Tais-med.ru2

Neuroscience in Anesthesiology and Perioperative Medicine
Section Editor: Gregory J. Crosby
Cerebral Oxygen Desaturation Events Assessed byNear-Infrared Spectroscopy During Shoulder Arthroscopyin the Beach Chair and Lateral Decubitus Positions
Glenn S. Murphy, MD,* Joseph W. Szokol, MD,* Jesse H. Marymont, MD,* Steven B. Greenberg, MD,*Michael J. Avram, PhD,† Jeffery S. Vender, MD,* Jessica Vaughn, BA,* and Margarita Nisman, BA*
BACKGROUND: Patients undergoing shoulder surgery in the beach chair position (BCP) may beat risk for adverse neurologic events due to cerebral ischemia. In this investigation, we soughtto determine the incidence of cerebral desaturation events (CDEs) during shoulder arthroscopyin the BCP or lateral decubitus position (LDP).
METHODS: Data were collected on 124 patients undergoing elective shoulder arthroscopy in theBCP (61 subjects) or LDP (63 subjects). Anesthetic management was standardized in allpatients. Regional cerebral tissue oxygen saturation (SctO ) was quantified using near-infrared
spectroscopy. Baseline heart rate, mean arterial blood pressure, arterial oxygen saturation, andSctO were measured before patient positioning and then every 3 minutes for the duration of the
surgical procedure. SctO
values below a critical threshold (ⱖ20% decrease from baseline or
absolute value ⱕ55% for ⬎15 seconds) were defined as a CDE and treated using apredetermined protocol. The number of CDEs and types of intervention used to treat low SctO2values were recorded. The association between intraoperative CDEs and impaired postoperativerecovery was also assessed.
RESULTS: Anesthetic management was similar in the BCP and LDP groups, with the exceptionof more interscalene blocks in the LDP group. Intraoperative hemodynamic variables did notdiffer between groups. SctO values were lower in the BCP group throughout the intraoperative
period (P ⬍ 0.0001). The incidence of CDEs was higher in the BCP group (80.3% vs 0% LDPgroup), as was the median number of CDEs per subject (4, range 0 –38 vs 0, range 0 – 0 LDPgroup, all P ⬍ 0.0001). Among all study patients without interscalene blocks, a higher incidenceof nausea (50.0% vs 6.7%, P ⫽ 0.0001) and vomiting (27.3% vs 3.3%, P ⫽ 0.011) was observedin subjects with intraoperative CDEs compared with subjects without CDEs.
CONCLUSIONS: Shoulder surgery in the BCP is associated with significant reductions in cerebraloxygenation compared with values obtained in the LDP. (Anesth Analg 2010;111:496 –505)
The beach chair position (BCP) has been used for position.3Althoughthesafetyoforthopedicsurgeryinthis
shoulder arthroscopic procedures since the early
position has been well established,4 rare catastrophic neu-
1980s. The advantages of the conventional BCP
rologic events have been reported. Pohl and Cullen5 re-
(45°–90° above the horizontal plane) include lack of bra-
ported 4 cases of ischemic brain and spinal cord injury
chial plexus strain, a reduced risk of direct neurovascular
occurring after surgery in the BCP. In an additional report,
trauma compared with the lateral decubitus approach,
visual loss and ophthalmoplegia were described after
excellent intraarticular visualization, and ease of conver-
shoulder surgery in a sitting position.6 Eight intraoperative
sion to an open approach if needed.1,2 In the United States,
cerebrovascular events were reported in a survey of the
approximately two-thirds of arthroscopic and open shoul-
American Shoulder and Elbow Surgeons Society; all events
der procedures are performed with the patient in the sitting
occurred during surgery in the BCP.3
The etiology of central nervous system injury after shoul-
der surgery in the BCP has not been established definitively.
From the *Department of Anesthesiology, NorthShore University Health-System, University of Chicago Pritzker School of Medicine, Evanston; and
Several authors have hypothesized that cerebral ischemia
†Department of Anesthesiology, Northwestern University Feinberg School
may occur when anesthetized patients are placed in a 45° to
of Medicine, Chicago, Illinois.
