Birthbrochure_en.pdf
A clear account of test tube fertilisation 1.1 More and more couples are having problems achieving a pregnancy 1.2 What tests have to be carried out? What exactly is in-vitro fertilisation? 2.1 IVF treatment demands a lot from you and your partner 2.2 Who is in the IVF team? How does normal fertilisation occur? The IVF treatment programme 4.1 Maturation of eggs is stimulated 4.2 Do not miss a check-up 4.3 Ovulation comes into view 4.4 Picking up the eggs 4.5 The best eggs are fertilised 4.6 A tense moment: replacement of one or more fertilised eggs 4.7 Replacement follows quickly What is the cost of in-vitro fertilisation? IVF and micro-injection (ICSI) for serious male infertility 8.1 Who is eligible for egg donation? 8.2 Where do the donor eggs come from? The blastocyst stage 9.1 Increasing the likelihood of implantation 9.2 Nature and procedure 10. Pre-implantation diagnosis (PGS and PGD) 11. IVF and ICSI may be worth a try for you A clear account of test tube fertilisation Infertility is an emotionally loaded subject. Medical science, however, has made some important progress in this area, so that a solution can be found for the majority of couples.Sub-fertile or less fertile couples are those who actively try to achieve a pregnancy for at least one year and do not succeed. This happens to 15% of all couples.
1.1 More and more couples are having problems achieving a pregnancy This problem probably occurs more frequently now than in the past, and a few important reasons can be mentioned for this:» Many young people give priority to their profession and career and only think about having children at a later stage, while woman's natural fertility reduces with age; » In the environment around us, we come into contact with many harmful substances every day – either consciously or not; many of these harmful substances have a structure that is very similar to artificial female hormones (oestrogens) and they have a negative impact on the quality of sperm.
These are two purely social reasons that can account for the declining fertility facing more and more couples.
1.2 What tests have to be carried out? Before we can trace possible difficulties affecting a couple, we systematically go through the various steps that lead to a naturally occurring pregnancy. The cause of infertility lies in one of those steps.
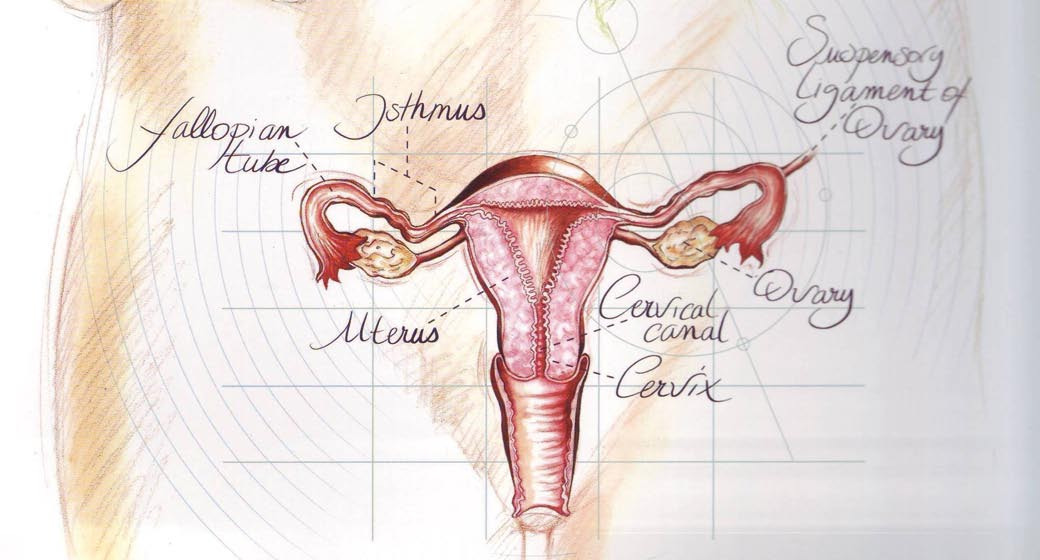
If one of the millions of sperm cells comes into contact with the egg, fertilisation takes place in the Fallopian tube. The egg then divides into a large number of cells. This clump of cells implants itself into the mucous membranes of the womb and there it continues to develop into a full-term baby at birth.
