Multi-organ dysfunction secondary to severe wasp envenomation
Ittyachen et al. International Journal of Emergency Medicine (2015) 8:6 DOI 10.1186/s12245-015-0054-7 Multi-organ dysfunction secondary to severe waspenvenomation Abraham M Ittyachen*, Shanavas Abdulla, Rifzana Fathima Anwarsha and Bhavya S Kumar Wasp sting is not an uncommon incident. Around 56% to 94% of the population is stung at least once in theirlifetime by a member of the order Hymenoptera which includes wasps, bees, and ants. The response to a waspsting may vary from mild local reaction to severe systemic and anaphylactic reactions. The clinical picture andmortality rate tend to be more severe in adults compared to children. We present a 32-year-old agricultural workerwho was bitten by multiple wasps while on a coconut tree. In spite of the heavy load of venom due to the multiplebites, the patient did not develop anaphylaxis. However, a delayed reaction did occur within 48 h in the form ofsevere multi-organ dysfunction. There was significant improvement by around 2 weeks; but it took another 6 monthsfor the serum creatinine to normalize. This case highlights the occupational risk of Hymenoptera envenomation, thelife-threatening complications that may follow and which may even be delayed as was the case with this patient, andthe value of emergency care and intensive management which can result in a favorable clinical outcome.Keywords: Wasp sting; Allergy; Multi-organ dysfunction (exact species could not be identified) while climbing a Wasp sting is not an uncommon incident. Wasps together coconut tree. He had developed breathing difficulty and with bees and ants belong to the order Hymenoptera.
generalized swelling immediately after this incident. He Around 56% to 94% of the population is stung by a mem- was taken to a nearby hospital where he was treated in the ber of this order at least once in their lifetime . The re- emergency unit and send home the same day as he felt sponse to Hymenoptera stings are classified as normal ‘better'. The next day, he noticed a decrease in his urine local reactions, large local reactions, systemic anaphylactic output and progressive shortness of breath and hence was reactions, systemic toxic reactions, and unusual reactions referred to our hospital.
[. The most frequently observed are large local and This was a young male who was engaged in agricul- systemic anaphylactic reactions [. In children, around tural work. He had a history of bronchial asthma since 60% of systemic sting reactions are mild, whereas in childhood and used to take albuterol inhalers occasion- adults, systemic reactions tend to be severe in about 70% ally. There was no history of severe wheezing until now.
[. Also, the fatality rate is higher in elderly patients than He neither smoked nor took alcohol and also denied that in children and young adults . Herein, we present taking any illicit drugs.
a young male who had multi-organ dysfunction secondary At arrival in the ED, he was conscious and oriented. He to multiple wasp stings.
appeared jaundiced with multiple swellings predominantlyover the trunk, upper limbs, and head (these swellingslater developed mild ulcerations) (Figures and . There Case presentation was mild tachycardia (110 beats/min) and tachypnea A 32-year-old male presented to the emergency depart- (24 times/min). Oxygen saturation was 92% on room air, ment (ED) of our hospital with breathing difficulty and de- and blood pressure was recorded as 140/90 mm of Hg in creased urine output. One day prior to the arrival in our the right upper limb. The rest of systemic examination hospital, this patient had been bitten by multiple wasps was unremarkable.
Based on a clinical suspicion of multi-organ dysfunction, * Correspondence: Malankara Orthodox Syrian Church Medical College and Hospital, Ernakulam he was evaluated as such. His laboratory parameters were District, Kolenchery, Kerala State 682311, India 2015 Ittyachen et al.; licensee Springer. This is an Open Access article distributed under the terms of the Creative CommonsAttribution License which permits unrestricted use, distribution, and reproductionin any medium, provided the original work is properly credited.


Ittyachen et al. International Journal of Emergency Medicine (2015) 8:6
HIV were negative. Being an area endemic for leptospirosis,the same was also ruled out.
Patient was managed initially in the intensive care unit
(ICU). He received intravenous methylprednisolone andantihistamines (pheniramine maleate) for the first 24 h.