90° sitting position.5,7 In awake volunteers, sympathetic ner-
Accepted for publication March 29, 2010.
vous system activation occurs when assuming a sitting posi-
Supported by institutional and/or departmental sources (Department ofAnesthesiology, NorthShore University HealthSystem). FORE-SIGHT cere-
tion; systemic vascular resistance and heart rate (HR) are
bral oximetry probes were provided to the department at cost for the project
increased to maintain mean arterial blood pressure (MAP)
by CAS Medical Systems, Inc., Branford, CT.
and cardiac output.8–10 In anesthetized patients, however, the
Address correspondence and reprint requests to Glenn S. Murphy, MD,Department of Anesthesiology, NorthShore University HealthSystem, Uni-
response of the autonomic nervous system is attenuated by
versity of Chicago Pritzker School of Medicine, 2650 Ridge Ave., Evanston,
the vasodilating effects of IV and volatile anesthetics. Signifi-
IL 60201. Address e-mail to [email protected].
cant decreases in cardiac output, MAP, and cerebral perfusion
Copyright 2010 International Anesthesia Research SocietyDOI: 10.1213/ANE.0b013e3181e33bd9
pressure (CPP) have been observed in neurosurgical patients
August 2010 • Volume 111 • Number 2

when position was changed from supine to sitting.11,12 Pro-
BIS values between 40 and 60. In addition, patients received 1
longed reductions in systemic pressures and CPP that exceed
to 2 g 䡠 kg⫺1 䡠 h⫺1 fentanyl throughout the surgical proce-
critical thresholds (severity and time) may result in perma-
dure. If required, rocuronium (10-mg boluses) was adminis-
nent neurologic injury.
tered to maintain a train-of-four count of 2 to 3. Ventilation
Near-infrared spectroscopy (NIRS) is a noninvasive tech-
was controlled to maintain end-tidal carbon dioxide (Etco2)
nology that provides continuous monitoring of regional cere-
between 30 and 34 mm Hg. Lower body forced-air warming
bral tissue oxygen saturation (Scto
devices (Bair Hugger威; Augustine Medical, Minneapolis,
2). NIRS technology allows
for the immediate recognition and treatment of cerebral
MN) were used to maintain core temperature above
desaturation events (CDEs) that would otherwise be undetec-
35.0°C. Ondansetron 4 mg was given to all patients
ted with conventional intraoperative monitoring. NIRS has
within 30 minutes of tracheal extubation. Neostigmine 50
been used to assess the incidence of CDEs in patients under-
g/kg and glycopyrrolate 10 g/kg were administered
going procedures at high risk for adverse neurologic
at a train-of-four count of at least 2 to reverse neuromus-
outcomes (cardiac, vascular, liver transplant, and major ab-
cular blockade at the conclusion of surgical closure.
dominal surgery).13 Although orthopedic patients in the BCP
Clinicians were instructed to maintain MAP within 20% of
are at risk for cerebral hypoperfusion, no previous clinical
baseline values throughout the intraoperative period, as per
trials have assessed changes in Scto
standard practice involving surgery in the sitting position at
2 in this patient popula-
tion. The aim of this prospective cohort study was to deter-
our institution. Baseline MAP was determined in the sedated
mine the incidence of CDEs in the BCP and compare this
patient in the supine position. MAPs below this threshold
cohort to subjects undergoing shoulder surgery in the lateral
were treated with phenylephrine (80 g), ephedrine (5 mg), or
decubitus position (LDP). In addition, the relationship be-
a fluid bolus, as required clinically. Patients undergoing
tween CDEs and early clinical recovery was examined.
surgery in the LDP were treated with the same MAP protocol.
Cerebral Oxygenation Measurements and
Patients and Anesthesia
Perioperative Data Collection
This study was approved by the IRB of NorthShore Uni-
Cerebral oxygen saturation was measured continuously
versity HealthSystem and written informed consent was
using the FORE-SIGHT system (CAS Medical Systems, Inc.,
obtained from all subjects. Seventy consecutive patients
Branford, CT). The FORE-SIGHT device is a continuous
scheduled to undergo elective arthroscopic shoulder sur-
wave, spatially resolved cerebral oximeter that uses 4
gery under general anesthesia in the BCP were enrolled
discrete wavelengths of laser light to calculate the absolute
(BCP group). During this same time period, 70 additional
value of Scto2. Four wavelengths of light allow for more
consecutive patients presenting for the same surgical pro-
accurate determination of oxyhemoglobin and deoxyhemo-
cedure in the right or left LDP were enrolled (LDP group).