Both the man and the woman are involved in the testsHowever, the egg and sperm cell are unable to merge for any reason, the couple is infertile. In this case, either the sperm quality is not good enough, or something is wrong with the woman's reproductive organs. From medical statistics we know that in 40% of infertility cases, the cause should be sought in both man and woman. Therefore, both man and woman should be involved in the start of the diagnostic work-up.
A clear account of test tube fertilisation Male fertility testsMale fertility is determined by means of a sperm test. The quality of sperm is assessed on the basis of a microscopic investigation. Fertile sperm cells are highly motile and normal in shape. There must be enough fertile sperm cells in the sample. If this is the case, the man is usually fertile and the remainder of the tests will be concentrated on the woman. If the quality of the sperm is not high enough, a thorough physical examination of the man takes place, possibly followed by some technical investigations in the laboratory. A demonstrable cause of reduced sperm quality is only found in a minority of men. Opportunities to treat these men by means of medication or surgical intervention are therefore limited. In very few cases, it is necessary to resort to donor insemination. For most couples, since the implementation of in-vitro fertilisation with sperm cell micro-injection (ICSI), it is possible to achieve a pregnancy using the partner's own sperm. In donor insemination, frozen sperm from an anonymous donor is used.
Female fertility testsFemale fertility is initially determined by a simple anatomical investigation. During this investigation the cervix of the womb is checked. It is ascertained whether there is any inflammation and whether, midway in the menstrual cycle, there is plenty of good, stretchy mucus. The uterus or body of the womb should be normal in shape so that an embryo can implant within it and continue to grow into a full-grown baby. The investigation, also called hysterography (HSG), is carried out by taking a few X-rays while a contrast medium is injected through the cervix. This HSG also clearly shows whether the Fallopian tubes are open. An alternative examination is a hysteroscopy, in which an ‘optical instrument' (a small telescope with a diameter of about 6 mm) is used to view the uterine cavity via the cervix.
If the fertility problem has already existed for a number of years or if the patient's medical history points towards earlier infections, operations or very painful periods, it is often decided to carry out a laparoscopy. This is a surgical investigation in which an optical instrument is inserted through the navel. The internal appearance of the pelvis is then visible on a TV monitor and we obtain a perfect and detailed overview of the internal reproductive organs. Minor abnormalities discovered during this investigation can usually be cured during the surgical investigation itself.
After these tests it may become clear that the woman's reproductive organs are intact, but that the functioning of her sex hormones is disturbed. The woman does not usually notice anything about this aspect of fertility, except for a rather irregular cycle. Problems of this type can be ascertained by means of a laboratory investigation (i.e. a blood test). Ultrasound scans may also be used to investigate whether an egg is maturing.
A clear account of
test tube fertilisation
2. What exactly is in-vitro fertilisation?
Everyone has heard of "test tube babies" and the terms "in-vitro fertilisation" or IVF are also used. But what does IVF really mean and how does this fertility process works? Translation of these words makes things become rather clearer. "Fertilisation" means "making pregnant", and "in vitro" means "outside the body". This means that an egg is put together in a glass dish with a large number of sperm cells so that it can be fertilised. The fertilised egg is then replaced in the woman's body and after this procedure a normal pregnancy can take place.
The treatment can be broadly divided into five stages:
» Stimulating the process of egg maturation
In a normal menstrual cycle, only one egg matures in each cycle. More eggs are needed for an in-vitro fertilisation treatment, to increase the likelihood of success. The development of multiple eggs is promoted using a combination of medicines.
» Removal of eggs by aspiration
After this ovarian stimulation process of around 10 to 12 days, the doctor removes the mature eggs from the body to fertilise them outside the body. We call this the ‘pick-up', in which eggs are aspirated from the ovaries.
A few hours after the removal of the eggs from the body, eggs and sperm are brought together. The egg can now be fertilised.
