction, free-
ible. The arcing motion of the fiber tip should follow the
(page number not for citation purposes)
World Journal of Surgical Oncology 2003, 1
Figure 3
Appearance of left apical pad
Figure 2
Appearance of proximal surgical capsule
groove should span from the level of the bladder neck tothe level of the verumontanum. The surgeon should occa-
curve of the surgical capsule as it progresses laterally. It is
sionally reconfirm the location of the verumontanum by
important to begin the dissection at a point slightly
looking toward the floor, to ensure that the groove is not
proximal to the apex, in order to leave behind an "apical
extended too far distally. Once the groove is created, it is
pad" of tissue that helps protect the integrity of the
again widened and deepened to the level of the surgical
capsule along its entire extent.
Once definition of the apical tissue has begun, the beak of
Step 7 – Separation of right lobe from roof of capsule
the resectoscope is again guided under the lip of the apex
The tip of the laser fiber should be angled toward the
to leverage the adenoma away during dissection. The lat-
plane between the adenoma and the capsule. Initially, the
eral dissection should proceed up to approximately the 9
fiber should be directed along the plane proximally and
to 10 o'clock position, with smaller glands allowing more
distally in a sequential fashion to begin dividing the ante-
lateral freedom. The lateral wall of the right lobe should
rior attachments of the right lobe. It is helpful for the dis-
then be freed from the surgical capsule by proceeding
section to begin at the bladder neck, where capsular
proximally along the already defined plane. At this point,
definition is much easier (FigurThe attachments
the surgeon should be rotating the resectoscope in alter-
between the anterior portion of the lobe and the capsule
nating clockwise and counterclockwise directions, which
are taken down sequentially until the lateral extent of the
causes the tip of the laser fiber to proceed in a smooth arc
lobe is reached.
back and forth within the established plane. The dissec-tion should be continued until difficulty is encountered
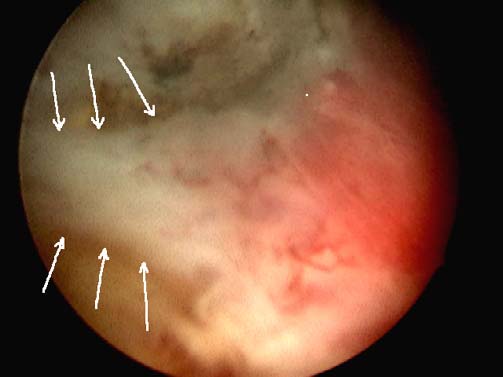
Step 8 – Dissection and release of lateral portion of right lobe
with exposure of the plane proximally. As much of the
It is crucial at this stage to identify the extent of the
lateral lobe is dissected away from the bladder neck area
remaining lateral attachments near the apex of the lobe.
as possible, to facilitate the final steps of the enucleation.
This process can be difficult, as the planes of dissectionbetween the adenoma and capsule from the anterior and
Step 6 – Creation of anterior groove
posterior vectors may not join at the same level laterally.
Attention is turned to the 12 o'clock region of the prostatic
It is helpful to gain perspective by guiding the resectos-
fossa, where the anterior commisure (midline groove
cope first along the anterior plane and then the posterior
between lateral lobes) is located. The resectoscope is
plane, to fully visualize the lateral extent of each. Once the
turned 180° to allow the laser fiber to be positioned cor-
junction between the planes is defined, usually by a
rectly. Laser settings should be adjusted back to 2 J and 50
mucosal strip or bridge (Figurey the laser to
Hz. Beginning at the bladder neck and proceeding dis-
join the planes. Laser settings are 2 J and 40 Hz during
tally, a groove is cut along the anterior commisure. This
division of the mucosal strip. The surgeon can then con-
(page number not for citation purposes)

World Journal of Surgical Oncology 2003, 1
Figure 5
Appearance of mucosal strip (to left)
Figure 4
Dissection of plane between anterior surgical capsule and
adenoma
erally, and division of the remaining attachments at thebladder neck are done as previously described.
tinue the dissection proximally, at 2 J and 50 Hz, to free
Step 11 – Inspection of the prostatic fossa
the lateral extent of the lobe.
Once all lobes have been dissected free and pushed intothe bladder, the laser settings should be changed to 2.5 J
Step 9 – Completion of right lobe enucleation
and 40 Hz (for large bleeders) or 1.5 J and 30 Hz (for
At this point, the right lobe will be held only by attach-
smaller bleeders and near apex) to achieve optimal coag-
ments at the bladder neck level. The anterior attachments
ulation. The capsular surface is then inspected carefully.
at the bladder neck should already have been divided. By
Any capsular bleeders should be coagulated by first defo-
following this plane further laterally, any remaining
cusing the laser (positioning tip of the fiber 2–3 mm away
attachments in this area can be freed. Finally, one should
from the surface) and then activating it until hemostasis is
proceed under the lobe and finish dividing attachments at
achieved. A dry fossa is essential before beginning
the floor of the capsule and the posterior bladder neck.
morcellation to optimize visualization and minimize the
The lobe can then be pushed into the bladder by leverag-
risk of bladder injury. If any residual portions of adenoma
ing upward with the beak of the resectoscope
remain along the surface of the capsule, these can be easily
Care should be taken to avoid injuring the bladder neck
vaporized or enucleated with the laser.
during this process, which can occur if the resectoscopebeak is inadvertently pushed too posteriorly.