globin levels by compensating for wavelength-dependent
Exclusion criteria included preexisting cerebrovascular
scattering losses and reducing interference from other
disease or orthostatic hypotension; age ⬍18 years; ASA
background light absorbers.17,18 Sensors were applied bi-
physical status IV or V; or anticipated procedure under
laterally to each frontotemporal area after cleansing the
interscalene blockade with monitored anesthesia care as the
skin area with alcohol (the medial margin at the midline of
primary anesthetic. Allocation into the BCP and LDP
the forehead [avoiding the temporalis muscle] and the
groups was determined by surgical preference, and use of
lower margin 1–1.5 cm above the eyebrow). The cerebral
interscalene blocks in each group was also primarily influ-
oximetry and BIS probes were secured in the preoperative
enced by surgeon preference. Anesthesia care was admin-
holding area and covered with an opaque wrapping to
istered to the BCP and LDP groups by the same group of
prevent light interference.
providers (15 anesthesiologists).
On arrival to the operating room, MAP and HR were
Cerebral oximetry values may be affected by depth of
recorded. Simultaneously, arterial oxygen saturation (Spo2)
anesthesia, type of anesthetic administered, arterial carbon
and Scto2 values were measured in patients before induc-
dioxide concentrations, inspired oxygen content, and sys-
tion of anesthesia while breathing a 50% air/oxygen mix-
temic blood pressure management.14–16 Therefore, anes-
ture. These variables (Scto2, MAP, HR, and Spo2) were then
thetic management was carefully standardized in subjects
manually recorded by a research assistant every 3 minutes
in both cohorts. Patients received midazolam 2 mg IV
for the duration of the operative procedure. Intraoperative
before being transported to the operating room. Intraopera-
Scto2 data were also collected continuously on a USB
tive monitoring consisted of electrocardiography, auto-
device. Baseline Scto2 was the mean value observed over a
matic arterial blood pressure assessment using a cuff
1-minute period after induction of anesthesia during a
placed on the nonoperative upper extremity, pulse oxim-
stable interval (MAP within 20% baseline values, BIS
etry, capnography, bispectral index monitoring (BIS威
40 – 60, Etco2 30 –34 mm Hg, and Fio2 50%) approximately
system; Aspect Medical Systems, Newton, MA), and mea-
10 minutes after induction of anesthesia. Baseline measures
surement of core temperature via an esophageal probe.
for MAP, HR, Spo2, and BIS used in the analysis were also
Anesthesia was induced with propofol 2.0 to 2.5 mg/kg,
recorded at this time. Five minutes after these initial data
fentanyl 100 g, lidocaine 50 mg, and rocuronium 0.6 to 0.8
were collected, the patient was positioned for the surgical
mg/kg. Maintenance of anesthesia consisted of sevoflurane
procedure. In the BCP group, the head was secured in a
1% to 3% in an oxygen/air mixture (fraction of inspired
neutral position to ensure that cerebral venous drainage
was not impaired. The back of the operating room table
of 50%). Sevoflurane concentrations were
adjusted to maintain MAP within 20% of baseline values and
was then raised to 80° to 90° above the horizontal plane. In
August 2010 • Volume 111 • Number 2
Cerebral Desaturation in the Beach Chair Position
the LDP group, patients were placed in the LDP with the
Discrete data were compared using Fisher exact test
head supported with towels to maintained alignment with
(NCSS, Kaysville, UT). The 95% confidence intervals for the
the thoracolumbar spine. The NIRS monitor was positioned
differences in percentages were calculated using the Far-
rington and Manning score. Ordinal data and continuous
2 data could be viewed by the research assistant
but not by clinicians providing intraoperative care. If any
data that were not normally distributed are presented as
median and range. These data were compared between
2 values below a previously defined critical threshold
(ⱖ20% decrease from baseline or absolute value ⱕ55% for
groups using the Mann-Whitney U test and within groups
⬎15 seconds) were observed by the research assistant,
using Wilcoxon signed rank test (StatsDirect, Cheshire,
clinicians were instructed to treat the CDE. For this investiga-
UK). The median differences and their 95% confidence
tion, a prioritized intraoperative management protocol was
intervals were calculated.
used to increase Scto
Normally distributed continuous data are presented as
2 values. Interventions to treat CDEs
included the following: (1) increasing MAP with phenyleph-
mean and SD. These data were compared using the un-
rine (80 g), ephedrine (5 mg), or a fluid bolus, as clinically
paired t test (NCSS), except for the hemodynamic data.