» Replacement of the embryo
If fertilisation has been successful, one or more fertilised eggs (these are already referred to as embryos) are replaced in the womb.
» Checking and outcome
A tense time then follows: pregnant or not? During this period the woman continues to be monitored by her doctor. After about three to four weeks there usually is an appointment with the treating doctor to discuss the results.
A clear account of
test tube fertilisation
Normal fertilisation
2.1 IVF treatment demands a lot from
you and your partner
A course of IVF treatment takes a few weeks. During this period, from the first day of menstruation, the treatment takes up a lot of your time. This usually begins by taking medicines to stimulate maturation of eggs. Blood tests, ultrasound scans and gynaecological examinations also take time. Your daily routine will be disordered for a month. You probably will consider that this is worthwhile, but it is still good to think about the consequences of an IVF treatment.
In addition to the investment of time, both the man and the woman are very emotionally involved in the treatment. Particularly after replacement of the fertilised eggs, a very tense period begins. Feelings of fear, uncertainty and hope play a dominant role. For most couples, this stage is the most difficult in the whole course of treatment. You are not alone, however, and you can count on help and support from the IVF team.
2.2 Who is in the IVF team?
IVF is an invasive treatment that requires knowledge and takes time.
For this reason many hospitals are equiped with a multidisciplinary team.
Its composition is different in each hospital but it usually consists of:» gynaecologists;» an andrologist;» nurses or counsellors;» secretaries;» one or more embryologists;» IVF laboratory workers;» a psychologist;» a social nurse;» laboratory personnel from the disciplines involved (isotope laboratory, andrology,
haematology, clinical chemistry and microbiology).
All the team members work closely together to achieve the best results. The IVF team is there to treat, offer guidance and answer questions. So do not hesitate to discuss your problems or uncertainties with them. The IVF team can offer support on many occasions.
3. How does normal fertilisation occur?
To understand the IVF method properly, we must first explain how fertilisation takes place under normal circumstances. In one of the two ovaries – from the first day of the menstrual cycle – an egg begins to ripen. This egg is only visible under the microscope and it is snugly packaged in a bubble of fluid (a follicle). This follicle grows to a diameter of approximately two centimetres and then bursts. The egg is released and captured by one of the Fallopian tubes, which are linked to the womb. We call this moment ovulation, and it takes place approximately midway
A clear account of
test tube fertilisation
IVF treatment programme
between two episodes of menstruation. You can imagine that blocked Fallopian tubes, for example, interfere with this process. The egg then cannot pass through the Fallopian tube and cannot be fertilised by sperm cells there. In short, natural fertilisation is impossible in this case.
If the egg meets the sperm cells in the Fallopian tube and is fertilised, it takes four days for the egg to reach the womb. The egg – which is already dividing – implants itself into the mucous membranes of the womb. This implantation is the beginning of a pregnancy.
4. The IVF treatment programme
4.1 Maturation of eggs is stimulated
With the help of medication, development of eggs is stimulated. Normally only one egg matures in each cycle. Through treatment with hormone preparations, it is often possible to have several eggs maturing at once. More mature eggs will soon mean a greater likelihood of fertilisation and ultimately pregnancy. The hormonal preparations which are used are:» A nasal spray or injection from day 1 or day 21 of the cycle. This medication
suppresses production of the hormones produced in a spontaneous cycle. The medication also suppresses ovulation and makes it possible to monitor hormonal stimulation better;
» Injections contain the hormones that stimulate the ovaries to produce more than
one egg. The injections are given for a period of 10 to 14 days.
4.2 Do not miss any appointment
You also have to visit the hospital regularly during hormone treatment for blood tests and ultrasound scans. The IVF team will tell you all about this and provide the prescriptions for the medication you need. On the basis of the findings during the check-ups, the team will determine the correct dose of the hormone preparation. This quantity may vary from day to day. The investigations are also important to determine the correct date for the puncture.
