Microsoft word - 4177447e-5e10-183ba3.doc

Guidelines for the Management of Asthma in California Schools
A comprehensive resource for school health and other personnel
to address asthma in the school setting
Arnold Schwarzenegger
Governor
State of California
Kimberly Belshé
Secretary
Director
California Health and Human
California Department of
Services Agency
Health Services
April 2004
Guidelines for the Management of Asthma in California Schools
Majel Arnold, R.R.T., M.S.-H.S.A.
Marilyn Ryan, R.N., B.S.N.
California Asthma Public Health Initiative
Los Angeles County Office of Education
California Department of Health Services
Los Angeles, California
Sacramento, California
Eileen Yamada, M.D., M.P.H.
Patricia L. Collier, R.N., M.A.
Maternal and Child Health Branch
Los Angeles County Office of Education
California Department of Health Services
Los Angeles, California
Sacramento, California
Linda Davis-Al dritt, R.N., M.A., P.H.N. California Department of Education Sacramento, California AnnMarie Duquette, R.N., M.S.N. Kern County Unified School District Bakersfield, California Marie Fortier, R.N., B.S.N. Solano County Office of Education Fairfield, California Anne Kelsey-Lamb, M.P.H. Regional Asthma Management and Prevention Initiative (RAMP) Oakland, California Patricia Michael, R.N., M.A., P.H.N. California Department of Education Sacramento, California David Núñez, M.D., M.P.H. California Asthma Public Health Initiative California Department of Health Services Sacramento, California Paul Qaqundah M.D., F.A.A.P., F.A.A.A.A.I. School Health Committee Orange County Chapter Huntington Beach, California Col een Richardson, C.A.E. California Thoracic Society Tustin, California
Ronald W. Chapman, M.D., M.P.H.
Howard Taras, M.D.
California Department of Health Services
Department of Pediatrics
Sacramento, California
University of California, San Diego
San Diego, California
STARBRIGHT Foundation
Kerry Van Frank R.N., B.S.N.
Los Angeles, California
Pasadena Community Asthma Project
Pasadena, California
Gordon Garcia, M.D.
Kaiser Permanente
Northern California Region
Community Action to Fight Asthma
Sacramento, California
Oakland, California
STARBRIGHT Foundation
Los Angeles, California
Ardis Hanson, R.N., B.S.N.
San Francisco Unified School District
San Francisco, California
Marie Hoemke, R.N.
San Francisco Unified School District
San Francisco, California
Beth Saiki, M.P.H.
American Lung Association
San Francisco, California
George Saunders, M.P.H.
Environmental Health Investigations Branch
California Department of Health Services
Oakland, California
Sidney Smith, M.D., F.A.A.P.
American Academy of Pediatrics
Southern California Region
Los Angeles, California
Barbara Spark
U.S. Environmental Protection Agency
Region IX
San Francisco, California
Guidelines for the Management of Asthma in California Schools
Table of Contents
Introduction. 7
B. Definitions .9
C. General
• Peak Flow Monitoring.14
• Metered Dose Inhalers (MDI) .16
• Mechanical Nebulizer.16
• Nurse Assessment Vital Signs Reference.17
• Environmental Protection Agency - Tools for Schools.18
Management of Asthma in California Schools: Guidelines for
Health Care Practice .19
• Access to Medications.19
• School Environmental Control.19
• Responsibilities of School Site Administrator .20
• Responsibilities of School Nurse.20
• Responsibilities of Teacher .23
• Responsibilities of Physical Education Instructor, Coach, and
Certified Athletic Trainer.24
E. Sample School Forms .25
• DHS Asthma Action Plan for Schools and Families .26
• Health Care Provider's Authorization Form and
Parent Consent for Management of Asthma in School and School
Sponsored Activities, including authorization for a student to carry
and self administer their medication .29
• Health Care Provider's Authorization Form and
Parent Consent for Management of Asthma in School and School
Sponsored Activities .31
• Management of Asthma at Home Interview Form: Information
for an Individualized School Health Care Plan .33
F. Health Care Procedures for Management of Asthma in Schools
• Asthma Episode Response Procedure.35
• Peak Flow Meter Procedure.36
• Metered Dose Inhaler Procedure .38
• Mechanical Nebulizer Procedure.40
G. Appendix
• California Education Code
Self Administration of Asthma Medication .44
• California Code of Regulations
Administering Medication to Pupils .45
• Sample Poster for School Emergency Response Procedure for
Severe Asthma Episode.51
• "Stepwise Approach for Managing Asthma in Adults and
Children Older than 5 Years of Age: Treatment" table .52
• Asthma Controllers and Asthma Relievers Medication
References .53
• How to Use a Metered Dose Inhaler (MDI): Student/Parent
Education Reference.55
• Open Mouth Technique Student/Parent Education Reference.57
• Closed Mouth Technique Student/Parent Education Reference .58
• Peak Flow Monitoring Student/Parent Education Reference.59
• "How Asthma-Friendly Is Your School?" Checklist.60
H. Resources .61
I. Bibliography.64
A. Introduction:
Asthma is a leading chronic illness for children and adolescents in the United States (Trends in Childhood Asthma: Prevalence, Health Care Utilization and Mortality, PEDIATRICS, August 2002). Recent California (2001 California Health Interview Survey) and national statistics (Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report, May 2, 2003) indicate:
• An estimated 13.7 percent to 16.3 percent of California children ages 6-17 have been
diagnosed with asthma (approximately one mil ion children);
• Approximately 75 percent of these children experienced asthma symptoms within the
last year and over 30 percent experienced monthly, weekly, or daily symptoms;
• Nationally, asthma accounts for an estimated 14 mil ion absences from school each
• Asthma is a major cause of emergency department visits and hospitalizations for
In 2001, nearly 136,000 California adolescents (ages 12-17) with asthma missed one or more days of school per month. This translates to at least $40.8 mil ion in lost revenue for the state's public schools (for absences attributable to preventable asthma exacerbations). Because students with asthma spend many hours at school participating in school activities, the school environment and staff play important roles in helping students manage their asthma. Students' lives and wel -being depend on the knowledge and correct response by school staff for assistance, if needed. Al school staff should have a basic understanding of asthma, be able to recognize signs and symptoms of an asthma episode, and know the appropriate action and response to initiate. School staff should also understand the importance of the prevention and control of asthma symptoms through environmental control measures. This includes assuring that common activities do not create an unsafe or unhealthy indoor environment. Proper monitoring and proper use of preventive medication and devices is also critical. Acute symptoms require prompt action to help students resume normal activities as soon as possible and/or to prevent an episode from becoming more serious or life-threatening. Each student should have an asthma action plan developed by his or her authorized health care provider. This plan will identify the status of the student's asthma control (asthma severity classification) and the need for student assistance and supervision. This plan can be used to identify specialized physical health care procedures needed in school, and to develop an Individualized School Health Care Plan (ISHP) for school accommodations (see Definitions, page 10). The role of school staff is to promote safe and healthy independent management by students with asthma for proper control of their chronic il ness and to provide assistance when students need additional help. Current standards of health care practice for the management of asthma wil impact the health care services needed by students at school and at al school related activities. Implementation of these standards wil require educated, responsible, and committed school staff to assist students with maintaining optimum management and control of their asthma. All students
have the basic right to an appropriate education, with access to the core curriculum, as facilitated by the provision of legal y required accommodations. This asthma module includes the fol owing information: •
Definitions of terminology used for understanding and treating asthma episodes.
Current general information about asthma and appropriate procedures to apply in the school environment.
School Management of Asthma: Guidelines for Health Care Practice: 1. Student access to medication. 2. School environmental control. 3. School staff responsibilities.
Sample school forms: 1. Authorization form for school personnel to assist the student in receiving his/her
2. Authorization form for a student who is able to self-carry his/her medication and
self-manage his/her medication.
3. Interview form used by the school nurse and completed with the parent and student
to obtain information to develop an Individualized School Health Care Plan.
Health care procedures used by the school nurse or public health nurse to train
designated school staff to perform as authorized.
The appendix contains: 1. California Education Code and California Code of Regulations information about self
administration of medication and administering medication to pupils in schools.
2. A sample poster for school emergency response procedure for severe asthma
3. "Stepwise Approach for Managing Asthma in Adults and Children Older than 5 Years
of Age: Treatment" table.
4. Current Asthma Control ers and Asthma Relievers medication name and photo
references (2003). This reference should be supplemented with additional information as new medications for asthma are approved for use in children.
5. Instructional resources for students and parents, including procedure descriptions for
how to use a metered dose inhaler (MDI), spacer, and peak flow meter.
6. "How Asthma-Friendly Is Your School?" checklist.
This information was developed to assist schools and school nurses in providing a safe, healthy environment, and to promote academic achievement, self-esteem, and future life success for al students with asthma. In addition, the Guidelines for the Management of Asthma in California Schools have been developed to reflect the current standards of health care practice and are recommended guidelines for inclusion in school district policies and procedures.
B. Definitions:
Asthma: Asthma is a chronic inflammatory disease of the airways in the lungs. This
airway inflammation contributes to recurrent acute episodes (attacks) of breathing
problems such as coughing, wheezing, chest tightness, or shortness of breath.
Asthma Action Plan: An action plan (or asthma management plan) is developed by the
authorized health care provider in partnership with the student and parent/guardian to
assist in the management of acute asthma episodes and in maintaining long-term control
of asthma. The plan may be based both on symptoms and peak flow measurements and
should be updated annually. The asthma action plan may be used to develop a student's
individualized school health care plan (ISHP), and may be attached to the ISHP or 504
plan. (See the sample DHS Asthma Action Plan for Schools and Families, pages 26-28.)
Asthma Severity Classification: The severity classification, determined by the health
care provider, combines subjective history (symptoms) and objective measures of lung
function (peak expiratory flow) to characterize the significance of the disease. The four
classes of severity are mild intermittent, mild persistent, moderate persistent, and
severe persistent. A classification of asthma based on severity is important for assessing
whether current medication therapy is sufficient and for determining the most effective
medication therapy. An individual's severity classification can change over time.
Individuals at any severity level can experience mild, moderate, or severe asthma attacks.
(See Stepwise Approach for Managing Asthma in Adults and Children Older Than Five
Years of Age: Treatment in Appendix, page 52.)
Epinephrine Pen (EpiPen): Epinephrine is an emergency injectable prescription
medication administered during a severe al ergic reaction called anaphylaxis. Anaphylaxis
is always treated as a medical emergency. Signs and symptoms may include flushing,
hives, faintness, loss of consciousness, severe difficulty breathing, and throat closing.
Anaphylaxis may occur following exposure to a variety of al ergens, including insect stings
and certain foods. Risk factors for anaphylaxis include food allergy, asthma, and prior
history of reactions. School personnel should identify children with a history of previous
anaphylaxis and establish an emergency plan for rapid treatment and medical attention.
Exercised Induced Bronchospasm (EIB) or Exercise Induced Asthma: Exercise may
be the only cause of asthma symptoms for some individuals. Exercise induced symptoms
should be anticipated in al students with asthma. EIB may also be a sign of inadequate
asthma management. Symptoms usually begin during exercise and peak five to ten
minutes after stopping exercise. As directed by the authorized health care provider, use of
quick-relief or certain long-term control medications before exercise may help reduce
exercise-induced symptoms and allow a child to participate ful y in exercise activities.
Influenza Vaccine: Parents should be advised that annual influenza vaccinations are
recommended for all children with asthma who do not have a history of severe al ergic
sensitivity to egg. Only the injectable, inactivated flu vaccine (not intranasal flu vaccine) is
recommended for children with asthma.
Individualized School Health Care Plan (ISHP): An ISHP is a nurse care plan for
managing health care services in school. A qualified school nurse develops the ISHP with
the parent, student, and physician (if appropriate). The ISHP uses the information from a
current health assessment to identify the health care needs of the student for school
attendance and to develop a plan for accommodations in school. The plan includes who
wil do what, when, where, and how; training, supervision and monitoring of designated
school staff; documentation of al information; an evaluation system for student outcomes
and changes; and, provides an accountability record for safe, consistent provision of
services to the student.