indicated; (2) increasing Etco
Mean differences and their 95% confidence intervals were
2 by decreasing ventilation; or (3)
calculated. Hemodynamic, Spo
2 concentrations. The number and type of
2, BIS, and Scto2 data were
interventions used to treat low Scto
compared within and between groups using a 2-factor
2 values were recorded by
the research assistant. In addition, interventions used by
analysis of variance with repeated measures on 1 factor,
clinicians to treat MAP reductions unrelated to Scto
with the Holm-Sidak method for pairwise multiple com-
noted. All data were collected until tracheal extubation.
parisons in post hoc analysis (SigmaPlot 11.0; Systat Soft-
After discontinuation of sevoflurane at the end of the
ware, Inc., San Jose, CA).
surgical procedure, the time required to achieve the following
Multiple logistic regression analysis (StatsDirect) was
end points were recorded: open eyes on verbal command;
performed to determine predictors of nausea. Variables
squeeze hand on verbal command; tracheal extubation; and
included in the initial analysis were those identified in
admission to postanesthesia care unit (PACU). The Aldrete
univariate analyses as having a value of P ⬍ 0.10. In the
score was recorded on arrival to the PACU and then assessed
final analyses, variables with high P values were removed
every 15 minutes until discharge. Hydromorphone was used
from the model 1 at a time and were excluded from the
for postoperative analgesia and titrated to achieve pain scores
final model if their removal either did not diminish the fit
of ⬍2 on a scale of 0 to 10 (0 ⫽ no pain, 10 ⫽ worst pain
of the model or actually improved it, as determined by the
imaginable). Any episodes of nausea and vomiting during the
correct prediction of both positive and reference responses.
PACU admission were noted, and the severity of events
The sensitivity and specificity of the logistic model were
graded on a 3-point scale (1 ⫽ mild, 1 episode; 2 ⫽ moderate,
calculated from the model-predicted reference and model-
2–3 episodes; and 3 ⫽ severe, ⬎3 episodes). The need for
predicted positive responses (using the default threshold
rescue antiemetics was also assessed. The times needed to
probability for positive classification of 0.5) and the actual
meet discharge criteria and achieve actual discharge were
reference and actual positive responses. No external vali-
noted. All recovery data were collected by PACU nurses
dation was attempted.
blinded to intraoperative cerebral oximetry information.
The criterion for rejection of the null hypothesis estab-
However, PACU nurses and research assistants were not
lished a priori was a 2-tailed P ⬍ 0.05.
blinded to patient positioning.
Patient demographic data that were recorded included
age, sex, height, weight, preoperative hemoglobin, ASA
One hundred forty patients were enrolled in this clinical trial.
physical status, and preexisting medical conditions. Details
Sixteen subjects were excluded from final analysis because of
of the intraoperative anesthetic management included du-
the following factors: changes in patient positioning (45°
ration of anesthesia, administration of crystalloids, doses of
beach chair) (4 in BCP group); protocol violations (3 in BCP
opioids and rocuronium provided intraoperatively, and
group and 3 in LDP group); incomplete data collection (2 in
core temperatures at the conclusion of the anesthetic.
BCP group and 3 in LDP group); and procedure canceledbefore entering the operating room (1 in LDP group). As a
Statistical Analysis
result, data analysis was performed on 61 patients in the BCP
Sample size was determined based on the primary outcome
group and 63 patients in the LDP group. The BCP and LDP
variable, the incidence of CDEs. Scto
groups were similar in terms of demographic characteristics.
predetermined critical threshold (ⱖ20% decrease from
There were no differences between groups in age, weight,
baseline or absolute value ⱕ55% for ⬎15 seconds) were
height, sex, preoperative hemoglobin values, preexisting
used to define these events. In a pilot study of patients
medical conditions, or ASA physical status (Table 1). Intraop-
undergoing surgery in the BCP, CDEs were observed in
erative management data are presented in Table 2. The
50% of the subjects. We hypothesized that we would
duration of anesthesia was longer in the LDP group. A higher
observe 50% fewer CDEs in patients having surgery in the
percentage of patients in the LDP group received interscalene
LDP. Group sample sizes of 66 in each group achieve 80%
blocks (71.4%) compared with the BCP group (8.2%, P ⬍
power to detect a difference of 0.25 between the null
0.0001) and a lower dose of intraoperative fentanyl was used
hypothesis that both group proportions are 0.50 and the
in the LDP group (P ⬍ 0.0001).