4.3 Ovulation comes into view
If the tests show that the eggs are almost mature, you will be prescribed a different hormone preparation. This medication accelerates the maturation process: your puncture will take place 34 to 38 hours after administering this hormone preparation. Puncture – aspiration of the follicles in order to obtain the eggs – must of course have taken place before ovulation.
4.4 Picking up the eggs
Removing the eggs is a minor surgical intervention in itself and it is done under ultrasound guidance. Ultrasound puncture takes place as follows: a probe containing
A clear account of
test tube fertilisation
IVF treatment programme
a hollow needle is attached to the ultrasound set. The gynaecologist views the ovaries via the vagina using the ultrasound probe. The follicles containing the eggs are punctured and the eggs, together with some fluid, are gathered into a tube. You and your partner can follow the procedure on the screen. So you are completely involved, because a local anaesthetic is sufficient for this procedure.
4.5 The best eggs are fertilised
The laboratory identifies and then evaluates the eggs and places them in a dish with the necessary growth medium containing nutrients. The contents of that dish more or less imitate the situation in the Fallopian tubes. The temperature and environmental factors are approximately the same as in the mother's body. This creates all the conditions for natural fertilisation.
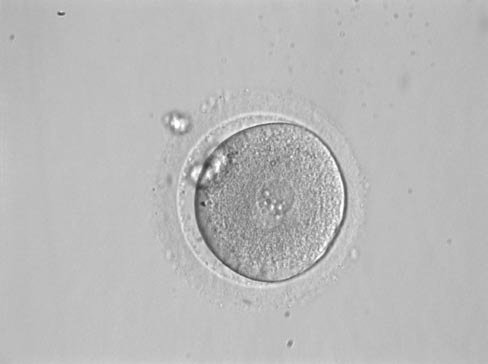
If the woman feels good after the intervention, she can go home. While selecting
Fertilised egg: PN stage
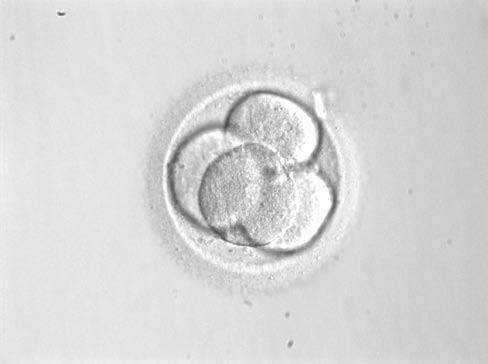
the eggs the sperm sample is also viewed. The quality of not only the eggs but also the sperm is very important. The most motile sperm cells are selected and placed together with the eggs. After 48 hours you can see whether the fertilised eggs have developed into embryos.
The fertilised eggs that have developed well are replaced within the body after 2 to 3 days. This is called an embryo transfer. If there has been no cell division, the embryo transfer cannot take place. This situation will be discussed with you.
4.6 A tense moment: replacement of one or more
As previously described, quite often multiple embryos are eligible for replacement. This is a very good sign, because even after the embryos have been replaced nature takes over and decides which embryo will continue to divide to become a child. The more embryos there are, the greater the likelihood of a pregnancy. Usually the gynaecologist decides together with you to place a maximum of three embryos within the uterus. There are legal rules governing this. If there are too many embryos, it is discussed in advance what should be done with the remaining embryos. Sometimes the possibilities include freezing them. Of course the IVF team can tell you more about this.
4.7 Replacement follows quickly
Two to three days after puncture, the gynaecologist returns the healthy embryos to the womb. This is done as an out-patient procedure, where no anaesthetic is needed. A thin catheter is inserted into the uterus via the vagina, containing a small quantity of fluid in which the embryos are "swimming''. The embryos are thus inserted into the womb. Hopefully they will implant into the womb – just as in a normal pregnancy – allowing cell division to continue.
A four-cell embryo
If the fertilised eggs have been replaced in the body, it does not mean that you are pregnant (yet). It takes up to three weeks before we know the outcome. The most
A clear account of
test tube fertilisation
difficult period therefore now begins. After the pick-up, hormonal support for the mucous membranes of the uterus is begun by inserting capsules of progesterone vaginally. After a first blood test and hormonal check the gynaecologist can decide to prescribe additional injections administered once every three days.