Step 12 – MorcellationThe inner sheath of the resectoscope along with the laser
Step 10 – Enucleation of the left lobe
fiber and stabilizing catheter are removed. The rigid offset
The left lateral side of the 5 o'clock groove (or 6 o'clock
nephroscope is then inserted into the outer resectoscope
groove in cases where the median lobe did not require
sheath. We utilize a commercially available morcellator
enucleation) is undermined, beginning at the bladder
(VersaCut, Lumenis Incorporated, Santa Clara, CA) con-
neck level and progressing distally. This begins separation
sisting of a set of hollow reciprocating blades (5 mm
of the posterior portion of the lateral lobe from the capsu-
diameter shaft) attached to a handle apparatus .
lar floor. The plane between the left lobe and the floor of
Offset nephroscopes with a 5 mm working channel (Karl
the surgical capsule is further defined by cutting laterally
Storz, Olympus) are required to accommodate the mor-
from the verumontanum in a transverse fashion. The beak
cellator. Olympus is the only manufacturer with a pur-
of the resectoscope can then be used to provide leverage
pose-built device for HoLEP and morcellation. A vacuum
under the lateral lobe while division of the posterior
pump is connected to the morcellator handle to provide
attachments is continued. Dissection of the left lobe apex,
suction through the blades, and device activation control-
anterior portion of the lobe, connection of the planes lat-
led through a foot pedal. Inflow tubing with normal
(page number not for citation purposes)

World Journal of Surgical Oncology 2003, 1
prostatic fossa. It can then be incised at different pointswith the laser fiber, providing more surface area for mor-cellator engagement without the risk of bladder injury.
As a option to morcellation, other investigators havedescribed a modified tissue retrieval technique where anenucleated prostate lobe is initially left attached at thebladder neck by a small pediA TUR electrocauteryloop is subsequently utilized to resect the lobe into piecesretrievable with an evacuator. While this alternative obvi-ates the need for a mechanical morcellator, the medianprostate volume of the patient cohort treated with thistechnique was only 38 ml. Overall, we believe that themorcellator remains the most efficient method of tissueremoval following enucleation. By employing the safetymeasures described earlier, morcellation can be per-
formed in a safe manner with little chance of morbidity.
Use of resectoscope beak to leverage adenoma upward
A 20 F, 3-way Foley catheter is placed at the conclusion ofthe case with the aid of a catheter guide. As continuousbladder irrigation is seldom required, the third port isplugged; however, it remains available should the need
saline should be connected to both inflow ports (outer
for irrigation arise. Currently, patients have their catheters
resectoscope sheath, rigid nephroscope) to ensure that the
removed early the following morning. HoLEP can be per-
bladder remains distended during the morcellation proc-
formed as an outpatient or overnight (i.e. short stay) pro-
ess. This is crucial, as collapse of the bladder can lead to
cedure, depending on patient preference.
significant injury to the bladder wall.
Under direct visualization, the tip of the morcellator is
Worldwide experience with the HoLEP technique has
inserted into the bladder and guided beneath a portion of
shown the procedure to be a safe and effective alternative
adenoma. The pedal is then depressed partially to trigger
for the surgical treatment of BPH. Although enucleation
the suction. Once a portion of adenoma is engaged by the
of prostate adenoma can be performed by a variety of
morcellator, the pedal is fully depressed to activate the
energy sources, only the holmium laser possesses the ideal
blades. It is important to keep the tip of the morcellatoranteriorly within the bladder and within the visual field atall times. The morcellator shaft should be moved in andout of the working channel in small increments androtated at times, to optimize engagement of tissue. Whenthe remaining tissue pieces are small, the surgeon shouldengage them with suction alone and pull them into theprostatic fossa, where morcellation can be done safely bypinning the tissue against the capsule. If difficulty isencountered in engaging these smaller pieces, theOlympus stone basket (Olympus America Incorporated,Melville, NY) or 11F Alligator forceps can be used to facil-itate their removal. Lastly, the Ellik evacuator is utilized toremove any remaining pieces of adenoma or clot. Thepatient is then given 20 mg of furosemide intravenouslyto promote urine flow during the immediate post-opera-tive period. If the procedure has been long or the capsuleis thin, it is advisable to give another 20 mg of furosemideintraoperatively to avoid fluid overload. On occasion, asmooth surfaced portion of adenoma fails to engage in
the morcellator. If it is too large to be removed with the
Morcellator inserted into offset nephroscope
basket or forceps, the adenoma should be moved into the
(page number not for citation purposes)
World Journal of Surgical Oncology 2003, 1
combination of cutting and coagulation. As a result, the
Gilling PJ, Mackey M, Cresswell M, Kennett K, Kabalin JN and Fraun-
risk of dilutional hyponatremia and the need for
transfusion are essentially eliminated. Hospital stays are
J Urol 1999, 162:1640-1644.