alternative hypothesis that the proportion of the LDP group
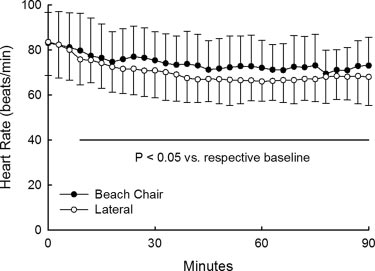
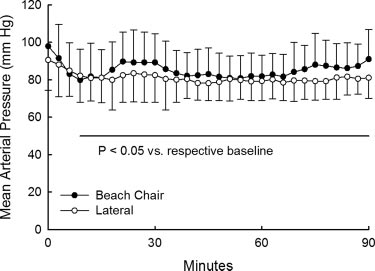
Hemodynamic data are presented in Figures 1 and 2.
is 0.25 with a 2-tailed significance level (␣) of 0.05 using 2
The ANOVA statistics revealed that whereas HR and MAP
or Fisher exact test with continuity correction.
decreased in both the LDP and BCP groups after induction
ANESTHESIA & ANALGESIA

Table 1. Patient Characteristics
Beach chair group
Difference (95% CI)
Sex (male/female)
38 (62.3%)/23 (37.7%)
40 (63.5%)/23 (36.5%)
⫺1.2% (⫺18.0% to 15.6%)
1.9 (⫺3.2 to 7.1)
⫺3.8 (⫺10.5 to 3.0)
⫺3.1 (⫺6.8 to 0.6)
ASA physical status
Hemoglobin (g/dL)
14.0 ⫾ 1.5a
13.9 ⫾ 1.4b
0.1 (⫺0.5 to 0.6)
1.7% (⫺5.5% to 9.8%)
⫺3.1% (⫺11.7% to 4.5%)
6.1% (⫺11.0% to 22.9%)
⫺1.6% (⫺8.5% to 4.4%)
5.2% (⫺6.7% to 17.6%)
1.9% (⫺8.2% to 12.4%)
⫺3.0% (⫺13.1% to 6.6%)
⫺4.6% (⫺15.1% to 5.3%)
⫺1.2% (⫺13.3% to 10.9%)
⫺6.1% (⫺17.5% to 4.8%)
CI ⫽ confidence interval; MI ⫽ myocardial infarction; COPD ⫽ chronic obstructive pulmonary disease; CVA ⫽ cerebrovascular accident; TIA ⫽ transient ischemicattack.
Data are mean ⫾ SD, median (range), or number of patients (%).
a n ⫽ 60.
b n ⫽ 52.
Table 2. Perioperative Variables
Beach chair group
Difference (95% CI)
Interscalene block
⫺63.2% (⫺74.6% to ⫺48.5%)
⫺18.0 (⫺32 to 4)
Dose fentanyl (g)
Dose rocuronium (mg)
⫺0.09 (⫺0.23 to 0.05)
Final OR temperature (°C)
⫺0.1 (⫺0.4 to 0.1)
Times to recovery landmarks (min)
Tracheal extubation
PACUAldrete scores
8 (2–10)a
9 (2–10)a
9 (8–10)b
10 (8–10)c
10 (8–10)d
10 (8–10)e
9 (8–10)f
10 (9–10)g
31.3% (17.1%–45.1%)
Nausea severity (1–3 scale)
1.5 (1–3)h
1 (1–2)i
19.7% (9.8%–31.8%)
Vomiting severity (1–3 scale)
1 (1–2)j
33 (52.4%)a
32.9% (17.0%–47.3%)
Pain medication dose (mg hydromorphone)
1.5 (0.5–4)l
1 (0.5–4.0)m
PACU discharge (min)
83.5 (39–145)a
⫺1 (⫺13 to 10)
94 (55–181)a
CI ⫽ confidence interval; OR ⫽ operating room; PACU ⫽ postanesthesia care unit.
Data are mean ⫾ SD, median (range), or number of patients (%).
a n ⫽ 62, b n ⫽ 58, c n ⫽ 57, d n ⫽ 18, e n ⫽ 27, f n ⫽ 9, g n ⫽ 4, h n ⫽ 24, i n ⫽ 5, j n ⫽ 13, k n ⫽ 1, l n ⫽ 52, m n ⫽ 33.
