Portalned.es
Childs Nerv SystDOI 10.1007/s00381-013-2341-z Surgical management of chronic traumaticpseudomeningocele of the craniocervicaljunction: case report Josué M. Avecillas-Chasin & Mwanabule Ahmed &Eric Robles Hidalgo & Luis Gómez-Perals Received: 19 November 2013 / Accepted: 2 December 2013 # Springer-Verlag Berlin Heidelberg 2013 Restoring the normal pattern of CSF circulation should be Purpose Chronic traumatic pseudomeningocele (PM) is a rare the aim of any neurosurgical intervention.complication of gunshot injuries of the craniocervical junctionin pediatric patients. Impairment of the CSF dynamics may Keywords Pseudomeningocele . Craniocervical junction .
cause severe symptoms and should be treated.
CSF fistula . Intracranial hypotension Methods We report the case of a 6-year-old girl who wasaccidentally shot in the neck during tribal clashes. On beingadmitted, she was neurologically intact with cerebrospinal fluid (CSF) leakage through the wounds. She underwentprimary closure of the wounds in a rural medical facility. After Gunshot injuries are common in developing countries. There two episodes of meningitis, CSF leakage resolved spontane- is currently a trend in tribal societies to use guns during ously. Nine months later, the patient was presented with a clashes, which not infrequently results in significant morbidity disfiguring mass growing in the posterior neck, severe head- or death in affected individuals [, ]. Gunshot injuries can aches, and constitutional symptoms such as loss of appetite involve the central nervous system and result in devastating and a failure to thrive.
neurologic damage, vascular injury, and meningitis [, Results Neurosurgical intervention was performed with the Traumatic pseudomeningocele (PM) is a rare complica- patient in the prone position. Occipital pericranium graft was tion of gunshot injury to the spine that can be managed by used to repair the defect, and the cavity of the PM was conservative measures and cerebrospinal fluid (CSF) diver- obliterated with muscle layers. The patient's symptoms im- sion in the earliest stages ]. Conservative management is proved at 1 year follow-up without PM recurrence.
therefore usually ineffective in the chronic stages of PM after a Conclusion This is a rare presentation of gunshot injuries in cavity is established, with resulting intracranial hypotension an environment with limited neurosurgical resources.
and CSF hypovolemia Here, we report a case of chronictraumatic PM of the craniocervical junction (CCJ) in severelysymptomatic child with severe symptoms due to a neck mass J. M. Avecillas-Chasin (*) effect and impairment CSF dynamics. Surgical repair of the Department of Neurosurgery, Institute of Neurosciences, Hospital traumatic pseudomeningocele resulted in a symptom-free Clínico San Carlos, Prof. Martín Lagos s/n, 28040 Madrid, Spain J. M. Avecillas-Chasine-mail: [email protected] M. AhmedDepartment of General Medicine, Coast Province General Hospital, A 6-year-old girl was involved in tribal clashes and was injured laterally by a gunshot in the posterior aspect of theneck at the CCJ level. The patient remained neurologically E. Robles Hidalgo L. Gómez-Perals intact and clear fluid was leaking from the wound upon Department of Neurosurgery, Hospital Universitario Nuestra Señorade la Candelaria, Santa Cruz de Tenerife, Spain reporting to the hospital. The patient underwent primary
closure of the wounds in a rural medical facility. Three days
fluid drained, allowing us to obtain good visualization of the
later, the wound became infected and CSF leakage from the
defect between the inferior border of the foramen magnum and
wound was evident. One month later, after two episodes of
the superior border of the posterior arch of C1. The extensive
meningitis, CSF leakage improved spontaneously. Nine
cavity had no free dural edges, and the posterior aspect of the
months later, the patient was readmitted for a disfiguring
medulla oblongata was entirely exposed (Fig.
pulsating mass on the neck, severe lingering headaches, loss
To repair the dural defect, an occipital 6×3 cm pericranium
of appetite, and failure to thrive during the last 6 months. A
graft was obtained and sutured to the border of the defect with
head computed tomography (CT) scan showed a PM of the
silk stitches at a 3 mm interval. To obliterate the dead space, the
CCJ widely communicated with the cisterna magna (Fig. ).