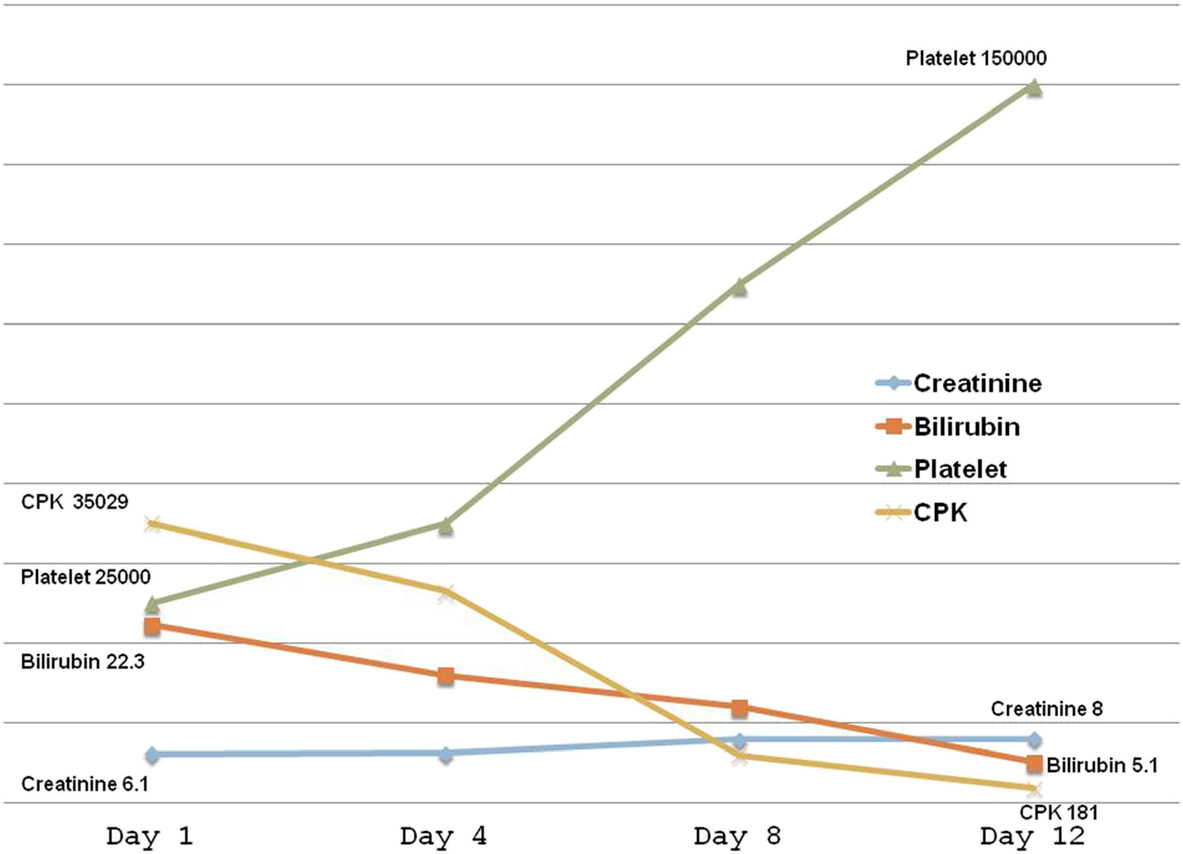
He continued to be anuric for the first 14 days and in allreceived 12 sessions of hemodialysis till the urine outputimproved and uremic symptoms subsided. He was alsotransfused 6 units of fresh frozen plasma (FFP) and 4units of platelet concentrate. The rest of the treatmentincluded intravenous fluids, prophylactic antibiotics, oxy-gen, and symptomatic measures. By about 2 weeks, his la-boratory parameters started improving (Figure . By the
Figure 1 Ulcerations over the scalp.
end of the third week, he was discharged successfully.
Though urine output had been established, it took an-
significant for severe renal failure, hemolysis, rhabdo-
other 6 months for his serum creatinine value to
myolysis, and liver dysfunction. His blood urea was
normalize. Throughout his hospital stay, the patient
126 mg/dL (N: 20 to 40 mg/dL) and serum creatinine
was hemodynamically stable and also did not require
was 6.1 mg/dL (N: 0.5 to 1.4 mg/dL). His liver enzymes
any assisted ventilation.
were also significantly raised: alanine transaminase (ALT)7128 IU/L (N: 5 to 35 IU/L) and aspartate transaminase
(AST) 13,985 IU/L (N: 8 to 40 IU/L). Coagulation parame-
Hymenoptera sting happens to be an occupational haz-
ters were mildly prolonged: prothrombin time 27.2 s (test)
ard in many parts of the world as was the case of this
and 11.3 s (control) and international normalized ratio
patient. The risk for systemic reaction is increased if pre-
(INR) 2.47. Though the patient had significant elevation in
ceded by a sting within the last 2 months even if the first
liver enzymes, he did not have any clinical features of liver
sting is well tolerated However, our patient did not
cell failure (hepatic encephalopathy). The disproportionate
reveal a prior history of envenomation despite the fact
rise in liver enzymes together with increased bilirubin
that he had an occupational risk. Though the risk for sys-
levels (total bilirubin 22.3 mg/dL N: 0.2 to 1.2 mg/dL) and
temic reaction is described to be greater in a bee venom-
a prolonged prothrombin time was presumably due to
sensitized patient compared with those sensitized to wasp
rhabdomyolysis and hemolysis/disseminated intravascu-
venom , our patient was an exception.
lar coagulation (DIC). A significant rise in the level of
The toxic compounds described in wasp venom are
lactate dehydrogenase (LDH) corroborated this finding
phospholipase A1, hyaluronidase, and antigen 5 [
(LDH: 76,100 IU/L N: 164 to 412 IU/L). Also, his hemogram
Other allergens include active peptides like melittin, amines
was deranged with the presence of anemia (hemoglobin:
like histamine and serotonin, and kinins, apamine, and
8 gm/dL) and thrombocytopenia (platelets: 25,000/mm3).
acetylcholine. Together, they are responsible for the myriad
His creatine phosphokinase (CPK) levels were also mark-
presentation of wasp sting. The more severe systemic
edly elevated - rhabdomyolysis (CPK: 35,029 IU/L N: 0 to
complications include renal (acute renal failure, nephrotic
225 IU/L). However, urine did not show any myoglobinuria.
syndrome, and renal tubular acidosis) cardiac
Viral markers for hepatitis B, hepatitis C, hepatitis A, and
(myocarditis, myocardial infarction, and arrhythmias), hepatic (centrilobular necrosis and pericholangitis), neurological (stroke, Guillian-Barre syndrome, andacute encephalopathy) hematological (hemolysis,DIC, and thrombocytopenia) [and vasculitis Our patient had several of these systemic reactions. How-ever, in spite of the heavy load of venom from the multiplebites, this patient did not develop the classic feature of se-vere anaphylaxis, specifically, anaphylactic shock.
For patients who have an occupational risk for insect
envenomation, immunotherapy may be a remedial meas-ure. However, the clinical effectiveness may be question-able not to mention the cost involved, especially forpoor communities. Monoclonal antibody as an adjuvant
Figure 2 Ulcerations over the upper limb.
to immunotherapy to increase the effectiveness of such
Ittyachen et al. International Journal of Emergency Medicine (2015) 8:6
Figure 3 Laboratory parameters. Note that all the parameters except creatinine had improved by about 2 weeks. It took another 6 months forthe creatinine to normalize.
therapy may be a future option but the issue of cost
Authors' information
still remains.
AMI is a professor of medicine and consultant intensivist at M.O.S.C MedicalCollege Hospital, Kolenchery, Ernakulam District, Kerala State, India. SA is anassistant professor of medicine in the same medical college. Both RFA and
BSK are residents in the medicine residency program in the same institution.
Although the management of any envenomation whether
Received: 13 October 2014 Accepted: 17 February 2015
it produces immediate anaphylaxis or late complicationsis challenging, the role of emergency care and intensivemanagement leading to a favorable outcome cannot be
Antonicelli L, Bilo MB, Bonifazi F. Epidemiology of Hymenoptera allergy.
Curr Opin Allergy Clin Immunol. 2002;2:341–6.
Emergency physicians should be aware of the risk of
Biló BM, Rueff F, Mosbech H, Bonifazi F, Oude-Elberink JN. Diagnosis of
hymenoptera envenomation in certain occupations and
Hymenoptera venom allergy. Allergy. 2005;60(11):1339–49.
the life-threatening complications that may follow and
Mueller UR. Clinical presentation and pathogenesis. In: Mueller UR, editor.
Insect sting allergy: clinical picture, diagnosis and treatment. Gustav Fischer
which may even be delayed as was the case with this
Verlag: Stuttgart; 1990. p. 33–65.
Lockey RF, Turkeltaub PC, Baird-Warren IA, Olive CA, Olive ES, Peppe BC,et al. The Hymenoptera venom study I, 1979–1982: demographics andhistory-sting data. J Allergy Clin Immunol. 1988;82:370–81.
Lantner R, Reisman RE. Clinical and immunologic features and subsequentcourse of patients with severe insect sting anaphylaxis. J Allergy Clin
Written informed consent was obtained from the patient
for publication of this case report and any accompanying
Annila IT, Karjalainen ES, Annila PA, Kuusisto PA. Bee and wasp sting reactions
in current beekeepers. Ann Allergy Asthma Immunol. 1996;77:423–7.
Pucci S, Antonicelli L, Bilo MB, Garritani MS, Bonifazi F. Shortness of intervalbetween two stings as risk factor for developing Hymenoptera venom
allergy. Allergy. 1994;49:894–6.
ED: Emergency department; ALT: Alanine transaminase; AST: Aspartate
Muller UR. Bee venom allergy in beekeepers and their family members.
transaminase; INR: International normalized ratio; DIC: Disseminated
Curr Opin Allergy Clin Immunol. 2005;5:343–7.
intravascular coagulation; LDH: Lactate dehydrogenase; CPK: Creatine
Hoffman DR, Jacobson RS. Allergens in Hymenoptera venom: XII how much
phosphokinase; HIV: Human immunodeficiency virus; ICU: Intensive care unit;
protein is in a sting? Ann Allergy. 1984;52:276–8.