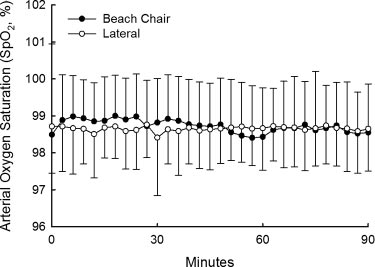
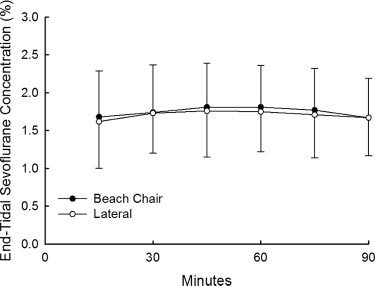
of anesthesia, intraoperative HR and MAP values did not
Scto2 data are presented in Figure 6 and Table 3. Scto2
differ between groups. No differences between groups
values before (75.5 ⫾ 4.0 vs 75.9 ⫾ 3.9) and after (baseline:
were noted in Spo
80.4 ⫾ 5.0 vs 81.1 ⫾ 5.1) induction of anesthesia were
2 (Fig. 3), end-tidal sevoflurane concen-
tration (Fig. 4), or BIS (Fig. 5) data throughout the intraop-
similar between the LDP and BCP groups. The ANOVA
erative period.
statistics revealed that Scto2 not only decreased over time
August 2010 • Volume 111 • Number 2

Cerebral Desaturation in the Beach Chair Position
Figure 1. Heart rate (bpm) for the patients in the beach chair position
Figure 3. Arterial oxygen saturation (SpO , %) for the patients in the
group and in the lateral decubitus position group. The data are
beach chair position group and in the lateral decubitus position
presented as mean ⫾ SD. The horizontal line indicates the time
group. The data are presented as mean ⫾ SD. There were no
during which the heart rates in the patients of the 2 groups differed
differences between the groups at any time. The number of patients
from their baseline heart rates (9 –90 minutes, overall P ⬍ 0.05).
in the beach chair position group decreased from 61 at baseline to
There were no differences between the groups at any time. The
60 at 45 minutes and then progressively over time to 51 at 1 hour
number of patients in the beach chair position group decreased from
and to 20 at 90 minutes, whereas the number of patients in the
61 at baseline to 60 at 45 minutes and then progressively over time
lateral decubitus position group decreased from 63 at baseline to 61
to 50 at 1 hour and to 20 at 90 minutes, whereas the number of
at 48 minutes and then progressively over time to 54 at 1 hour and
patients in the lateral decubitus position group decreased from 63 at
to 40 at 90 minutes.
baseline to 61 at 48 minutes and then progressively over time to 54at 1 hour and to 40 at 90 minutes.
Figure 4. End-tidal sevoflurane concentrations for the patients in thebeach chair position group and in the lateral decubitus position
Figure 2. Mean arterial pressure (mm Hg) for the patients in the
group. The data are presented as mean ⫾ SD. There were no
beach chair position group and in the lateral decubitus position
differences between the groups at any time. The number of patients
group. The data are presented as mean ⫾ SD. The horizontal line
in the beach chair position group decreased from 61 at 15 minutes
indicates the time during which the blood pressures in the patients
to 60 at 45 minutes, to 58 at 60 minutes, to 45 at 75 minutes, and
of the 2 groups differed from their baseline blood pressures (6 –90
to 25 at 90 minutes, whereas the number of patients in the lateral
minutes, overall P ⬍ 0.05). There were no differences between the
decubitus position group decreased from 63 at 15 minutes to 58 at
groups at any time. The number of patients in the beach chair
45 minutes, to 55 at 60 minutes, to 49 at 75 minutes, and to 43 at
position group decreased from 61 at baseline to 60 at 45 minutes
and then progressively over time to 51 at 1 hour and to 20 at 90minutes, whereas the number of patients in the lateral decubitusposition group decreased from 63 at baseline to 61 at 48 minutesand then progressively over time to 54 at 1 hour and to 40 at 90
in the BCP group). Nine of the episodes resolved within 1
minute of treatment. The duration of the episodes rangedfrom 30 seconds to 9 minutes.
but also was lower in the BCP group than the LDP group
Recovery data are presented in Table 2. Lower doses of
across time (P ⬍ 0.0001). The percentage of patients devel-
opioids were used in the LDP group in the operating room
oping a CDE was higher in the BCP group (80.3%) com-
and PACU, which was likely attributable to the higher use
pared with the LDP group (0%, P ⬍ 0.0001). In addition, the
of interscalene blocks in this group. The incidence of nausea
median number of CDEs was greater in the BCP group:
and vomiting was also lower in this group. The time from
ⱖ20% decreases in Scto
the end of the procedure to PACU admission was shorter,
2 from baseline (4 [0 –38] BCP; 0
[0 – 0] LDP; P ⬍ 0.0001) and Scto ⱕ
and early Aldrete scores were higher, in the LDP group. All
55% (0 [0 – 4] BCP; 0
[0 – 0] LDP; P ⫽ 0.003). Furthermore, the median number of
other immediate and early recovery variables were similar
interventions required to treat CDEs was also greater in the
between groups.