three muscular layers were reapproximated with sutures over
On examination, the patient was alert with reactive pupils.
the pericranium graft covering the defect. The fascial plane then
Furthermore, cranial nerve examination revealed no abnormal-
was closed with interrupted sutures. Finally, the skin was closed
ities, including no evidence of paresis or hypoesthesia in the
with vertical mattress stitches. At the immediate postoperative
limbs. After a thorough evaluation of the case, we decided to
period, the patient was neurologically intact without CSF fistu-
repair the defect due to the lack of improvement 9 months after
la. Eight months later, the patient remained asymptomatic with-
the injury. With the patient in prone position and the head fixed
out PM (Fig. ). Due to financial issues, the patient has not been
with the three-point Mayfield-Kees fixation device, a midline
able to obtain a control CT scan of the head. However, due to
skin incision was performed from 4 cm above the occipital
the absence of symptoms and no PM recurrence, control imag-
protuberance to the C2 vertebrae (Fig. We performed a
ing studies are not mandatory for this patient, mainly in devel-
careful dissection of cervical soft tissues and muscles. A T-
oping countries with healthcare services costly for patients.
shaped incision was made at the fascial plane and muscles.
Then, a subperiosteal dissection of the cervical spine wascarried out in order to expose the area from occipital squama
to the spinous process of the C2 vertebrae. Thus, we gainedaccess to the whole occipitocervical area which was occupied
We present a case of traumatic PM as a result of gunshot
by a large cavity full of CSF. The cyst was penetrated and the
wound in the neck that caused severe symptoms during
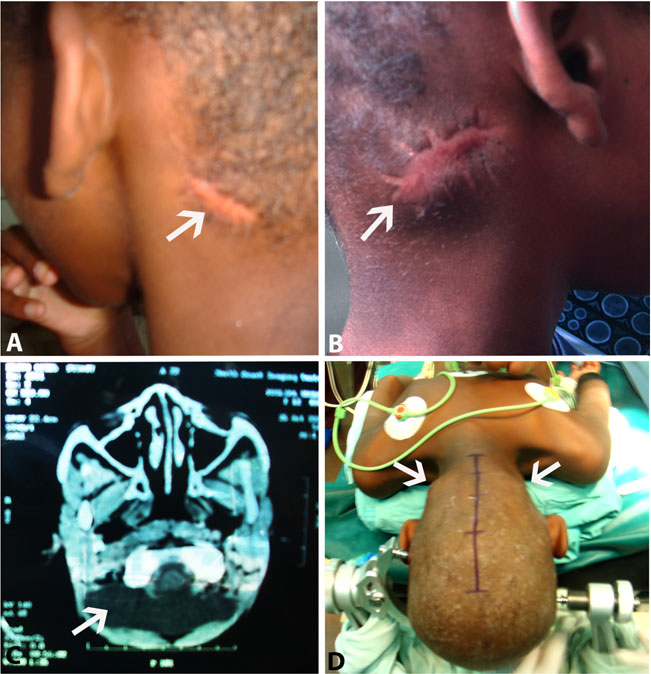
Fig. 1 Photograph of the childwith traumatic PM. a The scars ofthe penetrating injury in theposterior aspect of the neck areshown with the typical smallerentrance wound of the bullet andb larger exit wound. c CT scan ofthe head showed the PM (arrow).
d The child was operated in proneposition with midline incision4 cm over the occipital eminenceto the C2 vertebrae. We can alsosee the swelling of the scars due toPM (arrows)
angiography and endovascular treatment if necessary. CT scanof the injured spine segment could be important to evaluatethe need for surgical intervention []. On the other hand,when there is no neurologic deficit, infection, or CSF leakage,conservative management is recommended
The most common traumatic PM is due to brachial and
lumbosacral plexus injury Atlanto-occipital dislocationmay cause secondary PM due to dural lacerations in the zoneof the trauma that are associated with neurologic compromisein some cases , ]. In this setting, it has beenreported that hydrocephalus and syrinx are associated withthe PM [. These pathologic associations highlight theconcept of an alteration of the intracranial dynamics due toan ectopic cavity filled with CSF acting as a large reservoirthat produces a decrease in intracranial pressure and impair-ment of the CSF reabsorption in the arachnoid granulations,which act as pressure-dependent valves driven by the cardio-respiratory rhythm ]. The mechanism by which the CSFis contained in the cavity of the pseudomeningocele remainsunclear. It has been hypothesized that a ball-valve mechanismin the site of the dural laceration may play a role in thepersistence of the cavity Some authors argue that PMresults from arachnoid-intact herniation through the duraldefect; this phenomenon is referred to as "true meningoceles"
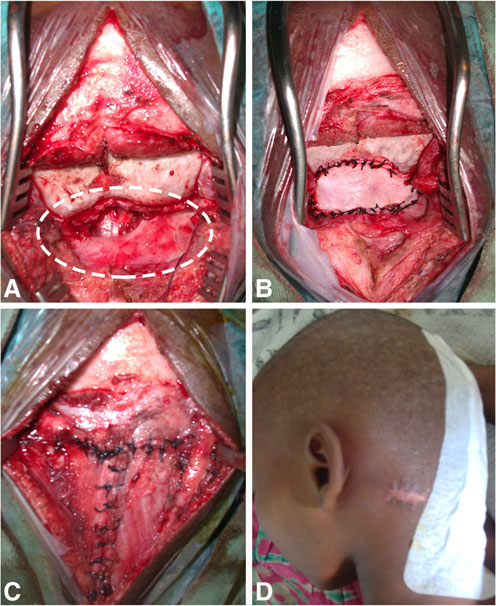
Fig. 2 Intraoperative photos. a The circle shows the extent of the PM.
The medulla oblongata was entirely exposed. b Occipital pericranium
]. CSF collections may tend to be spontaneously reabsorbed
flap was used for reconstruction; the graft was sutured around the defect.
in the soft tissue, but when a cavity is established, the
c The muscular layers were opened in a T-shaped fashion, and they were
CSF becomes more difficult to reabsorb and less likely
closed upon the graft to obliterate the cavity. d 5 days later, the child was
to be resolved with conservative treatment. In our case,
asymptomatic without CSF fistula
we did not find any dural laceration; however, we didfind a large cavity filled with CSF that had developed,
6 months. Impairment of CSF dynamics was the main cause
with neovascularization in the walls widely connected
of her clinical manifestations, and restoring the normal CSF
with the cisterna magna.
circulation was the aim of the surgical approach despite of a
There are many strategies to treat CSF disorders associated
situation with limited neurosurgical resources. Regarding the
with a PM. Direct dural repair is not always possible because
mechanism of the injury, the bullet went laterally through the
the location of the dural tears may not be readily accessible for
posterior cervical muscles with a small left lateral entry zone
a given surgical approach. In the acute setting, traumatic PM
and a bigger right lateral exit wound due to the conic effect of
could be treated with conservative measures, such as bed rest
the bullets , The bullet passed below the posterior rim of
and acetazolamide, or with more aggressive management such
the foramen magnum and the upper surface of the C1 posterior
as a blood patch, subarachnoid external drainage, or a lumbo-
arch piercing the dura but leaving intact the cervical spinal
peritoneal shunt. These interventions are usually quite effec-
cord, which led to the formation of a big intramuscular cavity
tive in the early stages of a PM when dural tears are apposed,
of the CSF []. Usually, this type of injury may cause severe
and the aim of the intervention is to decrease the pressure of
damage to the spinal cord. Indirect injuries may also occur due
CSF pulsations favoring spontaneous closure
to fractures and dislocations of the spine, and the outcome will
Some authors have reported severe long-standing headaches
depend on the spinal cord damage The initial manage-
which are recalcitrant to conservative treatment in patients
ment of this type of injury will require immediate debridement
who have been undergone lumbar puncture. When an occult
of the tissues. The evident bullet fragments should be carefully
CSF fistula is diagnosed, these authors advocate surgical
removed. Infection, hematoma, and persistent CSF leakage
repair of this type of dural injury to eliminate the headaches
should also be managed aggressively to avoid secondary
]. Otherwise, an epidural blood patch is one of the
damage of the spinal cord [,
strategies for use in acute or subacute stages of a PM that has
Penetrating trauma of the cervical spine is usually associ-
been reported as an effective approach in many types of CSF
ated with spine instability and vascular injuries. To address
collections; it remains one of the first invasive measures of
this, the appropriate workup should be carried out with
choice when a PM is present ].
When a long-standing PM becomes an encapsulated CSF
4. Doctor VS, Farwell DG (2007) Gunshot wounds to the head and
cavity producing severe symptoms of intracranial hypoten-
neck. Curr Opin Otolaryngol Head Neck Surg 15(4):213–218
5. Gutiérrez-González R, Boto GR, Pérez-Zamarrón A, Rivero-Garvía
sion, surgical repair is indicated with the aim of sealing the
M (2008) Retropharyngeal pseudomeningocele formation as a trau-
defect and eliminating the dead space to avoid recurrence ].
matic atlanto-occipital dislocation complication: case report and re-
Conservative measures may be ineffective due to integration
view. Eur Spine J 17(Suppl 2):S253–S256
of the pathological cavity with CSF spaces in the intracranial
6. Hawk MW, Kim KD (2000) Review of spinal pseudomeningoceles
and cerebrospinal fluid fistulas. Neurosurg Focus 9(1):e5
compartment. In this case, it is insufficient to only relieve
7. Hugenberg F, Anjango WO, Mwita A, Opondo D (2007) Firearm
pressure from the defect since a chronic PM does not usually
injuries in Nairobi, Kenya: who pays the price? J Public Health
have closely apposed free dural edges that can close sponta-
Policy 28(4):410–419
neously [The operative technique to repair the PM includes
8. Khan MB, Kumar R, Irfan F, Bin IA, Bin BME (2013) Civilian
craniocerebral gunshot injuries in a developing country: presentation,
primary closure of the dural defect with or without graft
injury characteristics, prognostic indicators, and complications.
depending on the size of the defect using 4.0 nonabsorbable
World Neurosurg. doi
sutures at a 2 to 5-mm interval Sealant and fibrin glue can
9. Misra SN, Morgan HW, Sedler R (2003) Lumbar myofascial flap for
be used when leakage persists despite adequate suture closure.
pseudomeningocele repair. Neurosurg Focus 15(3):E13
10. Mokri B (1999) Spontaneous cerebrospinal fluid leaks: from intra-
In our case, this was neither possible nor necessary because of
cranial hypotension to cerebrospinal fluid hypovolemia—evolution
successful closure with sutures and the lack of non-autologous
of a concept. Mayo Clin Proc 74(11):1113–1123
materials in hospitals with limited resources. The muscular
11. Naso WB, Cure J, Cuddy BG (1997) Retropharyngeal
planes should be closed in two or three layers to obliterate the
pseudomeningocele after atlanto-occipital dislocation: report of twocases. Neurosurgery 40(6):1288–1290, discussion 1290–1
dead space between the dural repair and soft tissues [].
12. Natale M, Bocchetti A, Scuotto A, Rotondo M, Cioffi FA (2004) Post
Drainage should be avoided because it could promote the
traumatic retropharyngeal pseudomeningocele. Acta Neurochir
persistence of communication between the intra- and
(Wien) 146(7):735–739
extradural space and results in high risk of infection.
13. Nurboja B, Rezajooi K, Newton MC, Casey ATH (2009) Spinal
meningocele due to iatrogenic dural puncture during epidural anal-
In summary, traumatic PM is a rare complication of gun-
gesia for childbirth: 5-year history of headache with a spinal etiology.
shot wounds involving the CCJ. In the pediatric population,
J Neurosurg Spine 11(6):764–767
impairment of the CSF dynamics may cause severe symptoms
14. Paternoster G, Massimi L, Capone G, Tamburrini G, Caldarelli M, Di
and should be treated with the aim of restoring the normal
Rocco C (2012) Subcutaneous blood patch for iatrogenic suboccipitalpseudomeningocele following decompressive suboccipital
pattern of CSF circulation to reduce the symptoms. In chronic
craniectomy and enlarging duroplasty for the treatment of
stages, surgical treatment with obliteration of the cavity and
Chiari I malformation. Technical note. Childs Nerv Syst 28(2):287–
closure of the defect is mandatory due to the high probability
of failure through conservative or less aggressive measures.
15. Pinto A, Brunese L, Scaglione M, Scuderi MG, Romano L (2009)
Gunshot injuries in the neck area: ballistics elements and forensicissues. Semin Ultrasound CT MRI 30(3):215–220
The authors would like to acknowledge the support
16. Reed CM, Campbell SE, Beall DP, Bui JS, Stefko RM (2005)
of the Neurosurgery, Education and Development (NED) Foundation for
Atlanto-occipital dislocation with traumatic pseudomeningocele
humanitarian missions in Eastern Africa.
formation and post-traumatic syringomyelia. Spine 30(5):128–133
Conflict of interest
17. Robertson DP, Simpson RK (1992) Penetrating injuries restricted to
the cauda equina: a retrospective review. Neurosurgery 31(2):265–269, discussion 269–70
18. Rosenfeld JV (2002) Gunshot injury to the head and spine. J Clin
Neurosci 9(1):9–16
19. Schievink WI, Maya MM (2013) Ventral spinal cerebrospinal fluid
1. Bono CM, Heary RF (2004) Gunshot wounds to the spine. Spine J
leak as the cause of persistent post-dural puncture headache in
children. J Neurosurg Pediatr 11(1):48–51
2. Brodbelt A SM (2010) An Anatomical and physiological basis for CSF
20. Spitz DJ, Ouban A (2003) Meningitis following gunshot wound of
pathway disorders. In: Mallucci C, Sgouros S (eds) Cerebrospinal fluid
the neck. J Forensic Sci 48(6):1369–1370
disorders. Informa Healthcare USA, Inc, New York, pp 1–21
21. Syre P, Rodriguez-Cruz L, Desai R, Greene KA, Hurst R, Schuster J,
3. Demetriades D, Theodorou D, Cornwell E, Asensio J, Belzberg H,
Malhotra NR, Marcotte P (2013) Civilian gunshot wounds to the
Velmahos G, Murray J, Berne TV (1996) Transcervical gunshot inju-
atlantoaxial spine: a report of 10 cases treated using a multidisciplinary
ries: mandatory operation is not necessary. J Trauma 40(5):758–760
approach. J Neurosurg Spine 19(6):1–8
Source: http://www.portalned.es/en/images/stories/documents/Ciencias/Surgical%20management%20of%20chronic%20traumatic.pdf
fkn.org.il
This article appeared in a journal published by Elsevier. The attached copy is furnished to the author for internal non-commercial research and education use, including for instruction at the authors institution and sharing with colleagues. Other uses, including reproduction and distribution, or selling or licensing copies, or posting to personal, institutional or third party
caipisa.it
Sede: via Cisanello 2, 56124 Pisa CLUB ALPINO ITALIANO Anno XXX - Numero 1 - 2011 I monumenti di Piazza del Duomo sullo sfondo delle Apuane innevate. Questa bella fotografia scattata da Enrico Mangano dalla terrazza dell'Hotel Duomo costituisce l'immagine di copertina del volumetto "Le nostre Alpi", che dopo una lunga attesa ha visto finalmente la luce. La pubblicazione, a carattere essenzialmente fotografico, è stata presentata durante l'assemblea annuale del