5. Pregnant or not?
It is not easy to continue living your life during this period as if nothing has happened. Feelings of anxiety, hope and doubt follow at a rapid pace. During this period, when you are wrestling with all kinds of questions and emotions, you can always fall back on the expert advice and support of the IVF team. It also makes sense to continue with your daily routine, such as work or other activities. This not only serves as a distraction, but it also ensures that you do not become too focused on a pregnancy which is still uncertain.
Look up friends and acquaintances when you are finding things difficult. Be realistic, but do not hide your feelings. An open discussion with a fertility expert may also provide some relief. It makes sense only to tell a small group of people (family or good friends) about your treatment, since otherwise you will be bombarded with well-intentioned but often burdensome questions.
Positive result: investigationsIf you have not yet menstruated during three weeks after replacement of the fertilised eggs, then a final blood test follows. If this test is positive, the gynaecologist will usually carry out an ultrasound scan a few weeks later to see whether the pregnancy is progressing well. During these weeks you are constantly being assessed. If the ultrasound scan reveals a heartbeat, you can cautiously begin to rejoice in the fact that you are pregnant.
Negative result: coping and discussionIf you menstruate, the treatment has unfortunately failed. You will have to cope with this of course, since unconsciously you will have assumed that everything would go well. You should always make an appointment with your gynaecologist in order to discuss what to do next. Or you can repeat the treatment after a resting cycle or you can have the previously frozen embryos replaced. Or you can even wait a couple of months. The choice is always yours.
A couple coming for treatment must also be informed from the very beginning that about three attempts may be needed. Nevertheless, it does not make sense to continue such treatment endlessly. After a failed treatment a discussion takes place with a gynaecologist and you will be informed about what to do next.

A clear account of
test tube fertilisation
How much does it cost
What is the likelihood of a pregnancy?If it is possible to replace several embryos, the likelihood of a pregnancy is about 30% each time replacement takes place. This percentage is not much less than the natural likelihood of becoming pregnant. Of course the quality of the egg and sperm cells also influences the result.
However, at every stage in the treatment program, unforeseen complications can occur. Sometimes the ovaries react too quickly and ovulation takes place before puncture takes place. It is possible that none of the eggs will be fertilised. Sometimes implantation goes wrong. The likelihood of a miscarriage is also higher. Only nature can control the way in which the body responds.
It is good to understand that a treatment can sometimes fail. This is not a reason to be discouraged. For many couples, IVF has turned out to be the way to have children. As well as disappointing results there have also been a good number of successes. This is a reason to consider IVF as a serious option if you want children and cannot become pregnant – completely – naturally. You can contact the experts from the Centre for Reproductive Medicine about this.
In-vitro fertilisation is now widely spread and it is certainly no longer experimental. While the IVF technique originally was almost used exclusively for blocked Fallopian tubes, it is now increasingly being used for problems of reduced male fertility as well.
6. What is the cost of in-vitro fertilisation?
The cost of IVF treatment is currently paid by the government. If you are under 43 years of age, reimbursement is available for six cycles of treatment.
IVF laboratory assistant
7. IVF and micro-injection (ICSI) for
serious male infertility
In the last decades, researchers have proven that sperm quality has declined significantly. Experts have been looking hard for possible reasons for this.
It may be related to external factors that affect each one of us, whether we are aware of it or not. This has an impact on the fertility of couples. We can certainly see that the cause of a couple's wish for children remaining unfulfilled must increasingly be sought on the male side.
If we are able to use specific laboratory techniques (capacitation) to get at least 5 million motile sperm cells from the ejaculate, this sperm concentrate can be injected into the womb (intra-uterine insemination).
A clear account of
test tube fertilisation
Serious male infertility
If there are at least 500,000 sperm cells, these can be brought into contact with eggs in the laboratory under the most favourable conditions. In this method, which is virtually always known as in-vitro fertilisation or IVF, 60 to 80% of the eggs can be fertilised.
In some cases, however, there are so few good quality sperm cells that the likelihood of fertilisation is virtually non-existent. The only solution for this so far has been artificial fertilisation using sperm donated by a fertile man, which is known as donor sperm.
Scientific research has now even found a solution for couples with highly reduced male fertility. This technique is called intracytoplasmic sperm injection or ICSI.
This is a method that has completely transformed our understanding of the normal treatment for male subfertility, since it requires only one sperm cell to fertilise an egg.
Another indication for this micro-injection technique arose when it was seen in fertility centres that fertilisation did not take place with a conventional IVF treatment in 15% of attempts.
First of all, the sperm cells have to bind to the coating around the egg (the so-called zona pellucida). After binding, the sperm cell undergoes a reaction and penetrates the coating of the egg. The sperm cell then fuses with the wall of the egg before penetrating and being fertilised. Techniques like ICSI have been developed to help those sperm cells with greatly reduced fertilisation potential to overcome these barriers. ICSI (intracytoplasmic sperm injection) consists of the injection, using a fine glass pipette, of a single sperm cell that no longer even needs to be motile, into the inside or cytoplasm of the egg.
Intracytoplasmic sperm injection (ICSI) (1 sperm cell)
A clear account of
test tube fertilisation
This ICSI technique is also a solution for very serious male factors. Sperm can be obtained surgically from the epididymis (MESA: microsurgical epididymal sperm aspiration) or via testicular sperm extraction (TESE). After sperm extraction using MESA or TESE, ICSI will also be used on the eggs so that embryos can be transferred at a later stage.
In egg donation a donor gives up her eggs to a couple who would like to have children but where the woman is unable to become pregnant. In the laboratory one or more donated eggs are brought together with her partner's sperm cells. If the fertilisation is successful, the embryo or embryos are replaced in the womb of the female partner in the couple. This replacement is painless.
8.1 Who is eligible for egg donation?
The largest eligible group consists of women who (now) have no eggs, due to reasons such as:» an operation where both ovaries have been removed;» poorly functioning ovaries;» abdominal irradiation or chemotherapy;» early menopause.
Another group consists of women who are carriers of serious hereditary diseases. Women who do not have their own eggs also lack the hormone production in the ovaries which is needed to allow the egg to mature and maintain the pregnancy. The woman in whom the fertilised eggs are replaced is therefore given hormone-replacement medication.
8.2 Where do the donor eggs come from?
The best option is to maintain the principle of anonymity. In anonymous donation, the eggs come from IVF patients who give permission for their excess eggs to be used. If donor eggs are available, the male partner in the couple is asked to bring in his sperm sample so that the donor eggs can be inseminated. It is not yet possible to freeze eggs. There is a great shortage of eggs. Women who wish to give up their eggs can collect information from IVF nurses. If you provide a candidate egg donor this can significantly speed up your own treatment.

A clear account of
test tube fertilisation
9. The blastocyst stage
In in-vitro fertilisation, or IVF, the fertilised eggs are nurtured in an artificial fluid and then replaced in a womb 2 or 3 days later. In natural fertilisation, the developedembryo has no contact with the womb until 5 days later, where it eventually attaches and implants. It has become technologically possible to allow the fertilised eggs to develop into embryos over 5 to 7 days after fertilisation, so that the natural time for the embryo to arrive in the womb is completely respected. These 5 day old embryos are called blastocysts.
9.1 Increasing the likelihood of implantation
This method is used to increase the likelihood of implantation of the embryo in the case of specific indications. These are:» At least three consecutive failures after replacement of the embryo, despite a
normal uterine cavity, progesterone and luteal phase length. Progesterone is a hormone that ensures that the mucous membranes of the womb are made ready for implantation of the embryo. The luteal phase is the period after ovulation and it is characterised by the appearance of a corpus luteum from the burst ovarian follicle, which secretes progesterone;
» The need to avoid the risk of multiple pregnancy, due to an abnormally
Microscopic image
» Confirmed embryo quality problems after IVF, where the ability to develop needs
to be investigated;
» Risk of hyperstimulation.