BCP group (2 [0 –11] BCP; 0 [0 – 0] LDP; P ⬍ 0.0001). Scto
Further analysis was performed to determine the impact
values increased after initial treatment interventions in 61%
of intraoperative CDEs on postoperative recovery (Tables 4
of patients, with most responses occurring within 30 to 45
and 5). Data were analyzed only on subjects who did not
seconds. Eight patients had 12 episodes of Scto ⱕ
receive interscalene blocks because use of this technique
ANESTHESIA & ANALGESIA
was not equally distributed between the BCP and LDPgroups and interscalene blocks can beneficially influencerecovery from anesthesia. Patient characteristics did notdiffer between subjects with and without CDEs. Perioper-ative management variables, including opioid dosing in theoperating room and PACU, also did not differ betweengroups. A significantly higher incidence of nausea (50.0%vs 6.7%, P ⫽ 0.0001) and vomiting (27.3% vs 3.3%, P ⫽0.011) was observed in subjects with intraoperative CDEscompared with subjects with no CDE. All other recoverylandmarks (with the exception of Aldrete scores on PACUadmission) did not differ between groups.
To determine whether confounding variables may be
Figure 5. Bispectral index (BIS) for the patients in the beach chair
contributing to the nausea, age, sex, smoking status, hemo-
position group and in the lateral decubitus position group. The dataare presented as mean ⫾ SD. There were no differences between
globin concentration, operative position, fentanyl dose,
the groups at any time. The number of patients in the beach chair
end-tidal sevoflurane concentration, and the occurrence of
position group increased from 57 at baseline to 59 at 6 minutes,
cerebral desaturation were compared between patients
then decreased to 58 at 45 minutes after which it decreased
who had not had regional anesthesia and did not become
progressively over time to 49 at 1 hour and to 18 at 90 minutes,whereas the number of patients in the lateral decubitus position
nauseated and patients who had not had regional anesthe-
group decreased from 63 at baseline to 61 at 48 minutes and then
sia but did become nauseated. Variables identified in the
progressively over time to 54 at 1 hour and to 40 at 90 minutes.
univariate analyses as having a value of P ⬍ 0.10 andincluded in the initial multiple logistic regression analysisas predictors of nausea were hemoglobin concentration,operative position, and the occurrence of cerebral desatu-ration. The only variable included in the final multiplelogistic regression model as a predictor of nausea was theoccurrence of cerebral desaturation (logit P ⫽ ⫺2.639 ⫹2.639 ⫻ [0 ⫽ no desaturation, 1 ⫽ desaturation]; likelihoodratio test statistic ⫽ 17.56, df ⫽ 1, P ⬍ 0.0001). Thesensitivity of the logistic model was 91.7%, whereas itsspecificity was 56.0%.
DISCUSSIONPatients undergoing shoulder surgery in the BCP may be at
Figure 6. Regional cerebral tissue oxygen saturation (SctO ) for the
risk for cerebral hypoxia because of decreases in CPP. NIRS
patients in the beach chair position group and in the lateral
technology, which provides information on the balance
decubitus position group. The data are presented as mean ⫾ SD.
The solid horizontal line indicates the time during which the SctO
between oxygen supply and demand in the frontal region
values in the patients of the beach chair position group differed from
of the brain, has not been used previously to determine
their baseline SctO values (3– 0 minutes, overall P ⬍ 0.05) whereas
changes in Scto2 in this patient population. Our results
the dotted horizontal line indicates the time during which the SctO2
indicate that CDEs, defined as a ⱖ20% decrease in Scto2
values in the patients of the lateral decubitus position group differedfrom their baseline SctO values (12– 0 minutes, overall P
values from baseline measurements or an Scto
The dashed horizontal line indicates the times during which the SctO2
ⱕ55%, occurred frequently in patients having arthroscopic
values in the patients of the beach chair position group differed from
surgery in the BCP. Despite the use of a protocol designed
those in the lateral decubitus position group (3–90 minutes, overall
to optimize CPP, CDEs were observed in 80.3% of subjects.