FFP: Fresh frozen plasma.
King TP, Kochoumian L, Joslyn A. Wasp venom proteins: phospholipase A1and B. Arch Biochem Biophys. 1984;230:1–12.
Vikrant S, Pandey D, Machhan P, Gupta D, Kaushal SS, Grover N. Wasp
Competing interests
envenomation-induced acute renal failure: a report of three cases. Nephrology
The authors declare that they have no competing interests.
Chao YW, Yang AH, Ng YY, Yang WC. Acute interstitial nephritis and
Authors' contributions
pigmented tubulopathy in a patient after wasp stings. Am J Kidney Dis.
AMI conceived, researched, and drafted the manuscript. SA performed the
literature review and reviewed the manuscript. RFA and BSK reviewed the
Wagdi P, Mehan VK, Bürgi H, Salzmann C. Acute myocardial infarction
manuscript and obtained the relevant images. All authors read and approved
after wasp stings in a patient with normal coronary arteries. Am Heart J.
the final manuscript.
Ittyachen et al. International Journal of Emergency Medicine (2015) 8:6
Rowe SF, Greer KE, Hodge Jr RH. Electrocardiographic changes associatedwith multiple yellow jacket stings. South Med J. 1979;72(4):483–5.
Tsai CL, Fang CC, Chen WJ, Dierberg K. Hornet sting-induced toxic hepatitis.
Clin Toxicol (Phila). 2005;43(2):127–8.
Watemberg N, Weizman Z, Shahak E, Aviram M, Maor E. Fatal multipleorgan failure following massive hornet stings. J Toxicol Clin Toxicol.
1995;33(5):471–4.
Volders J, Smits M, Folkersma G, Tjan DH. An unusual neurologicalconsequence of massive wasp stings. BMJ Case Rep. 2012;28:2012.
doi:10.1136/bcr.01.2012.5555.
Sachdev A, Mahapatra M, D'Cruz S, Kumar A, Singh R, Lehl SS. Wasp stinginduced neurological manifestations. Neurol India. 2002;50(3):319–21.
Lombardini C, Helia RE, Boehlen F, Merlani P. "Heparinization" andhyperfibrinogenolysis by wasp sting. Am J Emerg Med. 2009;27(9):1176.e1–3.
doi:10.1016/j.ajem.2009.02.005.
Monzon C, Miles J. Hemolytic anemia following a wasp sting. J Pediatr.
1980;96(6):1039–40.
Krishna MT, Ewan PW, Diwalar L, Durham SR, Frew AJ, Leech SC, et al. BritishSociety for Allergy and Clinical Immunology: Diagnosis and management ofhymenoptera venom allergy: British Society for Allergy and ClinicalImmunology (BSACI) guidelines. Clin Exp Allergy. 2011;41(9):1201–20.
doi:10.1111/j.1365-2222.2011.03788.x.
Schoen EJ. Temporal arteritis after Hymenoptera sting. J Rheumatol.
1998;25(10):2040–2.
Ruëff F, Przybilla B, Biló MB, Müller U, Scheipl F, Seitz MJ, et al. Clinicaleffectiveness of hymenoptera venom immunotherapy: a prospectiveobservational multicenter study of the European Academy of Allergologyand Clinical Immunology Interest Group on Insect Venom Hypersensitivity.
PLoS One. 2013;8(5):e63233. doi:10.1371/journal.pone.0063233.
Palgan K, Bartuzi Z, Gotz-Zbikowska M. Treatment with a combination ofomalizumab and specific immunotherapy for severe anaphylaxis after awasp sting. Int J Immunopathol Pharmacol. 2014;27(1):109–12.
Submit your manuscript to a
journal and benefi t from:
7 Convenient online submission7 Rigorous peer review7 Immediate publication on acceptance7 Open access: articles freely available online7 High visibility within the fi eld7 Retaining the copyright to your article
Submit your next manuscript at 7 springeropen.com
Source: http://www.immediatecaretraining.ie/assets/Multi-organ_dysfunction_secondary_to_severe_wasp_envenomation.pdf
Microsoft word - 109094_01-qxr-medguide-1col-web.docx
MEDICATION GUIDE QUDEXY™ XR (cue-DEKS-ee ex-arr) Extended-Release Capsules Read this Medication Guide before you start taking QUDEXY XR and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment. If you have any questions about QUDEXY XR, talk to your healthcare provider or pharmacist.
19291_amgpro_kendler_mg_pi_lo2
For the treatment of postmenopausal women with osteoporosis at high risk for fracture Prolia® has been studied in patients who received prior alendronate therapy Patients Continuing on Alendronate Therapy or Transitioning to Prolia® Were Evaluated1 Weekly alendronate 70 mg and placebo SC Q6M All patients on alendronate Weekly oral placebo and denosumab 60 mg SC Q6M