Long-term Control Medications: (See Asthma Controllers for names and photos of
different medications in Appendix, page 53.) These medications are taken daily on a long-
term basis to achieve and maintain control of persistent asthma. The goal of therapy is to
prevent asthma symptoms from occurring. Long-term control medication is recommended
for al three categories of persistent asthma. Since these medications can be administered
at home, most students do not need to take them while they are at school. These
medications do not provide quick relief of asthma symptoms. Examples of medications
that provide long-term control include:
Inhaled corticosteroids (Aerobid®, Azmacort®, Beclovent®, Flovent®, Pulmicort®,
long-acting
Beta2–agonists (Foradil®, Serevent®)
Combination inhaled corticosteroid/long-acting Beta2–agonists (Advair®)
Oral leukotriene modifiers (Accolate®, Singulair®)
Other medications: Theophylline, cromolyn (Intal®), and nedocromil (Tilade®)
Studies comparing inhaled corticosteroids to other control er medications are limited, but
available evidence shows that no long-term control medication appears to be as effective
as inhaled corticosteroids in improving asthma outcomes.
Mechanical Nebulizer: A small, portable machine used to deliver certain asthma
medications. The nebulizer is plugged into an electrical outlet or may be battery powered.
A nebulizer treatment usually takes 10-15 minutes to administer. Students requiring
regular nebulizer treatments may need to keep the nebulizer at school.
Metered Dose Inhaler (MDI): MDIs are the most common delivery devices for inhaled
medications. Appropriate technique is important to ensure adequate delivery of
medication to the airways. Use with a spacer/holding chamber is recommended. Open
mouth and closed mouth techniques may be used if a spacer is not available. Other types
of delivery devices that do not require a spacer include Dry Powder Inhalers (DPI) and
Breath Actuated MDIs.
Oral Corticosteroids (prednisone, methylprednisolone): Used for moderate to severe
asthma exacerbations to speed recovery and prevent relapse of exacerbations. These are
general y prescribed for once daily "burst" therapy lasting three to ten days. Frequent
courses of oral corticosteroids are an indication of poorly control ed asthma. Some
individuals with severe persistent asthma may require the long-term use of oral
corticosteroids.
Peak Flow Meter: A peak flow meter is a device that measures how well air moves out of
the lungs (peak expiratory flow [PEF]). When airflow is obstructed by asthma, the peak
flow meter provides an objective measure of the severity of the airway obstruction. The
peak flow meter may detect airway narrowing from asthma before noticeable symptoms
occur. Children over five years old are generally able to use these devices.
Pulse Oximeter: A portable electric pulse oximeter can measure the oxygen saturation in
an individual's bloodstream through an electronic sensor applied to the fingertip. The
normal oxygen saturation measurement in a healthy individual is 100 percent. An oxygen
saturation measurement below 92 percent is a medical alert value. While many individuals
experiencing asthma symptoms may have reduced oxygen saturation levels, a normal
oxygen saturation measurement does not exclude the possibility that an individual is
experiencing asthma symptoms.
Quick-Relief Medications: (See Asthma Relievers for names and photos of different
medications in Appendix, page 54.) Medications that give prompt relief of
bronchoconstriction and accompanying acute symptoms: coughing, wheezing, shortness
of breath, rapid breathing, and chest tightness. Short acting bronchodilators are the most
effective medication for relieving acute bronchospasm. Frequent use of quick relief
medications (greater than twice weekly in intermittent asthma; daily or increasing use in
persistent asthma) may indicate inadequate asthma control. If frequent use is noted, the
student's parent or guardian and health care provider should be advised to consider
initiating (or increasing) long-term asthma control medication. Al students with asthma
should have their quick relief medication available at school in case of unexpected
exposure to asthma triggers or an asthma episode.
Examples of quick relief medications include:
Albuterol
(Xopenex®)
(Alupent®)
Ipratroprium bromide (Atrovent®)
Terbutaline
Spacers/Holding Chambers: Spacers attach to the MDI and facilitate a more uniform
dose of medication delivery from the MDI to the lungs. The holding chamber al ows
medication to remain suspended as an aerosol and the one way valve opens only when an
inhalation occurs. Examples of spacers include Inspirease®, Aerochamber®, and
Aerochamber with Mask®.
Specialized Physical Health Care Services (SPHCS): These health care services are
prescribed by a physician, require medically related training, and are necessary in order
for the student to attend school. In California, any individual with exceptional needs who
requires SPHCS can be provided these services in compliance with California Education
Code (CEC) Section 49423.5 and California Code of Regulations (CCR) Section 3051.12.
Students may also qualify for these services under federal laws, the Americans with
Disabilities Act (ADA), and Section 504 of the Rehabilitation Act. Students with asthma
may qualify for these services in school depending on the severity of their condition and if
the condition adversely affects their educational performance.
Triggers: Triggers are factors that contribute to or cause an asthma episode in a particular
individual. Triggers may be allergens or irritants and include smoke, dust mites, pests,
mold, furry animals, odors, respiratory infections, changes in weather, and exercise.
Environmental control measures should be instituted that reduce exposure to factors
known to increase the student's asthma symptoms.
504 Plan: Section 504 of the Rehabilitation Act of 1973 (P.L. 93-112) is a federal civil
rights law that prohibits discrimination on the basis of disability in programs or activities
that receive federal financial assistance. Any student who meets the definition of a
qualified person with a disability, meaning one with a substantial physical or mental
impairment of a major life activity, a record of a disability, or is regarded as disabled by
others, may qualify for reasonable accommodations and modifications in school under this
federal law. With parental written permission, a multi-disciplinary team conducts an initial
evaluation. A 504 Accommodation Plan is developed and should include the nature of the
disability and what major life activity is limited, the basis for the disability determination, the
impact the disability has on education programs, and the required accommodations to
insure education with non disabled peers to the maximum extent possible in the Least
Restrictive Environment (LRE).
C. General Information
Background
The increase in the prevalence of asthma in children has resulted in a higher number of
students requiring health care assistance in school. Some schools in California have an
enrol ment of 50 to 100 students with diagnosed asthma. The health care requirements in
school for these students range from minimal assistance (for students with wel control ed
asthma who are self-managing their health care needs) to health care and emergency
assistance from trained school staff (for students with severe and frequent asthma episodes).
Children may experience severe and life-threatening asthma exacerbations separated by long
periods with apparently normal lung activity and without any obvious symptoms. Even children
with a history of mild intermittent asthma may experience a life-threatening asthma episode.
For children with poorly control ed asthma, symptoms can interfere with:
• School sport practices and events; • School performance and self-esteem; • School attendance; • School field trips; • Physical education; • Play activities; and • Playing brass or wind musical instruments.
However, children with wel control ed asthma can ful y participate in all of the above activities. Expected outcomes of care for children with asthma should be high because:
• Symptoms can be minimized or eliminated;
• The disease can be control ed; and
• Activity limitations should not be necessary.
Individualized School Health Care Plans The Individualized School Health Care Plan (ISHP) is a nurse care plan used to manage the health care needs of students. The school nurse is the only qualified school staff in the school system to develop an ISHP, train school staff in health care procedures, supervise procedure performance, and monitor and evaluate student outcomes. In the absence of a school nurse, a school can employ a public health nurse to develop an ISHP for a student with health care needs, train school staff in health care procedures, supervise procedure performance, and monitor and evaluate student outcomes. A licensed California physician and surgeon or authorized health care provider can also supervise school staff performance of health care procedures. Asthma education programs from local community agencies can be used to provide information to school staff (see Appendix for information resources regarding asthma education programs). Students with asthma who are compliant with their asthma action plan developed by their health care provider may not have asthma episodes that interfere with their educational
progress and may not need an ISHP in school. An ISHP should be developed in school for a student with severe and frequent asthma episodes that impact their education program and require health care and emergency assistance from trained school staff. The health care needed may be provided as Specialized Physical Health Care Services (SPHCS). Al students receiving SPHCS should have an ISHP. School policies and procedures should address provisions for students with asthma and criteria for determining when a student needs an ISHP and SPHCS. Peak Flow Meters
Peak flow meters are useful in the management of the student with asthma because these devices can detect decreased lung function and with early intervention a serious asthma flare may be avoided. Some children are poor perceivers of their asthma and may not recognize either subtle or dramatic signs or symptoms of poorly control ed asthma. Daily peak flow monitoring may be particularly useful in these children.
• Baseline data for the student must be obtained. The student's personal best peak flow
should be recorded so that comparisons can be made. Although predicted "normal" peak flow is determined by height, age, gender, and the type of meter used, it is preferable to monitor asthma control by the personal best reading. This is the highest measurement the child can achieve on a symptom free day.
• Peak expiratory flow (PEF) measurements are used by the authorized health care
provider to develop an asthma action plan for the child which may be used by the school nurse to evaluate the child's level of asthma control.
• PEF measurements may be used to determine the student's respiratory status by the
school nurse or trained, designated school staff.
• Peak flow meters are noninvasive assessment tools and do not require a health care
provider's authorization for use in school.
• Parents should be informed if a peak flow meter is used in school for their child and be
given the opportunity to decline the use with their child.
• If a peak flow meter is used for more than one student, each student must have his or
her own mouthpiece (or disposable) for each use. Each student should use the same type of peak flow meter in school as at home since the measured peak flow may vary between different types of meters. Peak flow meters should be cleaned regularly according to the manufacturer's instructions.
• See student/parent education resource on the use of peak flow meters in Appendix,
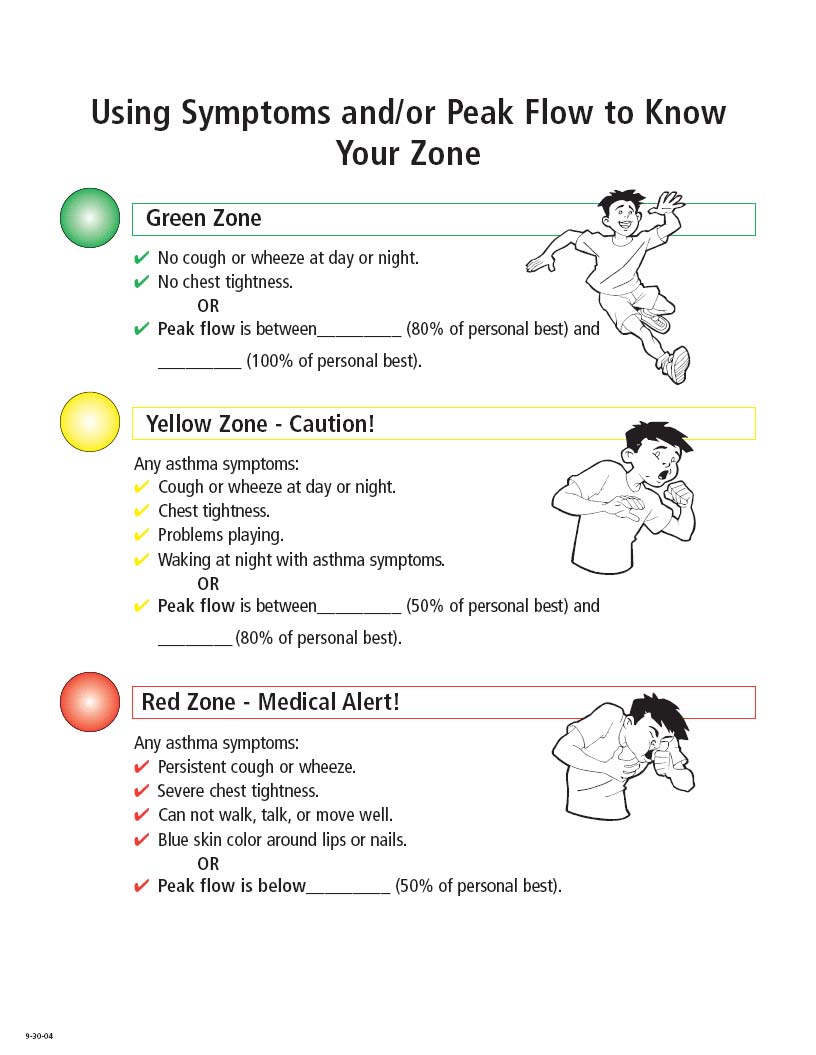
"Traffic Light" Zones for Asthma Management
Symptom and peak flow based asthma action plans are useful in assessing and managing asthma, and can be included in the ISHP (see the sample DHS Asthma Action Plan for Schools and Families, page 26). Most asthma action plans use a color/zone system. This system is useful in assessing asthma control both according to symptoms and/or peak flow measurements. The color zone indicates which medications should be given and how often and describes other procedures to perform.