P ⬍ 0.05). The number of patients in the beach chair position group
In contrast, no CDEs were noted in a similar cohort of
decreased from 61 at baseline to 60 at 45 minutes and thenprogressively over time to 51 at 1 hour and to 20 at 90 minutes,
patients undergoing shoulder arthroscopy in the LDP. An
whereas the number of patients in the lateral decubitus position
association between intraoperative CDEs and postopera-
group decreased from 63 at baseline to 61 at 48 minutes and then
tive nausea and vomiting was also observed.
progressively over time to 54 at 1 hour and to 40 at 90 minutes.
Table 3. Primary Outcome Variables
Difference or median
Beach chair group
difference (95% CI)
Patients with cerebral desaturation events
80.3% (68.7%–88.4%)
Interventions for SctO decreases
Interventions for MAP decreases
Episodes SctO ⱕ55
Episodes ⱖ20% decrease SctO
CI ⫽ confidence interval; SctO ⫽ regional cerebral tissue oxygen saturation; MAP ⫽ mean arterial blood pressure.
Data are number of patients (%) or median (range).
August 2010 • Volume 111 • Number 2
Cerebral Desaturation in the Beach Chair Position
Table 4. Patient Characteristics
No interscalene block, no cerebral
No interscalene block, cerebral
desaturation events group
desaturation events group
Difference (95% CI)
Sex (male/female)
18 (60.0%)/12 (40.0%)
28 (63.6%)/16 (36.4%)
⫺3.6% (⫺25.9% to 18.2%)
1.7 (⫺4.8 to 8.2)
3.9 (⫺5.8 to 13.6)
2.4 (⫺2.4 to 7.2)
ASA physical status
Hemoglobin (g/dL)
13.8 ⫾ 1.4a
13.8 ⫾ 1.6b
⫺0.1 (⫺0.8 to 0.7)
6.7% (⫺1.7% to 21.3%)
1.1% (⫺8.9% to 14.6%)
⫺4.2% (⫺25.7% to 18.4%)
3.3% (⫺4.9% to 16.7%)
3.0% (⫺13.3% to 21.8%)
4.2% (⫺10.4% to 21.8%)
⫺6.8% (⫺18.2% to 4.9%)
⫺0.2% (⫺12.8% to 15.3%)
8.8% (⫺4.3% to 25.8%)
12.1% (⫺1.6% to 29.7%)
CI ⫽ confidence interval; MI ⫽ myocardial infarction; COPD ⫽ chronic obstructive pulmonary disease; CVA ⫽ cerebrovascular accident; TIA ⫽ transient ischemicattack.
Data are mean ⫾ SD, median (range), or number of patients (%).
a n ⫽ 29.
b n ⫽ 43.
Table 5. Perioperative Variables
No interscalene block, no
No interscalene block,
cerebral desaturation
cerebral desaturation
Difference (95% CI)
60.0% (74.1%–90.6%)
10 (⫺7.8 to 27.4)
Dose fentanyl (g)
Dose rocuronium (mg)
0.13 (⫺0.07 to 0.33)
Final OR temperature (°C)
⫺0.2 (⫺0.5 to 0.1)
Times to recovery landmarks (min)
Tracheal extubation
PACUAldrete scores
10 (8–10)a
9 (8–10)b
9 (9–10)c
10 (8–10)d
9.5 (9–10)e
9 (8–10)f
⫺43.3% (⫺59.1% to ⫺24.0%)
Nausea severity (1–3 scale)
1.5 (1–3)h
⫺23.9% (⫺39.3% to ⫺7.8%)
Vomiting severity (1–3 scale)
1 (1–2)j
4.7% (⫺11.3% to 18.6%)
Pain medication dose (mg
1.5 (0.5–4.0)k
1.5 (0.5–4.0)l
PACU discharge (min)
2.5 (⫺12 to 17)
2.5 (⫺12 to 22)
CI ⫽ confidence interval; OR ⫽ operating room; PACU ⫽ postanesthesia care unit.
Data are mean ⫾ SD, median (range), or number of patients (%).
a n ⫽ 29, b n ⫽ 43, c n ⫽ 16, d n ⫽ 12, e n ⫽ 4, f n ