A clinical and radiographic case series of implants placed with the simplified minimally invasive antral membrane elevation technique in the posterior maxilla
Our reference: YJCMS 1862 AUTHOR QUERY FORM Please e-mail or fax your responses and any corrections to: Article Number: 1862 Fax: +31 2048 52789 Please check your proof carefully and mark all corrections at the appropriate place in the proof (e.g., by using on-screenannotation in the PDF file) or compile them in a separate list. Note: if you opt to annotate the file with software other thanAdobe Reader then please also highlight the appropriate place in the PDF file. To ensure fast publication of your paper pleasereturn your corrections within 48 hours.For correction or revision of any artwork, please consult .
Any queries or remarks that have arisen during the processing of your manuscript are listed below and highlighted by flags inthe proof.
Query / Remark: Click on the Q link to find the query's location in text Please insert your reply or correction at the corresponding line in the proof Please provide organisation details for authors, "Udatta Kher, Kostantinos Siormpas, Ziv Mazor" if any.
The citation "Sakka et al., 2011" has been changed to match the author name/date in the reference list.
Please check.
Please provide the volume number or issue number or page range for the bibliography in Refs. "Hartlevet al., 2013, Jeong et al., 2014, Kotsakis et al., 2012, Nickenig et al., 2014, Sununliganon et al., 2014".
Please note that as per the journal style, if there are more than 6 authors, the first 6 author names are listedfollowed by ‘et al.' if the author group consists of 6 authors or fewer, all author names should be listed.
Therefore, in Ref(s). "Cochran et al, 2002; Galindo Moreno et al, 2008; Hartlev et al, 2013; Kfir et al,2009a; Kfir et al, 2009b; Vance et al, 2004" .Please list all names for up to 6 authors. For more than 6authors, use ‘et al.' after the first 6 authors.
Please confirm that given names and surnames have been identified correctly.
Please check this box or indicateyour approval if you have no corrections to make to the PDF file Thank you for your assistance.

YJCMS1862_proof ■ 6 September 2014 ■ 1/6
Contents lists available at
Journal of Cranio-Maxillo-Facial Surgery
A clinical and radiographic case series of implants placed with the
simplified minimally invasive antral membrane elevation technique in
the posterior maxilla
Kher , Andreas L. Ioannou *, Tarun Kumar Kostantinos Siormpas
Miltiades E. Mitsias , Ziv Mazor Georgios A. Kotsakis
Private Practice, Mumbai, India
b Advanced Education Program in Periodontology, University of Minnesota, United States
Division of Periodontology, Bapuji Dental College & Hospital, Davangere, India
Private Practice, Larissa, Greece
e Department of Periodontology & Implant Dentistry, New University College of Dentistry, NY, United States
Private Practice, Ra'anana, Israel
The aim of the present case series was to evaluate a simpli
fied minimally invasive transalveolar sinus
Paper received 2 March 2014
elevation technique utilizing calcium phosphosilicate (CPS) putty for hydraulic sinus membrane eleva-
Accepted 15 August 2014
tion. The simplified minimally invasive antral membrane elevation technique is based on the application
Available online xxx
of hydraulic pressure via a viscous bone graft that acts as an incompressible fluid.
In this retrospective study, 21 patients (mean age: 48.5 ± 12 years) consecutively treated with the
simplified minimally invasive transalveolar sinus elevation technique were evaluated. 28 tapered im-
plants were placed in posterior maxillary sites with less than 6 mm of residual bone height as deter-
Maxillary sinus/surgery
mined radiographically on cone beam volumetric tomographs. No sinus membrane perforations were
Surgical procedures
noted and none of the patients complained of symptoms of sinusitis post-operatively (0%). The mean
Minimally invasive
gain in bone height post-operatively was 10.31 ± 2.46 mm (p < 0.001). All implants successfully inte-
Putty bone substitute
grated (100% success rate) and were loaded with cement-retained prostheses.
The proposed technique is a simple, efficacious, minimally invasive approach for sinus elevation that
can be recommended for sites with at least 3 mm of residual height.
2014 Published by Elsevier Ltd on behalf of European Association for Cranio-Maxillo-Facial Surgery.
extraction, but is unrealistic for sites where anatomic limitations
require more involved procedures (). One such
Dental implant therapy has revolutionized the rehabilitation of
case is the edentulous posterior maxilla.
both the form and the function of missing teeth. In contemporary
Following extraction of teeth in the maxillary posterior region,
dental practice, implant dentistry is recognized as the
pneumatization of the maxillary sinus frequently occurs (
" for the rehabilitation of edentulous sites
). Depending on the degree of
). Patients' demands frequently dictate minimally invasive
pneumatization in conjunction with the amount of coexisting
surgery and timely delivery of restoration (
ridge resorption in an apical-coronal direction, different surgical
). This dual goal can be readily delivered by
methods are employed for sinus lift surgery
concepts such as immediate implant placement, or non-submerged
implant placement in sites with adequate bone volume post-
tionally, indirect, or transalveolar sinus
floor elevation techniques
are utilized when less than 5 mm of gain in bone height are
sought, while more aggressive direct, or lateral-window ap-
proaches are utilized in more advanced cases
* Corresponding author. Advanced Education Program in Periodontology,
University of Minnesota, 515 Delaware Street SE, Minneapolis, MN 55455, United
Direct sinus augmentation techniques have been shown to yield
States. Tel.: þ1 651 395 9200.
E-mail address: (A.L. Ioannou).
very favorable outcomes in regards to bone regeneration in the
1010-5182/ 2014 Published by Elsevier Ltd on behalf of European Association for Cranio-Maxillo-Facial Surgery.
Please cite this article in press as: Kher U, et al., A clinical and radiographic case series of implants placed with the simplified minimally invasive
antral membrane elevation technique in the posterior maxilla, Journal of Cranio-Maxillo-Facial Surgery (2014), http://dx.doi.org/10.1016/j.jcms.2014.08.005
YJCMS1862_proof ■ 6 September 2014 ■ 2/6
U. Kher et al. / Journal of Cranio-Maxillo-Facial Surgery xxx (2014) 1e6
sinus as well as very good success rates for implants placed in
placement were included in this study. A minimum of 2 mm of
bone height from the crest of the ridge to the floor of the sinus,
of the major drawbacks associated with this type of technique is
and 5 mm of minimum bone width were set as inclusion criteria.
patient satisfaction. Not only do patients undergo a more involved
In addition, patients had to be healthy, non-smokers, with no
procedure that has greater morbidity than conventional implant
history of acute sinusitis or sinus pathology. Patients with
placement, but they usually have to wait for several months prior to
asymptomatic mild thickening of the sinus mucosa were included.
having their chief concern addressed, restoration of their functional
Exclusion criteria included history of previous maxillary sinus
surgery, chronic intake of any medication that affects bone heal-
In a hypothetical case of ridge atrophy with coexisting pneu-
ing (chronic steroid regimen, oral or IV bisphosphonates, etc.),
matization of the sinus it is not infrequent for less than 5 mm of
active periodontal disease, or periapical pathology of the adjacent
residual bone height to remain in the posterior maxilla. In such a
case a patient would routinely undergo direct sinus augmentation
All patients were evaluated preoperatively for the need for sinus
followed by implant placement approximately 6e9 months later,
augmentation via cone beam tomography scans (CBCTs). The in-
they would finally have the implant restored after 3e4 months of
dications for the procedure and possible complications were
healing, giving a total treatment time of approximately 1 year. It is
reviewed with the patients and all patients agreed to proceed and
only reasonable that this estimated waiting time would seem
signed a consent form.
protracted to the majority of patients. In order to address this
concern there are recent reports in the literature showing that the
2.2. Surgical technique and follow-up
controlled elevation of the sinus floor using hydraulic pressure may
extend the indications for transalveolar sinus augmentation tech-
Patients were treated under local anesthesia and were pre-
niques and reduce treatment time for patients
medicated with a loading dose of amoxicillin/clavulanate potas-
Utilizing the minimally invasive antral membrane
sium administered 1 h prior to the surgical appointment
elevation technique, were successful in achieving
(875 mg/125 mg). Transcrestal sinus floor elevations were per-
up to, or even beyond, 10 mm of gain in vertical bone height in a
formed using a modification of the Summer's technique
series of published reports (The
). The pre-operative height of the residual ridge
rationale behind the use of a balloon is the even distribution of
was assessed radiographically by an experienced implant surgeon
hydraulic pressure at the membraneebone interface that results in
. Local anesthesia was administered using 2% lidocaine
atraumatic and safe elevation of the schneiderian membrane.
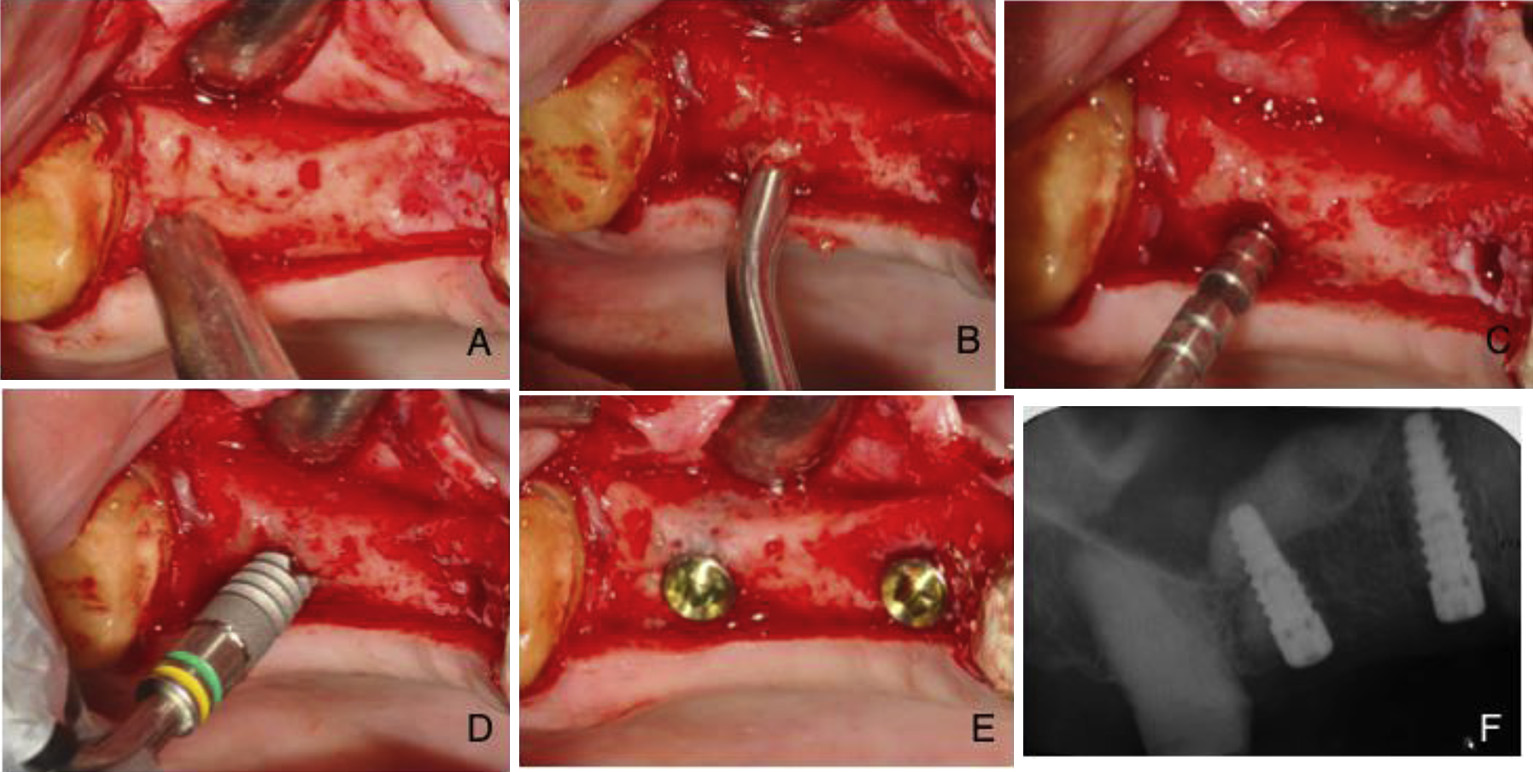
with 1:100,000 epinephrine to aid hemostasis of the area. Full
Although efficacious, this technique has not become the standard
thickness mucoperiosteal flaps were elevated in the posterior
method for sinus elevation surgical procedures, possibly because of
maxilla in order to gain access to the alveolar crest (A). An
the need to purchase specialized equipment and for specific
osteotomy was initiated at the ridge crest using a 2.0 mm pilot
drill. The drill was stopped 1 mm short of the estimated height of
The number of different surgical techniques for sinus
the sinus floor. A periapical X-ray was obtained to verify the exact
augmentation is only surpassed by the number of biomaterials
position of the drill in proximity to the sinus floor. The osteotomy
that have been used to overcome the challenge of insufficient
was further widened using the drilling sequence recommended
vertical bone height in the posterior maxilla
by the implant manufacturer (Tapered Internal, BioHorizons,
). Various bone-grafting
Birmingham, AL, USA). A small quantity of approximately 0.2 cm3
materials are frequently used in sinus lift procedures, including
of CPS putty (NovaBone Dental Putty, NovaBone Products, Ala-
autogenous bone, allografts, xenogeneic bone, and alloplastic bone
chua, FL, USA) was delivered in the osteotomy via a narrow-
tipped cartridge delivery system to act as a cushion prior to
). Recent data have
tapping the sinus floor, and a 3 mm concave osteotome with
shown that bone substitutes displaying a putty-like consistency
depth markings and a mallet were used to carefully fracture the
can present a valuable alternative in bone-grafting procedures
floor of the sinus ,C). Care was taken not to push the
osteotome into the sinus cavity to avoid inadvertent perforation
The handling characteristics of putty bone substitutes
of the sinus lining. Following the green-stick fracture of the floor
have expanded the available array of treatment options for bone
of the sinus, the bone substitute was directly injected into the
grafting in narrow spaces, and their viscoelastic properties may be
prepared sinus cavity via the cartridge delivery system. The car-
exploited to increase the safety and predictability of sinus lift
tridge tip fitted tightly in the osteotomy and allowed the insertion
pressure due to injection of the graft to be delivered directly to
The aim of the present case series was to evaluate a minimally
the fractured inferior border of the sinus floor. 0.5 cm3 of CPS
invasive transalveolar sinus elevation technique utilizing calcium
putty was carefully injected into the osteotomy (). The hy-
phosphosilicate (CPS) putty for hydraulic sinus membrane
drostatic pressure exerted by the putty resulted in an atraumatic
elevation of the sinus floor. CPS putty was added in increments
until adequate elevation of the schneiderian membrane was seen
2. Materials and methods
on intra-operative radiographs. An appropriately sized implant
was placed at the level of the osseous crest using a manual torque
2.1. Patient selection
wrench for enhanced tactile sensation (,E). The implants
were initially engaged into the remaining native bone at the crest
In this retrospective study, 21 patients consecutively treated in
of the ridge and then slowly twisted in to engage in the viscous
a dental clinic with a simplified, minimally invasive technique for
CPS putty at the apical aspect of the osteotomy. Cover screws
transalveolar sinus elevation were evaluated. Data related to age,
were placed and primary flap closure was achieved utilizing a
sex, implant location, intra-operative or post-operative compli-
single interrupted suturing technique.
cations, implant stability, implant success and radiographic bone
Postoperative instructions included oral administration of
changes were recorded for all patients. Patients with treatment
amoxicillin/clavulanate potassium (500 mg/125 mg three times a
plans for sinus elevation surgery with simultaneous implant
day) and ibuprofen (400 mg four times a day) for the first week
Please cite this article in press as: Kher U, et al., A clinical and radiographic case series of implants placed with the simplified minimally invasive
antral membrane elevation technique in the posterior maxilla, Journal of Cranio-Maxillo-Facial Surgery (2014), http://dx.doi.org/10.1016/j.jcms.2014.08.005
YJCMS1862_proof ■ 6 September 2014 ■ 3/6
U. Kher et al. / Journal of Cranio-Maxillo-Facial Surgery xxx (2014) 1e6
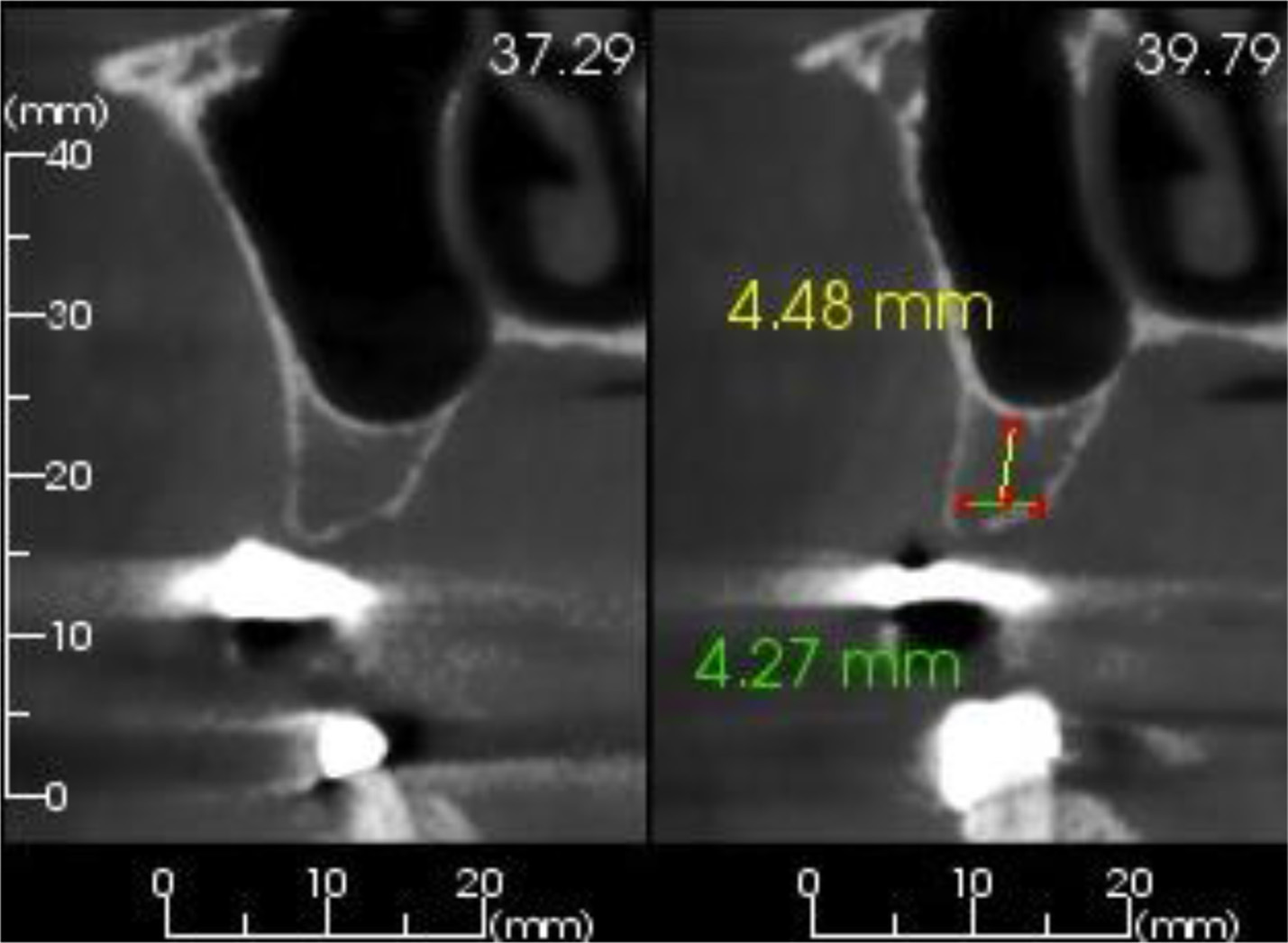
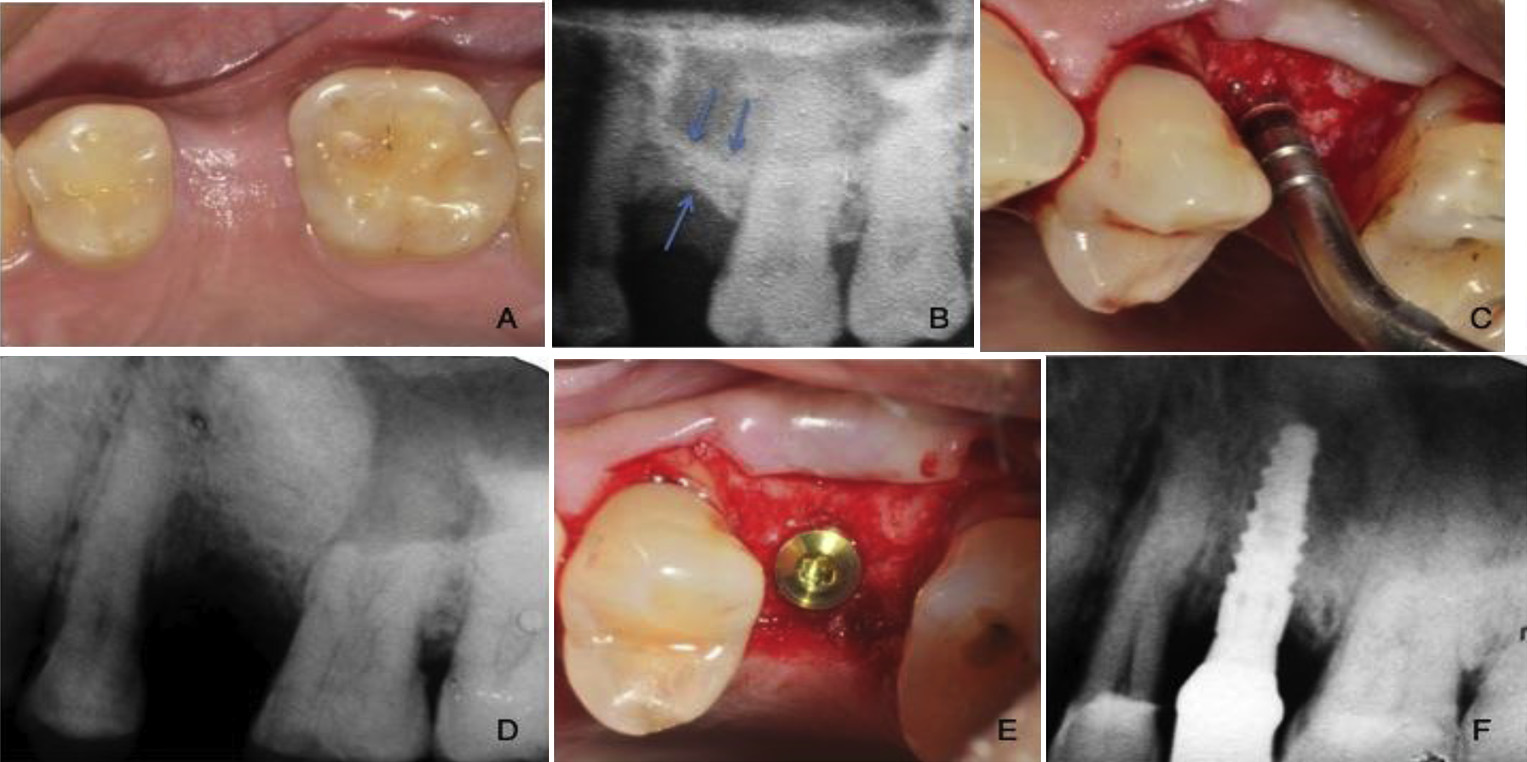
Fig. 1. Pre-operative assessment of the cross-sectional radiographic image revealed less than 6 mm of preoperative height on the edentulous site.
post-operatively. Chlorhexidine rinses were prescribed twice daily
for the above measurements (Image J, National Institutes of Health,
for 2 weeks. The patients were instructed to limit themselves to a
Bethesda, Maryland, USA).
soft diet for the first 2 weeks after surgery.
All patients were followed-up and assessed for implant survival
Patients were followed-up at 24 h, 10 days and 3 months after
and sinus complications on an individualized recall basis. Patients
the surgery for post-surgical evaluation. Second stage surgery was
were urged to contact the implant surgeon if any complication
scheduled at 3e5 months post-sinus lift. During the implant
arose between the recall appointments. Implant success was eval-
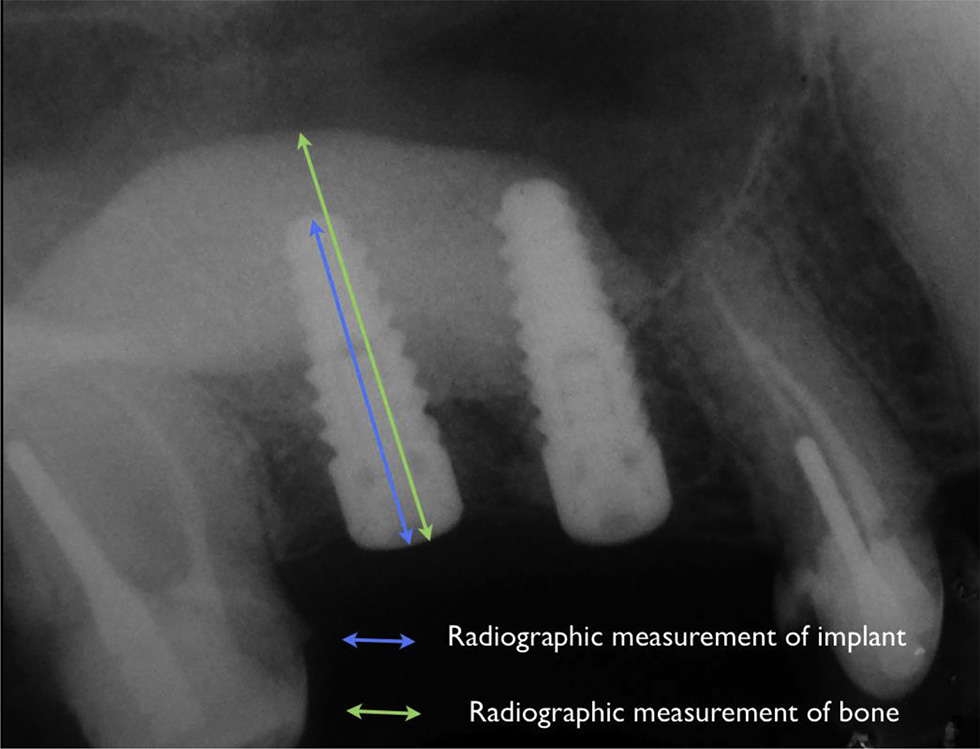
uncovery appointment a periapical radiograph was taken to eval-
uated clinically according to the criteria of .
uate the amount of vertical bone height gain and assess radio-
Briefly, the examination consisted of clinical detection of implant
graphic signs of implant integration (Radiographic
mobility with the application of horizontal jiggling forces with the
measurements of bone height from the crest to the floor of the
rear end of two periodontal probes. Assessment of the peri-implant
sinus where calculated twice by the same examiner at two different
tissues was performed visually for signs of erythema and/or edema
time intervals and the means of both measurements were reported.
and by palpation of the tissues surrounding the implant area.
The measurements included the scaling of the measured gain in
Additionally, periapical radiographs were obtained to ascertain the
vertical bone height based on the radiographic magnification of the
absence of a continuous radiolucency around the implant. Patients
implant to reduce any bias associated with possible elongation of
were also interviewed for subjective symptoms and evaluation of
the periapical radiographs. Specialized imaging software was used
Fig. 2. (A) Intraoperative view of the residual ridge prior to initation of the osteotomy; (B) the tip of the cartridge inserted into the osteotomy site; (C) application of the osteotome
to produce the required elevation of the sinus
floor; (D) implant placement; (E) implants placed at the level of the osseous crest; (F) postoperative radiograph showing significant
elevation of the sinus floor. Note the even fill of the sinus antrum by the flow of the viscous putty.
Please cite this article in press as: Kher U, et al., A clinical and radiographic case series of implants placed with the simplified minimally invasive
antral membrane elevation technique in the posterior maxilla, Journal of Cranio-Maxillo-Facial Surgery (2014), http://dx.doi.org/10.1016/j.jcms.2014.08.005
YJCMS1862_proof ■ 6 September 2014 ■ 4/6
U. Kher et al. / Journal of Cranio-Maxillo-Facial Surgery xxx (2014) 1e6
version 3.0.1, 2013 (2013-05-16, The R Foundation for Statistical
Computing, Vienna, Austria).
A total of 29 implants (Tapered Internal, BioHorizons, Birming-
ham, AL, USA) were placed in 21 consecutively treated patients
with the simplified minimally invasive transalveolar sinus eleva-
tion technique. The average patient age was 48.5 ± 12 years, and 9
patients were female. None of the patients were smokers. The re-
cord of adverse events included mild to moderate postoperative
edema for the first two or three postoperative days in most pa-
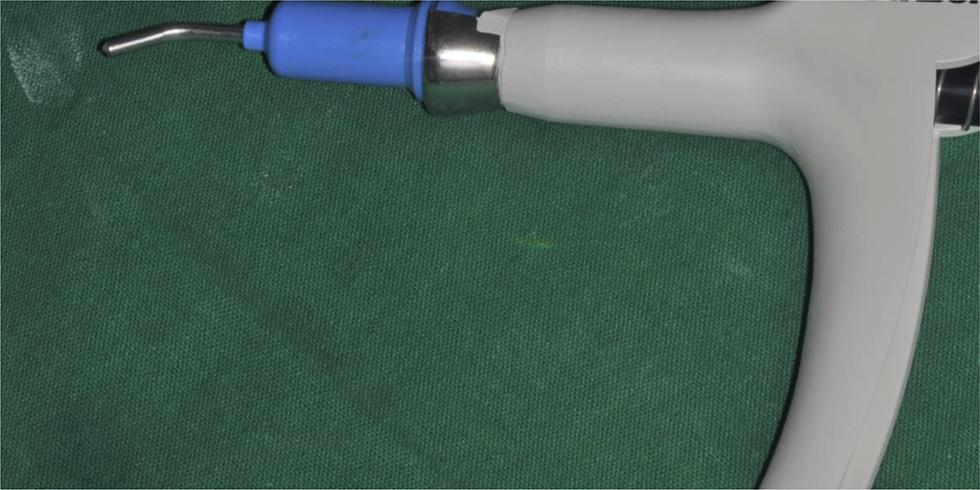
Fig. 3. Note the narrow tip of the delivery system that allows intimate contact of the
tients, and flap dehiscence in one patient that was caused by
cartridge with the walls of the osteotomy.
trauma during mastication. No reports of hematoma, severe pain,
or paroxysmal vertigo were noted in the present case series. The
sinus elevation was combined with CPS putty in all cases. No sinus
2.3. Statistical analysis
membrane perforations were noted and none of the patients
complained of symptoms of sinusitis post-operatively (0%). The
Patient characteristics and implant success were presented
mean preoperative bone height was 4.34 ± 1.16 mm, while a sig-
descriptively. The gain in bone height post-sinus surgery was
nificant gain of 10.31 ± 2.46 mm was noted post-operatively
assessed with a Wilcoxon signed-rank test. The alpha level was set
¼ 0.05. Calculations were performed with statistical software, R
Of the 29 implants placed, five were placed in 2nd premolar
sites, 19 in 1st molar sites and five in 2nd molar sites. 28 of the 29
implants were placed simultaneously with the transalveolar sinus
elevation with good to optimal primary implant stability in sites
with residual bone height ranging from 2.8 mm to 6.5 mm. The
remaining implant was placed after 6 months of healing due to the
poor bone quality at the site. The residual bone height during the
sinus augmentation surgery was 2.5 mm and the bone quality was
deemed as poor (class IV) during implant site preparation, thus
implant placement was aborted and the osteotomy was filled with
CPS putty after elevation of the sinus to 13.5 mm. After 6 months of
healing the site was re-entered and the implant was successfully
placed with adequate primary stability. The implant was func-
tionally loaded after 4 months of healing and remained successful
throughout the follow-up period. Due to delayed implant place-
ment this fixture was excluded from the analysis. All implants
placed in this case series were left to heal for 4e5 months after
implant placement and were then loaded with cement-retained
prostheses. All of the simultaneously placed implants (28/28)
were clinically stable and had no signs of peri-implant disease
Fig. 4. Description of the radiographic assessment technique utilizing the known
during a follow-up period of at least 1 year post-placement (min-
implant length as reference for accuracy of measurements.
imum of 9 months post-loading) (100% success rate).
Fig. 5. (A) Clinical photo prior to treatment; (B) preoperative radiograph; (C) utilizing the osteotomy approach; (D) postoperative radiograph; (E) implant placed at the level of the
osseous crest; (F) postoperative radiograph showing final prostheses.
Please cite this article in press as: Kher U, et al., A clinical and radiographic case series of implants placed with the simplified minimally invasive
antral membrane elevation technique in the posterior maxilla, Journal of Cranio-Maxillo-Facial Surgery (2014), http://dx.doi.org/10.1016/j.jcms.2014.08.005
YJCMS1862_proof ■ 6 September 2014 ■ 5/6
U. Kher et al. / Journal of Cranio-Maxillo-Facial Surgery xxx (2014) 1e6
membrane or a platelet-rich-fibrin membrane
Increase in vertical bone height post-surgery.
Pre-operative bone height
The consistency of the putty helps minimize membrane per-
Post-operative bone height
forations and associated adverse events during percussion with
osteotomes. The technique also attempts to overcome the need to
*Highly statistically significant (p < 0.001).
purchase the specialized equipment required to apply hydraulic
pressure for the elevation of the schneiderian membrane, while
simultaneously placing an adequate volume of the graft material
in the site to allow for placement of the implants. Additional ad-
vantages of this technique are its atraumatic nature, reduced
The use of the minimally invasive antral membrane elevation
chair-side times, reduced overall treatment duration, improved
technique has a well-documented history of success in achieving
patient comfort and minimal graft wastage. The alloplastic
significant elevation of the sinus floor while sparing the need for
biomaterial utilized has been shown to exhibit timely resorption
more invasive direct sinus augmentation approaches
and subsequent replacement with new vital bone in histological
). Implant placement simultaneously
studies with residual graft fractions ranging from 4.3% to 11.5%,
with this technique is highly predictable and yields success rates
after 6 months of healing
ranging from 95.2% to 100% for 6e18 months of follow-up (
The prompt bone turnover rate observed with CPS putty
These results are compara-
may provide a clinical benefit in terms of primary and secondary
ble, yet slightly better than those reported in a large-scale survival
implant stability that increases its suitability in implant surgery
analysis of implants placed with the osteotome technique for in-
direct sinus lift (). When comparing these re-
Limitations of the technique proposed, are the necessary oper-
sults it should be noted that the latter study reports survival rates of
ator skill and experience needed for success, and the minimum
up to 12 years of function, which may partially explain the differ-
3 mm of available bone height needed for achieving primary sta-
ence in outcomes ().
bility for the implant. In one case where treatment was planned
Results from the work of Kfir et al. (), and Mazor
with the recommended technique and a baseline bone height of
et al. ) are also well within the range of 92.7e96.9%
2.5 mm, adequate primary stability was not attainable due to the
survival reported by a systematic review for sinus lift using the
poor bone quality of the site and thus treatment was performed in a
transalveolar approach In this review it
staged manner. Therefore, when considering the loosely packed
was concluded that implants placed in sites with remaining bone
medullary bone frequently encountered in the posterior maxilla,
height less than 5 mm have a reduced overall survival rate
the simplified minimally invasive antral membrane elevation
). Even though in most published cases, the
technique should be recommended for sites with at least 3 mm of
minimally invasive antral membrane elevation technique has been
residual bone height. The application of this technique should al-
utilized in cases with less than 5 mm of residual bone height,
ways be performed simultaneously with the placement of the
survival of implants placed with this technique is very high,
appropriate biomaterials in the osteotomy, as the use of a blood clot
reaching up to 100% for 18 months of follow-up ).
or platelet concentrates alone may lead to unpredictable results
The most significant benefit from the use of this technique is
(). On the other hand, bone substitutes such as
that it can achieve a gain in bone height comparable with that
freeze-dried allografts, xenografts and mineralized alloplastic
achieved with the use of the lateral window approach, while
substitutes have all shown to be efficacious in sinus augmentation
maintaining the advantage of the less invasive transalveolar
procedures with results comparable to those observed with par-
approach (The procedure is effective even in
ticulated or block grafts of autogenous bone (
highly resorbed residual ridges, as significant quantities of grafting
material can be rapidly introduced at the site with minimum risk of
). The use of bone morphogenetic protein 2 107
perforation. In general, the transalveolar sinus lift approach is
has also shown very promising results in sinus augmentation sur-
employed for sites with more than 6 mm of bone height pre-
gery and if the currently available information is supported by
operatively, while lateral window approaches are reserved for
longitudinal studies, their clinical use may surpass that of bone
cases with diminished baseline dimensions
substitutes ).
). The currently proposed technique extends the application
The presented technique may offer a more conservative proce-
of the transalveolar approach to cases with significantly less bone
dure with less postoperative morbidity, than the direct sinus
height (3e6 mm).
augmentation approach. This technique can be successfully used
In this prospective study, a simplified minimally invasive
for sinus augmentation with simultaneous implant placement, as it
transalveolar technique for sinus augmentation was utilized by
may offer increased primary stability to the implant due to the
exploiting the viscous consistency and flow characteristics of a new
viscous nature of the utilized bone graft. These advantages make
generation putty graft. The presented technique serves a dual
this simplified approach a viable option for transalveolar sinus
purpose: to minimize adverse events associated with the use of
augmentation. A possible limitation of the present study is the
osteotomes, and to provide an inexpensive technique for predict-
relatively short-term follow-up observed, with a minimum obser-
able elevation of the sinus membrane. A key determinant of success
vation time of 9 months when loading was considered the baseline
in the present study was careful case selection. On a patient level,
and 12 months when placement was set as the baseline. None-
only healthy individuals that were non-smokers were admitted to
theless, it is well established that the vast majority of early and
this study in order to avoid poor responders to treatment. On a site-
medium-term implant failures occur at the time of second stage
level, none of the cases had sinus septa in the selected implantation
surgery rather than manifesting as failure to maintain osseointe-
regions that may increase the risk of membrane perforation, or
gration post-loading ). Yet, controlled
technique failure. In such an unfortunate instance, a conventional
clinical studies are required to longitudinally assess the efficacy of
lateral-window sinus augmentation approach should be utilized to
this surgical improvisation in comparison to direct sinus augmen-
allow for increased visibility, isolation of the membrane perforation
tation approaches and to unequivocally prove the proposed supe-
and coverage of the perforation with an absorbable collagen
riority of the presented technique on patient-related outcomes.
Please cite this article in press as: Kher U, et al., A clinical and radiographic case series of implants placed with the simplified minimally invasive
antral membrane elevation technique in the posterior maxilla, Journal of Cranio-Maxillo-Facial Surgery (2014), http://dx.doi.org/10.1016/j.jcms.2014.08.005
YJCMS1862_proof ■ 6 September 2014 ■ 6/6
U. Kher et al. / Journal of Cranio-Maxillo-Facial Surgery xxx (2014) 1e6
Kfir E, Kfir V, Goldstein M, Mazor Z, Kaluski E: Minimally invasive subnasal eleva-
tion and antral membrane balloon elevation along with bone augmentation and
implants placement. J Oral Implantol 38: 365e376, 2012
The simplified minimally invasive antral membrane elevation
fir E, Kfir V, Kaluski E, Mazor Z, Goldstein M: Minimally invasive antral membrane
technique is based on the application of hydraulic pressure by a
balloon elevation for single-tooth implant placement. Quintessence Int 42:
viscous bone graft that acts as an incompressible fluid. Therefore,
simultaneously with the atraumatic elevation of the schneiderian
fir E, Kfir V, Mijiritsky E, Rafaeloff R, Kaluski E: Minimally invasive antral mem-
brane balloon elevation followed by maxillary bone augmentation and implant
membrane, grafting of the maxillary sinus is achieved resulting in
fixation. J Oral Implantol 32: 26e33, 2006
promotion of intrasinus bone formation, increased implant stability
Kher U, Mazor Z, Stanitsas P, Kotsakis GA: Implants placed simultaneously with
due to the viscoelastic nature of CPS putty, and a shorter operative
lateral window sinus augmentation using a putty alloplastic bone substitute forincreased primary implant stability: a retrospective study. Implant Dent 23:
time owing to the simultaneous elevation and grafting approach.
The proposed technique is a simple, efficacious, minimally invasive
Kotsakis G, Chrepa V, Marcou N, Prasad H, Hinrichs J: Flapless alveolar ridge
approach for sinus elevation that can be recommended for sites
preservation utilizing the ‘socket-plug' technique: clinical technique and review
of the literature. J Oral Implantol, 2012 (in press)
with at least 3 mm of residual height.
Kotsakis GA, Salama M, Chrepa V, Hinrichs JE, Gaillard P: A randomized, blinded,
controlled clinical study of particulate anorganic bovine bone mineral and
calcium phosphosilicate putty bone substitutes for socket preservation. Int J
flict of interest
Oral Maxillofac Implants 29: 141e151, 2014a
None of the authors has any conflicts of interest to this study.
Kotsakis GA, Joachim F, Saroff SA, Mahesh L, Prasad H, Rohrer M: Histomorpho-
metric evaluation of a calcium-phosphosilicate bone substitute in extraction
sockets. Int J Periodontics Restorative Dent 34: 233e239, 2014b
Mahesh L, Salama MA, Kurtzman GM, Joachim FP: Socket grafting with calcium
phosphosilicate alloplast putty: a histomorphometric evaluation. Compend
Acocella A, Bertolai R, Nissan J, Sacco R: Clinical, histological and histomorpho-
Contin Educ Dent 33: e109ee115, 2012
metrical study of maxillary sinus augmentation using cortico-cancellous fresh
Mazor Z, Ioannou A, Venkataraman N, Kotsakis G: A minimally invasive sinus
frozen bone chips. J Craniomaxillofac Surg 39(3): 192
augmentation technique using a novel bone graft delivery system. Int J Oral
Chaves MD, de Souza Nunes LS, de Oliveira RV, Holgado LA, Filho HN,
Implantol Clin Res 4: 78
Matsumoto MA, et al: Bovine hydroxyapatite (Bio-Oss®) induces osteocalcin,
Mazor Z, Kfir E, Lorean A, Mijiritsky E, Horowitz RA: Flapless approach to maxillary
sinus augmentation using minimally invasive antral membrane balloon eleva-
J Craniomaxillofac Surg 40(8): e315ee320, Dec 2012
tion. Implant Dent 20: 434e438, 2011
Cochran DL, Buser D, ten Bruggenkate CM, et al: The use of reduced healing times
Mazor Z, Peleg M, Gross M: Sinus augmentation for single-tooth replacement in the
on ITI implants with a sandblasted and acid-etched (SLA) surface: early results
posterior maxilla: a 3-year follow-up clinical report. Int J Oral Maxillofac Im-
from clinical trials on ITI SLA implants. Clin Oral Implants Res 13: 144e153,
plants 14: 55e60, 1999
Nickenig HJ, Wichmann M, Z€oller JE, Eitner S: 3-D based minimally invasive one-
Dahlin C, Johansson A: Iliac crest autogenous bone graft versus alloplastic graft and
stage lateral sinus elevation e a prospective randomized clinical pilot study
guided bone regeneration in the reconstruction of atrophic maxillae: a 5-year
with blinded assessment of postoperative visible facial soft tissue volume
retrospective study on cost-effectiveness and clinical outcome. Clin Implant
changes. J Craniomaxillofac Surg, 2014 (Epub ahead of print)
Dent Relat Res 13: 305e310, 2011
Nkenke E, Schlegel A, Schultze-Mosgau S, Neukam FW, Wiltfang J: The endoscop-
Del Fabbro M, Corbella S, Weinstein T, Ceresoli V, Taschieri S: Implant survival rates
ically controlled osteotome sinus floor elevation: a preliminary prospective
after osteotome-mediated maxillary sinus augmentation: a systematic review.
study. Int J Oral Maxillofac Implants 17: 557e566, 2002
Clin Implant Dent Relat Res 14(Suppl. 1): e159e168, 2012
Romero-Millan J, Martorell-Calatayud L, Penarrocha M, Garcia-Mira B: Indirect
Del Fabbro M, Testori T, Francetti L, Weinstein R: Systematic review of survival rates
osteotome maxillary sinus floor elevation: an update. J Oral Implantol 38(6):
for implants placed in the grafted maxillary sinus. Int J Periodontics Restorative
Dent 24: 565e577, 2004
Rothamel D, Wahl G, d'Hoedt B, Nentwig GH, Schwarz F, Becker J: Incidence and
Ding X, Zhu XH, Wang HM, Zhang XH: Effect of sinus membrane perforation on the
predictive factors for perforation of the maxillary antrum in operations to
survival of implants placed in combination with osteotome sinus floor eleva-
remove upper wisdom teeth: prospective multicentre study. Br J Oral Max-
tion. J Craniofac Surg 24(2): e102
illofac Surg 45(5): 387e391, Jul 2007
Engelke W, Deckwer I: Endoscopically controlled sinus floor augmentation. A
Sakka S, Krenkel C: Simultaneous maxillary sinus lifting and implant placement
preliminary report. Clin Oral Implants Res 8: 527e531, 1997
with autogenous parietal bone graft: outcome of 17 cases. J Craniomaxillofac
Ferrigno N, Laureti M, Fanali S: Dental implants placement in conjunction with
Surg 39(3): 187e191, Apr 2011
osteotome sinus floor elevation: a 12-year life-table analysis from a prospective
Sbordone C, Toti P, Guidetti F, Califano L, Pannone G, Sbordone L: Volumetric
study on 588 ITI implants. Clin Oral Implants Res 17: 194e205, 2006
changes after sinus augmentation using blocks of autogenous iliac bone or
Galindo-Moreno P, Avila G, Fernandez-Barbero JE, et al: Clinical and histologic
freeze-dried allogeneic bone. A non-randomized study. J Craniomaxillofac Surg
comparison of two different composite grafts for sinus augmentation: a pilot
42(2): 113e118, Mar 2014
clinical trial. Clin Oral Implants Res 19: 755e759, 2008
Scheuber S, Hicklin S, Bragger U: Implants versus short-span fixed bridges: survival,
Gassling V, Purcz N, Braesen JH, Will M, Gierloff M, Behrens E, et al: Comparison of
complications, patients' benefits. A systematic review on economic aspects. Clin
two different absorbable membranes for the coverage of lateral osteotomy sites
Oral Implants Res 23(Suppl. 6): 50e62, 2012
in maxillary sinus augmentation: a preliminary study. J Craniomaxillofac Surg
Summers RB: A new concept in maxillary implant surgery: the osteotome tech-
41(1): 76e82, Jan 2013
nique. Compendium 15(152): 54e56, 1994
Gutwald R, Haberstroh J, Stricker A, Rüther E, Otto F, Xavier SP, et al: Influence of
Sununliganon L, Peng L, Singhatanadgit W, Cheung LK: Osteogenic efficacy of bone
rhBMP-2 on bone formation and osseo integration in different implant systems
marrow concentrate in rabbit maxillary sinus grafting. J Craniomaxillofac Surg,
after sinus-floor elevation. An in vivo study on sheep. J Craniomaxillofac Surg
2014 (Epub ahead of print)
38(8): 571e579, Dec 2010
Triplett RG, Nevins M, Marx RE, Spagnoli DB, Oates TW, Moy PK, et al: Pivotal,
Hartlev J, Kohberg P, Ahlmann S, et al: Patient satisfaction and esthetic outcome
randomized, parallel evaluation of recombinant human bone morphogenetic
after immediate placement and provisionalization of single-tooth implants
protein-2/absorbable collagen sponge and autogenous bone graft for maxillary
involving a definitive individual abutment. Clin Oral Implants Res, 2013 (Epub
sinus floor augmentation. J Oral Maxillofac Surg 67(9): 1947e1960, Sep 2009
Vance GS, Greenwell H, Miller RL, et al: Comparison of an allograft in an experi-
Jeong SM, Lee CU, Son JS, Oh JH, Fang Y, Choi BH: Simultaneous sinus lift and
mental putty carrier and a bovine-derived xenograft used in ridge preservation:
a clinical and histologic study in humans. Int J Oral Maxillofac Implants 19:
J Craniomaxillofac Surg, 2014 (Epub ahead of print)
Kfir E, Goldstein M, Rafaelov R, et al: Minimally invasive antral membrane balloon
Wagenberg B, Froum SJ: A retrospective study of 1925 consecutively placed im-
elevation in the presence of antral septa: a report of 26 procedures. J Oral
mediate implants from 1988 to 2004. Int J Oral Maxillofac Implants 21(1):
Implantol 35: 257e267, 2009a
Kfir E, Goldstein M, Yerushalmi I, et al: Minimally invasive antral membrane balloon
Xuan F, Lee CU, Son JS, Jeong SM, Choi BH: A comparative study of the regenerative
elevation - results of a multicenter registry. Clin Implant Dent Relat Res
effect of sinus bone grafting with platelet-rich
fibrin-mixed Bio-Oss® and
11(Suppl. 1): e83ee91, 2009b
commercial fibrin-mixed Bio-Oss®: an experimental study. J Craniomaxillofac
Kfir E, Kfir V, Eliav E, Kaluski E: Minimally invasive antral membrane balloon
Surg 42(4): e47ee50, Jun 2014
elevation: report of 36 procedures. J Periodontol 78: 2032e2035, 2007
Please cite this article in press as: Kher U, et al., A clinical and radiographic case series of implants placed with the simplified minimally invasive
antral membrane elevation technique in the posterior maxilla, Journal of Cranio-Maxillo-Facial Surgery (2014), http://dx.doi.org/10.1016/j.jcms.2014.08.005
Source: http://imparteducation.in/downloads1/Udata/JCMFS%20Indirect%20lift.pdf
Hydroxyurea clinical practice guidelines - providers - first choice by select health of south carolina
Tips and guidelines for prescribing hydroxyurea. Clinical Practice Guidelines • 15mg/kg daily for adult patients with normal kidney function. • 5-10mg/kg daily for adult patients with creatinine clearance (CrCl) <60 mL/min. • 20mg/kg daily for infants (>9 months) and Baseline laboratory values • Complete blood count (CBC) with differential.
milne.ruc.dk
- I, OM OG MED MATEMATIK OG FYSIK I, OM OG MED MATEMA Semi-Mechanistic Pharmacokinetic and Pharmacodynamic Modelling of a Novel Human Recombinant Follicle Stimulating Hormone Trine Høyer Rose Roskilde University Department of Science and Environment nr. 502 - 2016 DK - 4000 Roskilde Roskilde University,