Follow the authorized health care provider's individualized instructions for the child. The following are general recommendations for the three different color zones:
Green Zone
Indicates "relative stability"—Asthma is under good control
Children with wel control ed asthma should be maintained within 80 to 100 percent of their
best peak flow value and have minimal or no asthma symptoms.
Children may or may not require daily long-term control medication to remain in the green
zone. No change in asthma medications wil be needed at this level.
If the child experiences no asthma symptoms and peak flow measurements are
consistently greater than 80-90 percent of the personal best for several months, decreasing
the long-term control medications may be considered in consultation with the child's
guardian and health care provider.
Yellow Zone
Indicates "caution"—Asthma is not under control
Early signs or symptoms of an asthma attack are present (coughing or wheezing, difficulty
breathing, chest tightness, or pressure reported by the student). Peak flow measurements
wil decrease to between 50 to 80 percent of the expected personal best.
Prompt action is required to prevent an episode from becoming more serious. Prompt
administration of quick-relief medication is necessary as described in the ISHP or asthma
action plan. If appropriate changes in medication are made according to procedures in this
zone, the child's asthma should gradual y become stabilized again in the green zone.
The child's activity level should be adjusted to accommodate compromised lung function.
At the higher ranges of PEF in this zone, wheezing may not be noticeable with the use of a
stethoscope or the unaided ear. The lower ranges of this zone are usual y associated with
obvious clinical signs of asthma. This precrisis zone indicates extreme asthma instability
requiring immediate medical attention.
Indicates "medical alert—emergency!"—Severe asthma episode
Children in this zone may experience any of the symptoms in the yel ow zone and also may
have difficulty completing sentences and appear breathless, weak, or pale.
When PEF measurements fall at or below 50 percent of the personal best, the child faces
an almost certain asthma crisis.
Immediate and aggressive intervention is critical. Prompt administration of quick-relief
medication is necessary at frequent intervals as described in the ISHP or asthma action
plan. Close observation is required to assess the student's response to medication. The
child's parent or guardian should be notified of the child's condition.
The child must not be left unsupervised.
CALL 9-1-1 if child has:
•
Very fast or hard breathing
Skin sucking in over child's stomach or ribs with breathing
Breathing so hard they cannot walk or speak
Lips or fingernail beds turn blue
Metered Dose Inhaler (MDI):
• For students who carry their inhalers with them and self-manage their medication, an extra
quick-relief inhaler should be kept secure in the school health office in the event the student loses or forgets to bring their inhaler to school. These may also be needed for field trips and other off-site activities for students (health care providers can prescribe additional MDIs to families).
• Inhaler use must be monitored to know when the canister is empty. There is no reliable
method (e.g. floating the canister) for determining whether the MDI is ful or empty. Check with the pharmacist for the approximate date of the last dose in the container or fol ow manufacturer's instructions. The expiration date should also be identified on al inhaled medications.
• Frequent or daily use of quick-relief medications is often a sign of poorly control ed asthma.
Consultation with the child's parent and health care provider should be initiated to assess the severity of the child's asthma and to determine if asthma medications should be adjusted or if additional control er medications are necessary.
• See student/parent educational resources on the proper use of inhalers and spacers in
Appendix, pages 55-58.
Mechanical Nebulizer:
The mechanical nebulizer operates with either oxygen or compressed air to produce a stable
aerosol of fluid particles. Some long-term control medications and quick-relief medications
are available in liquid form for nebulization (Albuterol, Xoponex®, Pulmicort®).
• An ultrasonic nebulizer uses rapid vibration to convert liquid medication into ultra fine mist
aerosol particles that are then carried by a flow of compressed air or oxygen to the attached mouthpiece or mask.
• Manufacturer's instructions are used for the many different brands and models of
nebulizers; however, the standard procedure for treatment remains the same. The procedure for mechanical nebulizer is described in greater detail on pages 40-42.
• Mechanical nebulizers should be kept in a safe, clean, and secure location in schools and
made available for trained designated staff.
Nurse Assessment Reference:
Respiratory rate and heart rate normal ranges by age.
Age-Appropriate Vital Signs in Children
Normal Range of Resting Values
Respirations (/min)
60-100 122-132 128-140
Indicators of Hypoperfusion (poor blood flow)
• Tachycardia (fast heart rate) • Bradycardia (low heart rate—late sign) • Decreasing consciousness • Truncal pal or/cyanosis and coolness • Weak, thready, or absent peripheral pulses • Hypotension (low blood pressure—ominous sign)
Assessment of Level of Consciousness: AVPU Scale
A = Alert – Indicates the highest level of consciousness
The student will be awake and verbal or spontaneously interacts with the examiner and/or others who are
present.
V = Responds to verbal stimulus
The student may respond to a specific command or exhibit behavioral signs such as opening of the eyes,
quieting to a verbal command or loud voice.
P = Responds to painful stimulus
The student only responds to a painful stimulus. The student should withdraw from the stimulus.
Moaning or crying may also be elicited.
U = Unresponsive to any stimulus
The student shows no spontaneous responses and no responses to verbal or painful stimuli.
*Weight is approximate median of boys and girls combined, except for age 17
**Systolic blood pressure for the 90th – 95th height percentiles
Adapted from National Institutes of Health Clinical Center Website (www.cc.nih.gov/) and Pediatrics, v98, p654, 1996.
Information regarding the Management of Indoor Air Quality in the School Environment
Background Many indoor air quality problems in schools can impact the health of students and staff, including those with asthma. Some of the indoor air quality problems include: chemical pollutants from building or building maintenance materials; chemical pol utants form science and art classes; improperly maintained ventilation systems; and allergens from classroom animals and cockroaches or pests. Mold growth may result from standing water in maintenance rooms and near piping or from excess moisture in ceiling tiles, carpets, and other furnishings. Also, outdoor air pol utants and pollens may enter the school through ventilation systems and/or open doors and windows. In order to help improve indoor air quality problems in school buildings, the U.S. Environmental Protection Agency (EPA) developed the Indoor Air Quality (IAQ) Tools for Schools action kit. This kit helps school personnel identify, solve, and prevent indoor air quality problems in the school environment. Through the use of a 19-step management plan and checklists for the entire building, schools can also lower their students' and staff's risk of exposure to asthma triggers. The checklists cover the building's ventilation system, maintenance procedures, classrooms (especial y animals and mold), and food service areas. Contents of Action Kit Included in the kit is a Coordinator's Guide which explains the fundamentals of indoor air quality in schools and procedures for improving the air inside schools. The kit also contains checklists, a background informational piece for staff, a problem-solving wheel to identify potential indoor air quality causes and solutions, a guide for health care professionals, and a 30-minute, two-part video covering the ventilation checklist and a school's implementation of IAQ Tools for Schools. To use IAQ Tools for Schools, most schools form an IAQ coordinating team that implements the kit during the school year. Because IAQ problems can originate anywhere in the school building, usual y the entire staff is informed and brought into the process of improving the indoor air quality. In addition, students can be involved in the process. Information about available curricula on indoor air quality can be found at: http://www.epa.gov/iaq/schools/links.html School districts across the United States have adopted the principles of IAQ Tools for Schools, improving the indoor air quality in these districts' buildings. The IAQ Tools for Schools action kit can be used alone or in conjunction with the other school-based asthma curriculum for children. EPA has developed additional tools and programs to help schools and school districts implement IAQ Tools for Schools. This quick-start guide wil help you gain a valuable understanding of the IAQ Tools for Schools program and provide you with a brief review of the kit, helpful implementation ideas, and case studies of several schools that have successful y implemented the kit. Schools (or school districts) and nonprofit groups may receive a copy of the IAQ Tools for Schools action kit at no cost. Fax a request on school or company letterhead to IAQ INFO at 703-356-5386. For more information, cal IAQ INFO at 1-800-438-4318. The IAQ Tools for Schools action kit can also be downloaded at: http://www.epa.gov/iaq/schools/tools4s2.html.
D. Management of Asthma in California Schools: Guidelines for Health Care Practice
Access to Medications:
All schools should ensure that students with asthma have convenient and immediate access to their medications for al on- and off-site school sponsored activities before, during, and after school. These medications may prevent as wel as treat symptoms and enable the student to participate safely and vigorously in physical activities. Extra quick relief inhalers should be kept secured in the health office in the event the student loses or forgets to bring their inhaler with them. It may be necessary for students to carry and administer their own asthma medications. Effective January 1, 2005, any pupil may carry and self-administer inhaled asthma medication if the school district receives the appropriate written statements from both the pupil's physician and parent or guardian. Procedures for al owing students to carry and administer their own medications are outlined in CEC Section 49423.1 (see Appendix, pages 44). All medications to be administered to pupils at school must be in compliance with CEC Section 49423 and California Code of Regulations Title 5, Article 4.1, Section 600, Administering Medication to Pupils or Otherwise Assisting Pupils in the Administration of Medication During the Regular School Day (see Appendix, pages 45-50). Specialized Physical Health Care Services including the use of special medical equipment needed at school must follow CEC Section 49423.5 and CCR Title 5, Section 30051.12 for health care provisions in school. School Environmental Control:
All schools should cooperate in eliminating, decreasing, or control ing environmental risk factors that can exacerbate asthma. Implementation of programs such as the EPA IAQ Tools for Schools program, are useful in assisting schools to control environmental factors and IAQ. A healthy environment is necessary for keeping students healthy and preventing asthma symptoms. A healthy environment begins with proper maintenance of the building structure and its mechanical support systems. Basic cleanliness and dust control is very important to the control of asthma. Special attention and reasonable accommodation in school should be provided to students to decrease their exposure to their particular asthma triggers. Examples of triggers are listed in the table below:
INDOOR AND OUTDOOR AIR
OTHER TRIGGERS
Strong odors or fumes
Respiratory infections
Second hand smoke
Animal fur or feathers
Particulate matter
Medications (including
Car and bus exhaust Wheat
aspirin, ibuprofen, and
Cleaning products
Change of weather
In addition, school district policies and procedures should be developed to respond to local health advisories that are issued for high ozone days and poor outdoor air quality (see Best Practices for Communicating Air Quality and Related Health Information, Resources, page 62).
Responsibilities of School Site Administrator: Ensure the delivery of annual training to al school staff focused on providing a basic understanding of asthma. This includes information regarding the most common asthma triggers found in the school environment and the importance of reducing or removing these triggers, awareness of asthma signs and symptoms, and knowledge of the appropriate action or response to initiate when assistance is required.
The most important rules for staff to follow during an asthma episode:
NEVER LEAVE A STUDENT WITH BREATHING PROBLEMS ALONE.
DO NOT SEND A STUDENT WITH BREATHING PROBLEMS ANYWHERE.
GET HELP AND HAVE MEDICATION BROUGHT TO THE STUDENT.
Ensure that students with asthma have convenient and immediate access to their medication for al on- and off-site school sponsored activities before, during, and after school. Ensure that students with asthma have necessary accommodations in school and all procedures for assistance are provided by trained, designated staff and supervised by a qualified licensed health care professional. Ensure a clean and healthy environment with common sense indoor air quality principles and practices. Refer to the EPA's, Indoor Air Quality Tools for Schools (see Reference section). Ensure that common activities do not create an unsafe or unhealthy indoor environment. Ensure building maintenance, whenever possible, is scheduled during long weekends or vacations to avoid exposing students with asthma to fumes, dust, and other irritants. Curtail outdoor physical activities when local health advisories are issued for high ozone and poor air quality days. Ensure that information regarding health advisories for high ozone and poor air quality days are communicated to school personnel. Ensure that an emergency protocol for the management of asthma episodes for students is accessible to appropriate school personnel. Ensure inclusion and provision for accommodations in the school disaster plan for students receiving Specialized Physical Health Care Services (CEC Sections 35294-35297).
Responsibilities of School Nurse:
Determine when a student with asthma needs an ISHP. An interview with the parent and student wil validate the student's status regarding asthma control and/or accommodations needed in school. When accommodations are routine, the student is compliant with their asthma action plan, and does not have frequent asthma episodes, an ISHP may not be necessary. Availability and administration of medication may be al that is necessary for accommodation. Document the frequency of accommodations needed by students with asthma episodes to provide a record for evaluation and determination of when an ISHP is needed. It is
recommended that a copy of the student's asthma action plan be provided to the school whether or not a student has an ISHP. This plan can be used by the school nurse to evaluate a student's compliance if an asthma episode occurs. Al schools should establish standard asthma episode response procedures available for al school staff. Develop an ISHP when necessary, with the parent/guardian and student (if appropriate), including information from the authorized health care provider's asthma action plan and the health care provider's authorization and parent consent form for schools (see pages 26-33 for different sample form options to address these documentation needs, including the DHS Asthma Action Plan for Schools and Families). The ISHP is the student's school management plan for safe and healthy management of asthma in school and al school sponsored activities. It is developed for students with poorly control ed asthma that may interfere with their academic achievement and physical wel -being. 1. The student's ISHP includes information from a current health assessment by the school
nurse. The current health assessment includes:
• Current health status of student.
• Specific triggers that exacerbate the student's asthma.
• Health care procedures and emergency procedures needed in school and for al school
sponsored activities to accommodate the student's signs and symptoms of asthma wherever and whenever they might occur. This includes disaster preparedness.
• Information on medication, dosage, and time. Al medication administered in school
should comply with CEC Section 49423.
• Level of health care staffing needed in school as determined by school nurse. • Accommodation and modification of the student's active participation in physical
activities to match current asthma status for school related activities.
2. The ISHP includes:
• Health care procedures needed in school. • Identification of who wil do what, when, where, and how to accommodate the needs of
the student in school.
• Accommodations and modifications of the student's active participation in physical
activities to match current asthma status for school related activities.
• Identification of training, supervision, and monitoring of designated school staff
performing procedures.
• An evaluation system for student outcomes and changes.
• Is available to appropriate school personnel for all on- and off-site activities. • Can be included in the classroom teacher substitute book. • Can be used as a 504 Accommodation Plan and for an Individual Education Plan (IEP).
• Is reviewed yearly and/or whenever changes occur. • Is approved with written consent by the parent/guardian and school nurse. A copy of
this plan may be sent to the authorized health care provider, if requested, with parent/guardian written consent.
Monitor and evaluate outcomes of the ISHP and communicate with parent and authorized health care provider when changes and/or modifications are needed. Maintain linkages between school, family, and authorized health care provider to ensure coordinated care. Train and supervise al designated staff providing health care services to students with asthma in school. All training and supervision of designated staff by the school nurse must be in compliance with CEC Section 49423.5 and CCR, Title 5, Section 30051.12 for health care provision in school. The school nurse may partner with community and health care organizations and agencies as resources for assistance. Monitor students who are self-carrying and self-administering medication for managing asthma episodes. Students may be allowed to carry their inhaled asthma medications and use in school and al school sponsored activities, as prescribed by their authorized health care provider and in accordance with CEC Section 49423.1 (effective January 1, 2005). Assessing a student's ability to self- carry and self-administer asthma medications should include:
• The determination of the student's capability to have in his/her possession al necessary
equipment and medication.
• The determination of the student's capability for adherence to standard precautions and
appropriate handling of equipment and medication.
• The determination of the student's capability to maintain safety and privacy. • The development of an ISHP by the school nurse if the student's health condition and
status require monitoring and supervision.
The development of a written agreement with the student to include: 1. Reporting to designated school staff problems with medication, supplies, or equipment
and/or/when the student needs help.
2. Monitoring system for tracking student outcomes with self-administration of asthma
3. A clear understanding by the student of responsible behavior and that any act of
inappropriate behavior with regard to his/her self-administration of medication, such as sharing medications with peers, can result in the school administrator revoking the privilege of self-administration. Parent/guardian must be notified immediately if this should occur.
Inform the parents/guardians and authorized health care provider of acute asthma episodes occurring at school and discuss possible modifications in the student's asthma action plan and ISHP. Coach, counsel, encourage, and support each student's efforts to fol ow their asthma action
plan and develop a shared understanding about the conditions that require temporary activity modifications or medications. The school nurse can also intervene for temporary adjustments and modifications in physical activities in school. Assist the administrator in providing and/or planning general training to al staff regarding asthma and the appropriate responses when asthma episodes occur. The school nurse is the qualified school staff to provide this training and may partner with health care and environmental organizations for assistance within the community, if available. Train, educate, and support al school staff in problem solving and managing unpredictable occurrences of asthma episodes as wel as understanding new medical developments for treatment and control of asthma. Partner with community agencies, when available, for assistance with education programs and materials. Ensure that students with asthma have an emergency protocol for the management of asthma episodes.
Responsibilities of Teacher:
Know the early warning signs of an asthma episode for the students with asthma in their classroom and how to intervene. Know what the individual asthma triggers are for each student with asthma in their classroom and cooperate in reducing or removing environmental triggers found in classrooms such as animal fur, feathers, dust, perfume, etc., that may cause an asthma episode. Keep a current copy of the student's ISHP in the classroom, review it periodical y with the student and school nurse and know what steps to take in case of an asthma episode. Each student may have different medications and action plans as wel as different environmental factors that cause an episode. Prevention and quick appropriate response can avert a more serious episode. Understand that a student with asthma may feel:
• Drowsy, tired, or agitated when experiencing asthma symptoms.
• Withdrawn or different from the other students.
• Anxious about access to their asthma medication.
• Embarrassed about any disruption to usual school activities.
Educate classmates to understand asthma to enable students with asthma to feel more comfortable and less self-conscious. The school nurse can assist in providing information and educational programs using community agency resources. Review with the school nurse the possible side effects of asthma medications and how they may impact the student's performance in the classroom. Recognize that students with poorly control ed asthma may have excessive school absences. Develop a plan with the student and parent for handling missed schoolwork. Time lost from
school may negatively affect grades, academic achievement, self-esteem, and future life successes. Concerns should be referred to the school nurse, parent, and administrator. Be aware of health advisories issued for high ozone and poor air quality days.
Responsibilities of Physical Education Instructors, Coaches, and Certified Athletic Trainers:
Maintain a copy of and abide by the student's ISHP and understand what to do if an asthma episode occurs during exercise. Handle an episode quickly and appropriately, with tact and respect for privacy to avert a more serious episode. Abide by accommodations and modifications required in a student's 504 Plan or IEP. These are documents that provide parents and students with procedural safeguard rights. Accommodations/modifications should never influence, in a negative manner, the grade a student receives. Allow students to take their medication wherever they are and whenever they need it. This includes the use of any/al equipment devices such as inhalers, nebulizers, and peak flow meters. Medications taken before exertion may help avoid an episode. Preventive medicine enables most students with exercise-induced asthma to participate in any sport. Refer questions about a student's use of asthma medications to the school nurse. Encourage physical activity and participation in sports for students with asthma, understanding that physical activity can cause asthma symptoms for many students with asthma and the need to respect a student's limits. Be aware of environmental triggers; for example, exercising in cold, dry air and activities that require extended running exacerbate asthma more readily than other forms of physical activity. These activities must be done only as tolerated by the student. Curtail outdoor physical activities as appropriate for students with asthma when health advisories are issued for days when high ozone levels or poor air quality have been forecasted. Understand that warm-up and cool-down activities, appropriate for any exercise, may also be helpful for some students with asthma. Short periods of exercise fol owed by short rest periods may be better than continuous exercise. Exercise can cause asthma symptoms for many students. It is important to know that a child should not exercise when they are experiencing or recovering from an asthma episode. Refer questions about a student's ability to ful y participate in physical education to the school nurse and parent. Parent consent must be obtained for accommodations and modifications. The school nurse can assist with monitoring and evaluating the student's episodes during physical activities and give guidance and recommendations for adjusting activities to the parent and authorized health care provider. The school nurse can also consult with the authorized health care provider and parent for consents and authorizations for medication and schedule adjustments.
E. Sample School Forms
Health Care Provider's Authorization and Parent Consent for Management of
Asthma in School and School Sponsored Activities
First Name:
Last Name:
Completed by authorized health care provider:
7. Monitoring at school by symptoms only.
1. Control medication to be taken at school:
Symptoms:
Medication name: _
By peak flow meter and symptoms
Best peak flow is:
Medication name: _
Peak flow meter used:
2. Quick relief medication when symptoms occur at
8. Factors that cause an asthma episode:
Respiratory infection
Medication name: _
Strong odors or fumes
Medication name: _
Animal fur or feathers
Change of weather
3. Preventive medication before exertion or exercises at
9. Al ergies: _
Medication name: _
Spacer with mask used
Open mouth technique
4. Possible medication side effects at school:
5. Physician Asthma Action Plan Attached: Yes No 6.
Mechanical Nebulizer: Mask Mouthpiece Spacer Open mouth technique
Nebulizer Medication: _
Health Care Provider's Authorization for Management of Asthma in School
My signature below provides authorization for the above written orders. I understand that all procedures will be implemented in accordance with state laws and regulations. I understand that specialized physical health care services may be performed by unlicensed designated school personnel under the training and supervision provided by the school nurse. This authorization is for a maximum of one year. If changes are indicated, I will provide new written authorization.
I have instructed the above named student in the proper way to use his/her medications. It is my professional opinion
that they should be allowed to carry and use that medication by him/herself.
I request that the school nurse provide me with a copy of the completed Individualized School Health Care Plan.
Authorized Health Care Provider Name: Signature
Date Phone _ Address _ City Zip
Parent Consent for Management of Asthma in School
I (we) the undersigned, the parent(s)/guardian(s) of the above named student, request that the above authorization for specialized physical health care service for management of asthma in school be administered to my (our) child in accordance with state laws and regulations. I (we) will: 1. Provide the necessary supplies and equipment. 2. Notify the school's nurse if there is a change in student health status or attending authorized health care provider. 3. Notify the school nurse immediately and provide new consent for any changes in authorized health care provider's
I (we) give consent for the school nurse to communicate with the authorized health care provider when necessary.
I (we) understand that I (we) will be provided a copy of my (our) child's completed Individual School Health Care Plan.
Parent(s)/Guardian(s) Signature
_Date _
_Date _
Date Reviewed by School Nurse (Signature) Date Reviewed by Principal (Signature) _
Health Care Provider's Authorization and Parent Consent for Management of
Asthma in School and School Sponsored Activities
First Name:
Last Name:
Completed by authorized health care provider:
7. Monitoring at school by symptoms only.
1. Control medication to be taken at school:
Symptoms:
Medication name: _
By peak flow meter and symptoms
Best peak flow is:
Medication name: _
Peak flow meter used:
2. Quick-relief medication when symptoms occur at
8. Factors that cause an asthma episode:
Medication name: _
Respiratory infection
Strong odors or fumes
Medication name: _
Animal fur or feathers
Change of weather
3. Preventive medication before exertion or exercises at
Medication name: _
Spacer with mask used
Open mouth technique
4. Possible medication side effects at school:
5. Physician asthma action plan attached: Yes No 6.
Mechanical Nebulizer: Mask Mouthpiece
Spacer Open mouth technique
Nebulizer Medication: _
Health Care Provider's Authorization for Management of Asthma in School and School Sponsored Activities
My signature below provides authorization for the above written orders. I understand that all procedures will be implemented in accordance with state laws and regulations. I understand that specialized physical health care services may be performed by unlicensed designated school personnel under the training and supervision provided by the school nurse. This authorization is for a maximum of one year. If changes are indicated, I will provide new written authorization.