9.2 Nature and procedure
» Egg collection and fertilisation
Under local anaesthesia, the mature eggs are gathered via the vagina. This is done under ultrasound monitoring.
In IVF, the mature eggs are inseminated 3 to 6 hours after collection with 4,000–12,500 sperm cells and cultivated at 37˚C.
In ICSI (= micro-injection), the eggs are injected 2 to 4 hours later and after pre-treatment with one sperm cell, after which they are placed in a drop of nutrient fluid at 37˚C.
» Cultivation into blastocysts
The fertilised eggs are transferred to specific growth media one day after insemination. Embryo development is monitored daily up to and including the 7th day after insemination.
Depending on the appearance of the blastocyst stage, replacement is scheduled between the 5th and 7th day after insemination.
» Freezing of blastocysts
Excess blastocysts are frozen on days 5, 6 and 7 after insemination.
A clear account of
test tube fertilisation
10. Pre-implantation diagnosis (PGS and PGD)
Pre-implantation genetic screening (PGS) for aneuploidy offers an extra treatment option for couples with a low genetic risk. It is a derivative of pre-implantation genetic diagnosis (PGD) for couples with a high genetic risk of transmitting an inherited disease. PGS for aneuploidy is also carried out on one or two cells of the embryo (blastomeres), but it is limited to determining the presence or absence of those chromosomes which are involved in early abortions (X, Y, 13, 16, 18, 21 and 22). Studies have shown that aneuploidy is the most important factor in failure of implantation after medically guided reproduction (Dutch: MBV) in women aged over 37. PGS is also said to result in more knowledge about morphologically "normal" embryos in young women with repeated miscarriages and in patients with repeated failures of fertility treatments.
In collaboration with the Centre for Medical Genetics of the UZ Gent [Ghent University Hospital], a PGS programme was started up for the above groups of patients. The numerical chromosomal abnormalities for X, Y, 13, 18 and 21 will be determined and in the future possibly also for other chromosomes. Only embryos that satisfy this ‘partial' euploid genetic diagnosis and also develop morphologically correctly are considered further for replacement. It should become clear in future whether there is also a role for PGS in ‘single embryo transfer' in order to avoid twin pregnancies.
PGD can be carried out in some inherited diseases where the genetic condition can be localised by genetic testing. Through analogue techniques, embryos can then be tested to see whether or not they have the condition, and afterwards only the healthy embryos will be replaced. This is, of course, a specific technique which is only used in selected cases.
11. IVF and ICSI may be worth a try for you
In this booklet we have tried to give you some insight into the various methods of ‘test tube fertilisation' and the variants that exist. Research is still continuing. We are looking forward to solving fertility problems, and to a way of refining the existing treatments. If you are considering undergoing such a treatment, please contact the Centre for Reproductive Medicine for more information.
Above all, take time to decide together with your partner what you should do.
For many people, IVF, ICSI, MESA or TESE and egg donation offer the last hope of having a child.
Source: http://www.birth.be/BirthBrochure_en.pdf
Cti20414_vb_brochure_a4.indd
Built on the proven track record of the classic vbSeries® portable vibration analyzers and balancers, the all-new vbSeries data collectors, analyzers, and balancers have been re-engineered from the ground up to off er leading-edge reliability, accuracy, and usability. oved er onomics for wa gonomics for w lkaro alkar und data col ection ound data collection
sigmabooks.co.kr
Albala, Ken. Beans: A History. Berg, 2007 Allen, Stewart Lee. In the Devil's Garden: A Sinful History of Forbidden Food. Ballantine Books, 2002. Andrews, Jean. Peppers: The Domesticated Capsicums. University of Texas Press, 1984. Barkas, Janet. The Vegetable Passion. Charles Scribner, 1975. Behr, Edward. The Artful Eater. Art of Eating, 2004.