minimal, and almost all patients are able to be discharged
Kabalin JN, Mackey MJ, Cresswell MD, Fraundorfer MR and Gilling PJ
catheter-free. Although the learning curve for this proce-
J Endourol 1997, 11:291-293.
dure remains steep, the subsequent patient advantages
Matsuoka K, Iida S, Tomiyasu K, Shimada A and Noda S:
should continue to expand the appeal and usage of the
J Urol 2000,
163:515-518.
HoLEP technique within the urologic community. This
Matsuoka K, Iida S, Tomiyasu K, Shimada A, Suekane S and Noda S
technique has the potential to become the standard for
J Endourol 1998,
surgical management of BPH.
Mackey MJ, Chilton CP, Gilling PJ, Fraundorfer M and CresswellBr J
Urol 1998, 81:518-519.
Gan E, Costello A, Slavin J and Stillwell RG
JL has a financial interest and/or other relationship with
the Lumenis Corporation
Tech Urol 2000, 6:185-188.
Fraundorfer MR and Gilling PJ
Eur Urol 1998, 33:69-72.
RK – Study conception and drafting of manuscript
Moody JA and Lingeman JE: J Urol 2001, 165:459-462.
RP, SK, TS – Critical revision
Hochreiter WW, Thalmann GN, Burkhard FC and Studer UE: J Urol 2002,
ME, JL – Critical revision and supervision
Gilling PJ, Kennett K, Das AK, Thompson D and Fraundorfer MR
J Endourol 1998, 12:457-459.
Urology 2000, 56:3-6.
Moody JA and Lingeman JE:
Jacobsen SJ, Girman CJ, Guess HA, Rhodes T, Oesterling JE and Lie-
J Endourol 2000, 14:219-223.
J Urol 1996,
Gilling PJ, Kennett KM and Fraundorfer MR:
J Endourol
Urology 1996, 48:199-206.
Gilling PJ and Fraundorfe
Kuntz RM and Lehrich K:
Clin. Opin. Urol. 1998, 8:11-15.
Chan KF, Vassar GJ, Pfefer TJ, Teichman JM, Glickman RD, Weintraub
J Urol 2002, 168:1465-1469.
Lasers Surg Med 1999, 25:22-37.
Gilling PJ, Cass CB, Malcolm AR and Fraundorfer MR: J Endourol 1995, 9:151-153.
Kabalin JN, Gilling PJ and Fraundorfer MR: Mayo Clin Proc 1998, 73:792-
797.
Chun SS, Razvi HA and Denste Tech Urol 1995, 1:217-221.
Gilling PJ, Cass CB, Cresswell MD, Malcolm AR and Fraundorfer J Endourol 1996, 10:459-461.
Kabalin JN: J Endourol 1996, 10:453-457.
KabaliLasers Surg Med 1996, 18:221-224.
Mottet N, Anidjar M, Bourdon O, Louis JF, Teillac P, Costa P and Le
scientist can read your work free of charge
"BioMed Central will be the most significant development for
J Endourol 1999, 13:127-130.
disseminating the results of biomedical researc h in our lifetime."
Gilling PJ, Cass CB, Cresswell MD and Fraundorfer
Sir Paul Nurse, Cancer Research UK
Your research papers will be:
Urology 1996, 47:48-51.
Cresswell MD, Cass CB, Fraundorfer MR and Gilling PJ:
available free of charge to the entire biomedical community
peer reviewed and published immediately upon acceptance
N Z Med J 1997, 110:76-78.
Gilling PJ, Kennett KM and Fraundorfer MR
cited in PubMed and archived on PubMed Central
yours — you keep the copyright
J Endourol 2000,
14:757-760.
Submit your manuscript here:
(page number not for citation purposes)
Source: http://www.urologiarecife.com.br/artigos/011-Ho_YAG_laser_technical_update.pdf
math.helsinki.fi
Second order logic and set theory Both second order logic and set theory can be used as a foundation for mathematics, that is, as a formal language in which propositions ofmathematics can be expressed and proved. We take it upon ourselvesin this paper to compare the two approaches, second order logic on onehand and set theory on the other hand, evaluating their merits andweaknesses. We argue that we should think of first order set theoryas a very high order logic.
ssns.ca
Anna was visiting a friend in another city when strange things began to happen. She saw things that looked real, but later didn't seem real at all. She was so troubled by what she described as not feeling like herself that she woke her friend; together, they called Anna's parents. "She started to cry," says Anna's dad. "She was talking about things, but we didn't know where they were coming from."