I request that the school nurse provide me with a copy of the completed Individualized School Health Care Plan.
Authorized Health Care Provider Name:
Signature _
Date Phone _ Address _ City _ Zip _
Parent Consent for Management of Asthma in School
I (we) the undersigned, the parent(s)/guardian(s) of the above named student, request that the above authorization for specialized physical health care services for management of asthma in school be administered to my (our) child in accordance with state laws and regulations. I (we) will: 1. Provide the necessary supplies and equipment. 2. Notify the schools nurse if there is a change in student health status or attending authorized health care provider. 3. Notify the school nurse immediately and provide new consent for any changes in authorized health care provider's
I (we) give consent for the school nurse to communicate with the authorized health care provider when necessary.
I (we) understand that I (we) will be provided a copy of my (our) child's completed Individual School Health Care Plan.
Parent(s)/Guardian(s) Signature
_Date
_Date
Date Reviewed by School Nurse (Signature) _ Date Reviewed by Principal (Signature) _
Management of Asthma at Home
Sample Interview Form
(Completed By School Nurse with Parent and Student)
Identify what may cause an asthma episode. Check each that applies to the student.
Respiratory infection
Animal fur or feathers
Change of weather
Strong odors or fumes
Child carries medication with them at all times and independently self-administers.
Child needs assistance with medication administration.
List any environmental control measures, medications, and/or dietary restrictions that the student needs to prevent an asthma episode. Personal best peak flow number:
Type of peak flow meter:
Daily medication used at home:
Name Amount Route/Method
Steps taken at home during an asthma episode:
1. Medications given: _ 2. Response time: 3. Other interventions: 4. When 9-1-1 is called at home: _ Date of last 9-1-1 call:
Emergency asthma medications used at home:
Route/Method When used
Field trips:
Special Precautions: _
Disaster preparedness at school:
_
_
9-1-1 WILL BE CALLED ACCORDING TO STANDARD SCHOOL EMERGENCY
F. Health Care Procedures for the Management of Asthma in Schools
Asthma Episode Response Procedure
To provide assistance to a student experiencing moderate symptoms of wheezing,
coughing, shortness of breath, chest tightness, or breathing difficulty.
Equipment and Supplies
1. Prescribed medication.
2. All equipment and supplies necessary for administering medication.
Procedure
1. Determine if the student is displaying symptoms such as wheezing, coughing,
shortness of breath, chest tightness, or difficulty breathing.
Key Points and Precautions:
As the airway becomes inflamed, swollen, or narrowed, breathing becomes difficult.
2. Stay calm, calm student, speak softly, and stay with student. Cal for help if needed.
Key Points and Precautions:
Difficulty with breathing creates anxiety. Reassuring the student wil reduce
anxiousness.
3. Encourage student to take slow, deep breaths. Seat student comfortably. Do not
allow student to lie down or go to sleep.
Key Points and Precautions:
Expansion of the lung and movement of the diaphragm are greatest in this position.
4. Give asthma quick-relief medication (e.g., Albuterol inhaler or Albuterol nebulizer
treatment) as authorized in student's ISHP.
Key Points and Precautions:
Asthma quick-relief medication should relax and open airway to improve breathing.
5. Stay with student and observe for improvement.
Key Points and Precautions:
Quick-relief asthma medication will general y provide improvement.
6. Follow ISHP directions for when to al ow student to return to class or resume school
activities.
Key Points and Precautions:
Response time from medication may vary.
7. If no improvement in five minutes after medication administration, and student has:
• Very fast or hard breathing
• Skin sucking in over child's stomach or ribs with breathing
• Breathing so hard they cannot walk or speak
• Lips or fingernail beds turn blue
Cal for help. Call 9-1-1. Repeat quick-relief medication every 20 minutes or as
authorized in student's ISHP. Stay with the student and be prepared to do CPR.
Key Points and Precautions:
Student may have a respiratory infection or more severe exacerbation.
8. Provide emergency response team with steps taken and medication given.
Log al information.
Peak Flow Meter Procedure
1. To improve the ability to document the onset of and to assess the severity of asthma
2. To detect the small changes in airflow that occur at the start of an asthma attack.
3. To identify exercise-induced asthma.
4. To monitor the need for, or the response to, prescribed medication.
5. Measures peak expiratory flow (PEF).
Equipment and Supplies
1. Peak flow meter (various brands are available.) Student should use the same type of
flow meter as used at home.
2. Mouthpiece (plastic or disposable).
Procedure
1. Determine the need for the student to use the peak flow meter at school by reviewing
ISHP.
Key Points and Precautions:
Some students with asthma may not wheeze even though they are in acute distress.
They may not be moving enough air through the airways to cause audible wheezing.
Key Points and Precautions:
Clean procedure.
3. Place the mouthpiece on the peak flow meter.
Key Points and Precautions:
Make sure that the pointer is on zero.
4. Have the student stand up.
Key Points and Precautions:
Be sure there is no candy or gum in the student's mouth.
5. Have the student hold the meter without obstructing the outflow vent. Fingers must
not obstruct the vent.
Key Points and Precautions:
Blocking the outflow wil result in an erroneous high PEF reading. Hold the body of
the meter cylinder paral el to the floor.
6. The student must inhale as deeply as possible.
Key Points and Precautions:
Poor inspiration may produce a false low PEF reading.
7. Have the student place the mouthpiece on the tongue with lips around the outside of
the mouthpiece.
Key Points and Precautions:
Be sure that lips form a tight seal.
8. The student must blow out as hard and as fast as possible into the mouthpiece.
Key Points and Precautions:
The student's exhaling will cause the marker to move up the meter. Note and record
the measurement that registers on the meter.
9. Replace the marker at zero. Repeat the procedure two more times for a total of three
exhalations.
Key Points and Precautions:
Wait 15 seconds between each try. Do not record measurement if technique is not
adequate.
10. Record the best PEF measurement. Compare this reading with the personal best
PEF documented in the student's ISHP.
Key Points and Precautions:
Write PEF measurements on a piece of paper and record best measurement on the
log.
11. If PEF measurement is in the green zone, no change in medications is required. If
student has asthma symptoms consistent with the yel ow zone, fol ow instructions for
yellow zone.
Key Points and Precautions:
Give medicine as authorized and monitor for results. The student should be
breathing easier, able to cough and clear secretions, and resume usual activity.
12. If measurement is in the yel ow zone, administer asthma quick-relief medication and
control medication according to student's ISHP.
Key Points and Precautions:
Yel ow indicates trouble. Give medicine as authorized, monitor closely, and cal
school nurse with PEF reading. Notify parent.
13. If measurement is in the red zone, administer asthma quick-relief medication and
control medication according to student's ISHP.
Key Points and Precautions:
Get Help. Call 9-1-1. Notify school nurse and parent. Stay with student. Keep
student in sitting position and keep student calm. Be prepared to do CPR.
14. Record the findings and actions of procedure on the student's SPHCS log.
Key Points and Precautions:
Notify school nurse and parent of unusual findings and actions.
15. Refer to the manufacturer's guide for cleaning and maintenance of the peak flow
meter.
Key Points and Precautions:
Wear gloves for cleaning. Remove gloves and wash hands.
Metered Dose Inhaler Procedure with Holding Chamber/Spacer
Equipment and Supplies
1. Prescription inhaler medication with metered dose inhaler. For dry powder, disk, and
breath actuated inhalers see manufacturer's instructions.
2. Holding chamber/spacer recommended for use with metered dose inhaler. Please
note: some metered dose inhalers are equipped with a spacer. Check
manufacturer's instructions.
Purpose:
To provide quick relief or prevent asthma symptoms or episodes by administering asthma
medication directly into the lungs. For metered dose inhalers, holding chambers/spacers
facilitate a more uniform dose of medication delivery to the lungs. To prevent exercise
induced symptoms, students may use their quick-relief inhaler before exercising as
authorized by their authorizing health care provider.
Procedure
1. Determine the need for student to use an inhaler at school.
Key Points and Precautions:
Review authorized health care provider's order and student's ISHP.
Key Points and Precautions:
Clean procedure.
3. Shake the metered dose inhaler wel ten times. Dry power/disk inhalers do not
require shaking.
Key Points and Precautions:
The right amount of medication may not spray out if the inhaler is not shaken wel .
4. Attach the inhaler to the holding chamber/spacer, if necessary.
Key Points and Precautions:
To deliver the medication directly to the lungs, the technique with the inhaler must be
correct. If the inhaler cannot be used correctly, the student's authorized health care
provider should be contacted to determine alternative methods of asthma medication
administration.
5. For metered dose inhalers with a spacer, have the student:
• Hold the inhaler in one hand in an upright position. In the other hand, hold the
spacer attached to the inhaler.
• Breathe out to the end of a normal breath.
• Place the spacer in the mouth.
• Tilt the head slightly back and start to breathe in slowly.
Please note: For metered dose inhaler use without a spacer, student may use the
open or closed mouth technique. Please see education references, pages 57-58.
Key Points and Precautions:
The inhaler wil stop spraying if it is held upside down. See the manufacturer's
directions for the correct position.
6. Spray the inhaler at the start of a normal breath (inhaling).
Key Points and Precautions:
If sprayed at the end of a breath, the medication wil not work as wel .
7. Breathe in as deeply as possible over two to three seconds.
Key Points and Precautions:
Breathing in too fast makes most of the medicine stay in the mouth and throat rather
than being delivered to the lungs.
8. Take the inhaler/spacer out of the mouth and have student hold their breath eight to
• Wait one to two minutes between puffs.
• Repeat the procedure if another puff is authorized.
Key Points and Precautions:
Do not let the student take more puffs than directed by physician.
9. Determine if medication has improved signs and symptoms and observe for five
minutes.
Key Points and Precautions:
If improved, the student may resume school activities. If not improved, cal school
nurse and parent.
10. If students has:
• Very fast or hard breathing
• Skin sucking in over child's stomach or ribs with breathing
• Breathing so hard they cannot walk or speak
• Lips or fingernail beds turn blue
Cal for help. Call 9-1-1. Repeat quick-relief medication every 20 minutes or as
authorized in student's ISHP. Stay with student and be prepared to do CPR.
Key Points and Precautions:
Have help notify site administrator, school nurse, and parent.
11. Record occurrence and results on logging form.
Mechanical Nebulizer Procedure
To deliver bronchodilators, mucolytics, or other medications directly into the lungs by
means of aerosol instil ation, and to provide high humidity to facilitate the removal of
pulmonary and bronchial secretions.
Equipment and Supplies
1. Air compressor. 2. Connection
3. Medication or saline solution. 4. Medication cup. 5. Mouthpiece and mask. 6. Follow manufacturer's instructions for ultrasonic nebulizers.
Procedure
1. Determine the need for the student to use the nebulizer at school.
Key Points and Precautions:
Review the ISHP and authorized health care provider's authorization. Baseline rates,
depth, effort, noise, color, restlessness, and level of consciousness.
2. Obtain a pretreatment pulse and respiratory rate. Record on log form.
Key Points and Precautions:
Pretreatment vital signs are helpful in monitoring any adverse reaction as a
comparison after medication is given.
3. Monitor heart rate during and after treatment by taking pulse when bronchodilators
are administered.
Key Points and Precautions:
Bronchodilators may produce tachycardia (rapid heartbeat), palpitation, dizziness,
nausea, and excessive perspiration. Stop treatment and call school nurse if student
has any of these signs and symptoms.
5. Assemble equipment and medication, as ordered, near the student.
Key Points and Precautions:
Use students own medication cup, mouthpiece, or mask.
6. Explain the procedure to the student.
Key Points and Precautions:
Use language and demonstration methods that are appropriate for the student's level
of development because the effectiveness of this therapy depends on the student's
efforts.
7. Place the appropriate amount of medication and saline solution or water in the
nebulizers.
Key Points and Precautions:
Do not exceed the ordered amount.
8. Place the student in a comfortable sitting position.
Key Points and Precautions:
Expansion of the lungs and movement of the diaphragm are greatest in this position,
allowing for maximum treatment of the basilar areas of the lungs.
9. Have the student demonstrate mouth breathing. Have them practice if necessary.
Key Points and Precautions:
Demonstrate the procedure if needed.
10. Attach the nebulizer hose to the air compressor and turn it on. A fine mist should be
visible.
Key Points and Precautions:
If output from the nebulizer appears to have decreased or does not mist, check tubing
for tight connections, unplug the device, and check manufacturer's instructions for
trouble shooting. If nebulizer does not mist, cal the school nurse.
11. Have the student place the mouthpiece in his or her mouth if possible.
Key Points and Precautions:
Use the mask if the student cannot use the mouthpiece.
12. Tell the student to breathe in and out through their mouth.
Key Points and Precautions:
This technique al ows the medication to remain in the lungs longer and facilitates
dispersion of the particles.
13. Every two minutes, or as ordered, have the student take an extra deep breath or two,
hold his or her breath briefly, then exhale as slowly as possible. Resume normal
breathing until time for the next deep breaths.
Key Points and Precautions:
Deep breaths ensure that the medication is deposited deep into the lungs. Nose clips
may be used if the student has difficulty breathing through their mouth. Nose clips
require doctor's orders.
14. Observe the expansion of the student's chest.
15. Remove the mouthpiece or mask if a cough occurs during the treatment and al ow
the student to clear the secretions completely and then continue the treatment.
Key Points and Precautions:
Turn off the machine when it is not being used.
16. Give the student time to rest during the procedure if needed.
Key Points and Precautions:
Treatment may take 8 to 20 minutes depending on equipment used.
17. Observe the student for any adverse reactions such as wheezing (bronchospasm)
and excessive mucous deposition causing suffocation, rapid heart rate, nausea, and
dizziness.
Key Points and Precautions:
Wheezing may be due to increased or loosened secretions. If signs of suffocation,
rapid heart rate, nausea or dizziness occur, stop treatment, cal for help, stay with
student, and have help cal school nurse.
18. Continue the procedure until al the medication or fluid has been nebulized.
Key Points and Precautions:
All medication must be used to ensure a complete dose has been given to the
student.
19. Upon completion of the treatment have the student take several deep breaths, cough,
and spit out the secretions.
Key Points and Precautions:
Instruct and demonstrate the technique as needed.
20. Obtain and record student's pulse and respirations and observe student for ten
minutes.
Key Points and Precautions:
If after ten minutes, the student is breathing easier and their pulse and respirations
are within a normal range, then the student may return to their classroom.
21. If students has:
• Very fast or hard breathing
• Skin sucking in over child's stomach or ribs with breathing
• Breathing so hard they cannot walk or speak
• Lips or fingernail beds turn blue
Cal for help. Call 9-1-1. Repeat quick-relief medication every 20 minutes or as
authorized in student's ISHP. Stay with student and be prepared to do CPR.
Key Points and Precautions:
Have help notify site administrator, school nurse, and parent.
22. Wash your hands; have the student wash their hands.
23. Record the date and time;
a. the name of the medication used; b. duration of the treatment; c. the respiratory rate and effort, and the pulse during and after the student's
d. description of the secretions expectorated; e. observation time; f. time returned to classroom; g. and/or any other occurrences.
24. Daily, thorough cleaning of nebulizer is done at home. 25. After each treatment:
a. Put on gloves. b. Rinse the nebulizer, mouthpiece, and/or mask under hot, running water. c. Shake off the excess water. d. Lay parts on paper towels to dry. e. Cover the nebulizer parts with paper towels. f. When the parts are dry, store them in a clean, sealed plastic bag. The tubing does
not have to be cleaned but stored in the same bag with other equipment. Store machine and parts in a safe place that has easy access.
g. Wash sink and spray with approved disinfectant.
26. Remove gloves and wash hands.
G. Appendix
California Education Code (effective January 1, 2005)
CEC SECTION 49423.1 (a) Notwithstanding Section 49422, any pupil who is required to take, during the regular schoolday, medication prescribed for him or her by a physician and surgeon, may be assisted by the school nurse or other designated school personnel or may carry and self-administer inhaled asthma medication if the school district receives the appropriate written statements specified in subdivision (b). (b)
(1) In order for a pupil to be assisted by a school nurse or other designated school
personnel pursuant to subdivision (a), the school district shal obtain both a written statement from the physician and surgeon detailing the name of the medication, method, amount, and time schedules by which the medication is to be taken and a written statement from the parent, foster parent, or guardian of the pupil requesting that the school district assist the pupil in the matters set forth in the statement of the physician and surgeon.
(2) In order for a pupil to carry and self-administer prescription inhaled asthma
medication pursuant to subdivision (a), the school district shall obtain both a written statement from the physician and surgeon detailing the name of the medication, method, amount, and time schedules by which the medication is to be taken, and confirming that the pupil is able to self-administer inhaled asthma medication, and a written statement from the parent, foster parent, or guardian of the pupil consenting to the self-administration, providing a release for the school nurse or other designated school personnel to consult with the health care provider of the pupil regarding any questions that may arise with regard to the medication, and releasing the school district and school personnel from civil liability if the self-administering pupil suffers an adverse reaction by taking medication pursuant to this section.
(3) The written statements specified in this subdivision shal be provided at least
annual y and more frequently if the medication, dosage, frequency of administration, or reason for administration changes.
(c) A pupil may be subject to disciplinary action pursuant to Section 48900 if that pupil uses inhaled asthma medication in a manner other than as prescribed.
California Code of Regulations, Title 5. Education
Article 4.1. Administering Medication to Pupils or Otherwise Assisting Pupils in the
Administration of Medication During the Regular School Day
§600. Authorization.
Pursuant to Section 49423 and subdivision (b) of Section 49423.6 of the Education Code, any pupil who is required to take, during the regular school day, prescribed medication may be assisted by a school nurse or other designated school personnel if both of the fol owing conditions are met:
(a) The pupil's authorized health care provider executes a written statement specifying, at a
minimum, the medication the pupil is to take, the dosage, and the period of time during which the medication is to be taken, as wel as otherwise detailing (as may be necessary) the method, amount, and time schedule by which the medication is to be taken.
(b) The pupil's parent or legal guardian provides a written statement initiating a request to have
the medication administered to the pupil or to have the pupil otherwise assisted in the administration of the medication, in accordance with the authorized health care provider's written statement.
Authority cited: Sections 33031 and 49423.6, Education Code. Reference: Sections 49423 and 49423.6, Education Code.
New article 4.1 (sections 600-611) and section filed 11-20-2003; operative 11-20-2003 pursuant to Government Code section 11343.4 (Register 2003, No. 47).
§601. Definitions.
As used in Section 49423 and subdivision (b) of Section 49423.6 of the Education Code and in this article:
(a) "Authorized health care provider" means an individual who is licensed by the State of
California to prescribe medication.
(b) "Medication" may include not only a substance dispensed in the United States by
prescription, but also a substance that does not require a prescription, such as over-the-counter remedies, nutritional supplements, and herbal remedies.
(c) "Medication log" may consist of a form developed by the local education agency for the
documentation of the administration of the medication to the pupil or otherwise assisting the pupil in the administration of the medication. The medication log may include the fol owing:
(1) Pupil's name;
(2) Name of medication the pupil is required to take;
(3) Dose of medication;
(4) Method by which the pupil is required to take the medication;
(5) Time the medication is to be taken during the regular school day;
(6) Date(s) on which the pupil is required to take the medication;
(7) Authorized health care provider's name and contact information; and
(8) A space for daily recording of medication administration to the pupil or otherwise
assisting the pupil in administration of the medication, such as date, time, amount, and signature of the individual administering the medication or otherwise assisting in administration of the medication.
(d) "Medication record" may include:
(1) The authorized health care provider's written statement;
(2) The written statement of the parent or legal guardian;
(3) The medication log; and
(4) Any other written documentation related to the administration of the medication to
the pupil or otherwise assisting the pupil in the administration of the medication.
(e) "Other designated school personnel" may include any individual employed by the local
education agency who:
(1) Has consented to administer the medication to the pupil or otherwise assist the pupil
in the administration of medication; and
(2) May legal y administer the medication to the pupil or otherwise assist the pupil in the
administration of the medication.
(f) "Parent or legal guardian" means the individual recognized by the local education agency
as having authority to make medical decisions for the pupil.
(g) "Regular school day" may include not only the time the pupil receives instruction, but also
the time during which the pupil otherwise participates in activities under the auspices of the local education agency, such as field trips, extracurricular and cocurricular activities, before- or after-school programs, and camps or other activities that typical y involve at least one overnight stay away from home.
(h) "School nurse" means an individual employed by the local education agency who is a
currently licensed registered nurse and is credentialed pursuant to Education Code section 44877.
Authority cited: Sections 33031 and 49423.6, Education Code. Reference: Sections 44877, 49423 and 49423.6, Education Code.
1. New section filed 11-20-2003; operative 11-20-2003 pursuant to Government Code section 11343.4 (Register 2003, No. 47).
§ 602. Written Statement of Authorized Health Care Provider.
(a) A local education agency may establish specifications for the authorized health care provider's written statement in order to ensure that:
(1) The pupil is clearly identified;
(2) The medication is clearly identified;
(3) The dosage is clearly specified;
(4) The period of time during which the medication is to be taken is clearly specified; and
(5) Other information is obtained that is relevant to administering the medication to the pupil or otherwise assisting the pupil in administration of the medication.
(b) A pupil's parent or legal guardian may deliver the authorized health care provider's written statement to an authorized representative of the local education agency, such as the schoolsite administrator or his or her designee.
(c) A local education agency may require that an amended or new written statement be provided annual y and whenever there is a change in the pupil's authorized health care provider, or a change in the medication, dosage, method by which the medication is required to be taken, or date(s) or time(s) the medication is required to be taken.
Authority cited: Sections 33031 and 49423.6, Education Code. Reference: Sections 49423 and 49423.6,
Education Code.
§ 603. Written Statement of the Parent or Legal Guardian.
(a) A local education agency may establish specifications for the written statement of the pupil's parent or legal guardian in order to ensure that:
(1) The pupil is clearly identified.
(2) Permission is obtained for an authorized representative of the local education agency to communicate directly with the pupil's authorized health care provider, as may be necessary, regarding the authorized health care provider's written statement.
(3) The parent or legal guardian understands what employees of the local education agency will do to administer the medication to the pupil or otherwise assist the pupil in the administration of the medication.
(4) The parent or legal guardian understands his or her responsibilities to enable employees of the local education agency to administer the medication to the pupil or otherwise assist the pupil in administration of the medication, e.g., to ensure that a current authorized health care provider's written statement has been delivered to an authorized representative of the local education agency, or to ensure that the medication is delivered to the schoolsite in a proper container by an individual legal y authorized to be in possession of the medication.
(5) The parent or legal guardian understands how he or she may terminate consent for administration of the medication to the pupil or otherwise assisting the pupil in the administration of the medication.
(b) A local education agency may provide reasonable accommodations to a parent or legal guardian who has insufficient English language proficiency to produce a written statement without assistance or who has a disability that makes it difficult to produce a written statement.
Authority cited: Sections 33031 and 49423.6, Education Code. Reference: Sections 49423 and 49423.6, Education Code.
§ 604. Administration of Medication to Pupils or Otherwise Assisting Pupils in the
Administration of Medication.
(a) A school nurse may administer medication to a pupil or otherwise assist a pupil in the administration of medication as al owed by law and in keeping with applicable standards of professional practice.
(b) Other designated school personnel may administer medication to pupils or otherwise assist pupils in the administration of medication as al owed by law and, if they are licensed health care professionals, in keeping with applicable standards of professional practice for their license.
(c) The pupil's parent or legal guardian may administer medication to the pupil or otherwise assist the pupil in the administration of medication as al owed by law.
(d) An individual designated to do so by the parent or legal guardian may administer medication to the pupil or otherwise assist the pupil in the administration of medication as allowed by law. A local education agency may establish rules governing the designation of an individual by a parent or legal guardian in order to ensure that:
(1) The individual is clearly identified;
(2) The individual is wil ing to accept the designation;
(3) The individual being designated is permitted to be present on the school site;
(4) Any limitations on the individual's authority in his or her capacity as designee are
clearly established; and
(5) The individual's service as a designee would not be inconsistent or in conflict with
his or her employment responsibilities, if the individual being designated is employed by
the local education agency.
Authority cited: Sections 33031 and 49423.6, Education Code. Reference: Sections 49423 and 49423.6, Education Code.
§605. Self-Administration of Medication.
With the approval of the pupil's authorized health care provider and the approval of the pupil's parent or legal guardian, a local education agency may allow a pupil to carry medication and to self-administer the medication. A local education agency may establish rules governing self-administration in order to protect the health and safety both of the pupil and of the whole student body and staff at the schoolsite. Through such rules, a local education agency may describe circumstances under which self-administration may be prohibited.
Authority cited: Sections 33031 and 49423.6, Education Code. Reference: Sections 49423 and 49423.6, Education Code.
§ 606. Delivery and Storage of Medication.
A local education agency may establish policies governing the delivery of medication to the schoolsite (other than medication a pupil is al owed to carry for purposes of self-administration), as wel as the storage of medication in a manner that is secure and maintains the medication's effectiveness.
Authority cited: Sections 33031 and 49423.6, Education Code. Reference: Sections 49423 and 49423.6,
Education Code.
§ 607. Documentation.
A local education agency may establish policies regarding documentation of the administration of medication to pupils or otherwise assisting pupils in the administration of medication to ensure that:
(a) Pupil confidentiality is appropriately maintained;
(b) A medication record is maintained for each pupil to whom medication is administered or other assistance is provided in the administration of medication; and
(c) An appropriate record is kept of pupils who are al owed to carry and self-administer medication.
Authority cited: Sections 33031 and 49423.6, Education Code. Reference: Sections 49423 and 49423.6,
Education Code.
§ 608. Deviation from Authorized Health Care Provider's Written Statement.
A local education agency may establish policies regarding any material or significant deviation from the authorized health care provider's written statement in order to ensure that, as quickly as possible upon discovery, appropriate notification of the deviation is made:
(a) In accordance with applicable standards of professional practice, if the discovery is made by a licensed health care professional; or
(b) To the schoolsite administrator, the pupil's parent or legal guardian, an employee of the local education agency who is a licensed health care professional (if any), and the pupil's authorized health care provider, if the discovery is made by an individual who is not a licensed health care professional.
Authority cited: Sections 33031 and 49423.6, Education Code. Reference: Sections 49423 and 49423.6, Education Code.
§ 609. Unused, Discontinued and Outdated Medication.
A local education agency may establish policies regarding unused, discontinued, and outdated medication in order to ensure that:
(a) Such medication is returned to the pupil's parent or legal guardian where possible; (b) Such medication that cannot be returned to the pupil's parent or legal guardian is disposed of by the end of the school year in accordance with applicable law.
Authority cited: Sections 33031 and 49423.6, Education Code. Reference: Sections 49423 and 49423.6, Education Code.
§ 610. Applicability of this Article.
Nothing in this article may be interpreted as creating a state-mandated local program or as affecting in any way:
(a) The statutes, regulations, or standards of practice governing any health care professional licensed by the State of California in the carrying out of activities authorized by the license; (b) The statutes or regulations governing the administration of medication to pupils or otherwise assisting pupils in the administration of medication by individuals who are not licensed health care professionals, other than Section 49423 and subdivision (b) of Section 49423.6 of the Education Code; (c) The use of emergency epinephrine auto-injectors pursuant to Section 49414 of the Education Code; (d) The content or implementation of a pupil's individualized education program prepared in accordance with applicable provisions of federal and state law, or a pupil's Section 504 Accommodation Plan prepared in accordance with applicable provisions of the federal Rehabilitation Act of 1973.
Authority cited: Sections 33031 and 49423.6, Education Code. Reference: Sections 49414, 49423 and 49423.6, and Part 30 (commencing with Section 56000) of Division 4 of Title 2, Education Code.
§ 611. Issuance and Periodic Updating of Advisory.
The California Department of Education, with the approval of the State Board of Education, may issue and periodical y update an advisory providing non-binding guidance on the administration of medication to pupils and otherwise assisting pupils in the administration of medication. The advisory shal be a program guideline under Education Code section 33308.5, and shal meet the requirements of Education Code section 33308.5 (including the written notification that the guideline is merely exemplary and that compliance with the guideline is not mandatory).
Authority cited: Sections 33031 and 49423.6, Education Code. Reference: Sections 33308.5, 49423 and
49423.6, Education Code.
California Code of Regulations, TITLE 5. Education, Division 1. California Department of Education,
Chapter 2. Pupils, Subchapter 3. Health and Safety of Pupils,
Article 4.1. Administering Medication to Pupils or Otherwise Assisting Pupils in the Administration of Medication
During the Regular School Day
School Emergency Response Procedure for Severe Asthma Episode
NEVER LEAVE A STUDENT WITH BREATHING PROBLEMS ALONE
STAY WITH STUDENT
DO NOT SEND A STUDENT WITH BREATHING PROBLEMS ANYWHERE
IF YOU SEE:
1. Very fast or hard breathing.
2. Skin sucking in over child's stomach or ribs with breathing.
3. Breathing so hard they cannot walk or speak.
4. Lips or fingernail beds turn blue.
1. Stay with student, call for help, and have someone call 9-1-1.
2. Keep student sitting upright.
3. Ask student if their quick-relief medication (Albuterol) is with
them, or have quick-relief medication brought to student and
assist in immediate administration (inhaler or nebulizer).
4. Repeat quick-relief medication every 20 minutes or as authorized
in student's asthma action plan.
5. Watch breathing and be prepared to administer CPR until
paramedics arrive.
6. Have someone notify the school nurse.
7. School nurse or administrator will notify the student's parent
and health care provider.
NAEPP Expert Panel Report Guidelines for the Diagnosis and Management of Asthma–Update on Selected Topics 2002
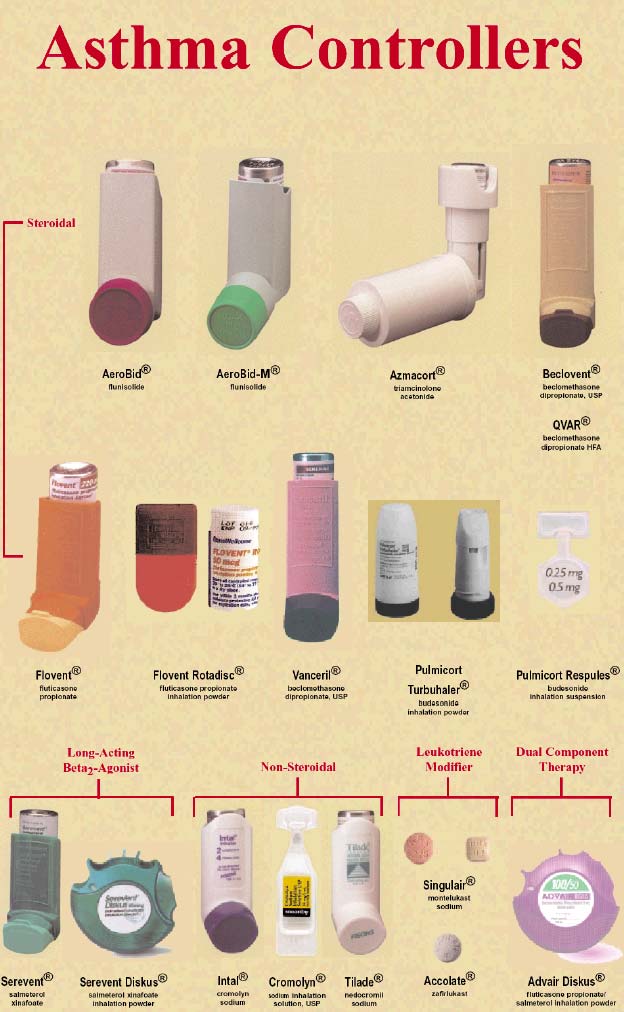
Central California Asthma Project, 2003

Central California Asthma Project, 2003
HOW TO USE A METERED DOSE INHALER (MDI)
Student/Parent Education Reference
This information wil describe how to correctly use inhalers and other breathing devices. It wil also help you to avoid common errors in your technique. If you have any questions about this information or your condition, be sure to ask your doctor or an appropriate health care professional.
A metered dose inhaler (MDI) contains medicine and propel ant in the form of a fine spray. It is used to inhale the medications used to treat asthma and other breathing problems. Each puff from a MDI supplies the same amount of medication.
To receive the most benefit from medication in a MDI, you must get the medication deep into your lungs. Even with proper inhalation technique, only about ten percent of the medication reaches the airways. The use of a 'spacer device' can increase the amount of medication that reaches your lungs.
Using a MDI with a spacer device
A spacer device is a chamber which attaches to any MDI ordered by your doctor. There are several types of spacer devices available. The most common brands are the Ventahaler® and the Aerochamber®. Spacer devices can be purchased at most local pharmacies.
How to use the MDI and Spacer Device:
1. Take the plastic cap off the mouthpieces of the inhaler and the spacer device.
Adapted from Calgary Health Region Patient Education Material/Learning and Development
2. Shake the inhaler wel for several seconds.
3. Fit the inhaler into the rubber end of the spacer.
4. Breathe out slowly and fully. Tilt your head back slightly.
5. Place the spacer in your mouth and close your lips around the mouthpiece.
6. Push down on the canister ONCE to release the medication. At the same time, take a
slow deep breath in.
7. Continue to breathe in SLOWLY. Hold it for as long as it is comfortable (aiming for up
to ten seconds). If you have trouble taking in a long deep breath, you can continue to
breathe normal y for three to four breaths through the mouthpiece.
TIP: If you hear a whistle sound from the Aerochamber, you are breathing too fast.
Slow down your breathing. This wil allow more medication to reach your lungs.
8. Breathe out gently through your nose.
9. If you need more than one puff of medication, wait one minute before repeating steps 2
10. Remove the spacer device from the inhaler and replace mouthpiece caps.
Adapted from Calgary Health Region Patient Education Material/Learning and Development
Metered Dose Inhaler
Open Mouth Technique
Student/Parent Education Reference
1. Remove the cap from the metered dose inhaler (MDI) and shake it wel .
2. Hold the MDI by placing your index finger on top of the inhaler and thumb on the
bottom of the plastic mouthpiece.
3. Tilt your head back slightly and breathe out slowly.
4. Open your mouth and hold the inhaler one to two inches away.
5. As you begin to breathe in slowly through your mouth, press down on the inhaler one
6. Continue to breathe in slowly (three to five seconds).
7. Hold your breath for at least ten seconds to al ow the medicine to reach deep into the
8. Repeat each puff as prescribed by the authorized health care provider. Wait at least
one minute and repeat the above steps.
9. Replace the cap on your MDI when you are finished.
Adapted from Breathe Your Best: A Quality Life Through Quality Care, Rhône-Poulene Rorer Pharmaceuticals Inc., 1998
Metered Dose Inhaler
Closed Mouth Technique
Student/Parent Education Reference
1. Remove the cap from the metered dose inhaler (MDI) and shake it wel .
2. Hold the MDI by placing your index finger on top of the inhaler and thumb on the
bottom of the plastic mouthpiece.
3. Tilt your head back slightly and breathe out slowly.
4. Put the inhaler in your mouth.
5. Press down on the inhaler to release medication as you start to breathe in slowly.
6. Continue to breathe in slowly (three to five seconds).
7. Hold your breath for at least ten seconds to al ow the medicine to reach deep into the
8. Repeat each puff as prescribed by the authorized health care provider. Wait at least
one minute and repeat the above steps.
9. Replace the cap on your MDI when you are finished.
Adapted from Breathe Your Best: A Quality Life Through Quality Care, Rhône-Poulene Rorer Pharmaceuticals Inc., 1998
Peak Flow Monitoring
Student/Parent Education Reference
Use of peak flow meters has greatly improved the ability to determine the child's respiratory status. It provides an objective measure rather than relying on subjective assessments. In addition, it helps to determine the effectiveness of interventions such as medications.
How to use a peak flow meter
1. Discard gum, candy, or food from mouth. 2. Place the indicator at the base of the numbered scale. 3. Stand up. 4. Take a deep breath. 5. Place the meter in mouth and close lips around the mouthpiece.
(Do not put tongue inside the hole.)
6. Blow out as hard and fast as possible. 7. Note the number. 8. Repeat steps 2 through 7 two more times. 9. Write down the highest of the three numbers.
How to use the RED, YELLOW, GREEN ZONE SYSTEM
Once you have obtained the child's current peak flow reading you should determine which of the three zones he/she is currently at by fol owing the steps outlined:
1. Record the highest of the three current peak flow readings.
2. Obtain the child's "personal best" from the Asthma Management Plan.
(The child's "personal best" should be determined when the child is symptom free, in cooperation with the health care provider, and should be redetermined regularly.)
3. Calculate the peak flow percentage as outlined below. Compare the result
from this line to the child's zone chart to determine course of action.
Calculating the Peak Flow Percentage
• Divide the current peak flow reading by • Current Reading: 250
the child's "personal best."
• Personal Best: 300
• Multiply by 100.
• Current/Personal Best: 250 / 300 = 0.83
• Record the result as a percentage.
• Multiply by 100: 83 percent of personal best
Source: National Asthma Education and Prevention Program (NAEPP), National Institutes of Health (NIH)
H. Resources
AIRNOW Kid's Air
An interactive website where kids can learn about the Air Quality Index (AQI) and how air quality effects their health.
Air Quality Index (AQI) AIRNOW
URL http://www.epa.gov/airnow/
Learn more about the Air Quality Index and about how clean the air is and whether it wil affect your health. EPA, state, and local agencies work together to report current and forecast conditions for ozone and particle pol ution. AIRNow provides forecasts of next day air quality.
American Lung Association
Open Airways for Schools is an award-winning program. In 1992, it was honored with a Health Education Research Award from the National Asthma Education and Prevention Program. The program teaches children, aged 8-11, how to detect the warning signs of asthma, including the environmental factors that can trigger an attack. It has been proven that children who participate in Open Airways for Schools have fewer and less severe asthma attacks, improve their academic performance, have more confidence in their ability to take more steps to manage their asthma, and exert greater influence on their parents' asthma management decisions.
Asthma Action Plan for Schools and Families
The California Asthma Public Health Initiative led a statewide task force in the development of an asthma action plan for school age children in California that would meet the needs of children, families, schools and health providers.
The plan is approved by the California Department of Health Services and is provided as an additional resource for schools and health providers to improve the availability in schools of a current asthma action plan for every child with asthma. Download a copy of the Asthma Action Plan for Schools and Families.
Asthma & Allergy Foundation of America (AAFA), Southern California Chapter
URL http://www.aafasocal.com
AAFA is the premier patient organization dedicated to improving the quality of life for people with asthma and allergies and their caregivers through education, advocacy, and research. Some of their children's asthma programs include Asthma Camp, Air Power Games, and the Breathmobiles.
Best Practices for Communicating Air Quality and Related Health Information
The Children's Environmental Health Center (CEHC) in Cal/EPA and the California Asthma Public Health Initiative (CAPHI) in the Department of Health Services undertook a one-year study of how local air districts communicate air quality and related health information to school districts and organized after-school programs. The results of the joint study are presented here in the form of a list of "best practices" for communicating air quality information from air districts to school districts and after-school programs, and from school districts to their schools and staff. CEHC and CAPHI also developed a sample action plan that school districts could use as a model for their own plans to address outdoor activities on poor air quality days.
California School Nurses Organization (CSNO)
URL http://www.csno.org
The mission of CSNO is to promote and strengthen its members in their role as the primary health professional within the educational community. This wil be accomplished through: professional development, legislative advocacy, communication with members, membership recruitment, public relations, governance, and leadership development.
California Asthma Resource (CARE) Directory
URL www.epeu.org/care
The CARE Directory is a searchable comprehensive database of asthma information
resources. It provides a central location for references to patient educational materials,
including many that are available in different languages. The CARE Directory was developed
by the Epidemiology and Program Evaluation Unit at the California Department of Health
Services, in partnership with the American Lung Association of California and the California
Asthma Public Health Initiative.
Division of Adolescent and School Health
Download the Strategies for Addressing Asthma within a Coordinated School Health Program.
Emergency Medical Services (EMS) Authority Inhaled Medications Training
Download the Nebulizer and Inhaled Medication Training Curriculum developed by the EMS division.
Environmental Protection Agency: IAQ Tools for Schools
URL http://www.epa.gov/iaq/schools/
The IAQ Tools for Schools program is a comprehensive resource that can help you maintain a healthy environment in your school buildings by identifying, correcting, and preventing IAQ problems.
"How Asthma Friendly is Your School?" Checklist
Parents and school staff wil find the checklist useful to determine how well their school setting accommodates children with asthma.
The checklist can help to identify sources of problems in schools for children with asthma. The scorecard format can be used by parents, teachers, and school nurses to help pinpoint specific areas that may cause problems for children with asthma. It is available in English and Spanish. Both are accompanied by an extensive list of organizations that can serve as useful resources for parents and school staff to make asthma-friendly changes in the school.
Managing Asthma: A Guide for Schools
Download Managing Asthma: A Guide for Schools, a guide developed by the NAEPP and intended to assist schools that are planning and/or maintaining an asthma management program. This guide provides fol ow-up steps for schools that currently identify students with asthma through health forms or emergency cards or plan to do so.
National Education Association Health Information Network
URL http://www.asthmaandschools.org/
Asthma and Schools consolidates information about asthma-related resources for school personnel working with grades K-12. The simple, searchable database links to educational materials, medical information, websites, and other resources.
National Heart, Lung, Blood Institute
Download the "Asthma Awareness Curriculum for the Elementary School Classroom," "Making a Difference: Asthma and Physical Activity in the Schools," and "Making a Difference: Asthma Management in the School" booklets and other school related information.
Resolution on Asthma Management at School
Download the resolution developed by the National Asthma Education Prevention Program (NAEPP) Coordinating Committee, including the American School Health Association.
SchoolAsthmaAllergy.com provides accurate, current, and useful tools and information to empower all of those caring for school-aged children with asthma and allergies.
Starlight Starbright Children's Foundation
Starlight Starbright is a non-profit organization that is leading the development of an innovative Asthma Tool Kit for Schools. Availability is anticipated in early 2005.
I. Bibliography
Akinbami, Lara J. and Kenneth C. Schoendorf, Trends in Childhood Asthma: Prevalence,
Health Care Utilization, and Mortality, Pediatrics, Aug 2002; 110: 315 - 322.
American Academy of Al ergy, Asthma and Immunology, Inc., Academic Services Consortium. Pediatric Asthma: Promoting the Best Practice, Milwaukee, 1999.
American Academy of Al ergy, Asthma & Immunology, Inc., The Allergy Report, Volumes I-III, Milwaukee: Wisconsin, 2000. www.theallergyreport.org/reportindex.html
American Association of School Administrators, Asthma Wel ness Keeping Children with Asthma in School and Learning, School Governance and Leadership, Vol. 5, No. 1, Spring, 2003. http://www.aasa.org/publications/sgl/Spring_2003.pdf
California Department of Health Services, Strategic Plan for Asthma in California, 2002. www.dhs.ca.gov/ps/cdic/cdcb/Medicine/Asthma/Documents/SP/Final%20Strategic%20Plan.pdf
Department of Health and Human Services, Centers for Disease Control and Prevention, Strategies for Addressing Asthma Within a Coordinated School Health Program, 2002. http://www.cdc.gov/HealthyYouth/asthma/pdf/asthma.pdf
Farber, Harold, M.D. and Michael Boyette. Control Your Child's Asthma: A Break Through Program for the Treatment and Management of Childhood Asthma, New York: Henry Holt & Co., 2001.
Gregory, Elizabeth, Empowering Students on Medication for Asthma to be Active Participants in Their Care: An Exploratory Study." The Journal of School Nursing, Vol. 16, No. 1 (February 2000).
Illinois Department of Human Services, Division of Community Health and Prevention, Office of Family Health, Asthma Management: A Resource Manual for Schools, January 2001.
Mannino DM, Homa DM, Akinbami LJ, et al. Surveil ance for Asthma-United States, 1980–1999. MMWR Morb Mortal Wkly Rep2002; 51(SS-1): 1 –13. www.cdc.gov/mmwr/preview/mmwrhtml/ss5101a1.htm
Michigan Asthma Strategic Planning Initiative Task Force, Asthma in Michigan – A Blueprint for Action, May 2001.
National Asthma Education and Prevention Program. Expert Panel Report II: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: National Heart, Lung, and Blood Institute. www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm
National Asthma Education and Prevention Program. Expert Panel Report: Guidelines for the Diagnosis and Management of Asthma, Update on Selected Topics, 2002. Bethesda, MD: National Heart, Lung, and Blood Institute; June, 2003. www.nhlbi.nih.gov/guidelines/asthma/index.htm Newacheck PW and N Halfon. Prevalence, impact, and trends in childhood disability due to asthma. Arch Pediatr Adolesc Med.2000; 154: 287 –293.
Schering-Plough Corporation, Respiratory Guidelines and Programs, Teaching Tool kit, 2000.
Source: https://fhop.ucsf.edu/sites/fhop.ucsf.edu/files/wysiwyg/ip_SchoolAsthmaGuide.pdf
The skinless work group: facing the uncertainty of resting on a void
International Journal of Applied Psychoanalytic StudiesInt. J. Appl. Psychoanal. Studies (2015)Published online in Wiley Online Library(wileyonlinelibrary.com) DOI: 10.1002/aps.1430 The Skinless Work Group: Facingthe Uncertainty of "Restingon a Void" MATÍAS SANFUENTES This paper examines the conflicts and resistances that contemporary organizationsface in the effort of generating new and challenging work opportunities. Assumingthe metaphoric and real character of the ‘body of the organization', differentdilemmas that work groups tackle in the generation of collaborative and productivespaces are described. Based on a socioanalytic consultancy carried out with agroup of Reichian body psychotherapists, the study illustrates the complexities todelineate a common strategy and to overcome the threatening porosity and incon-sistencies of the ‘institutional skin'. The lack of a body support is particularlyparadoxical for a group of psychotherapists that base their therapeutic method onbody techniques, and which crystallizes as an institution the place of rejectionand exclusion that Reich and the concern for the body have historically occupied.Copyright © 2015 John Wiley & Sons, Ltd.
caipisa.it
Sede: via Cisanello 2, 56124 Pisa CLUB ALPINO ITALIANO Anno XXX - Numero 1 - 2011 I monumenti di Piazza del Duomo sullo sfondo delle Apuane innevate. Questa bella fotografia scattata da Enrico Mangano dalla terrazza dell'Hotel Duomo costituisce l'immagine di copertina del volumetto "Le nostre Alpi", che dopo una lunga attesa ha visto finalmente la luce. La pubblicazione, a carattere essenzialmente fotografico, è stata presentata durante l'assemblea annuale del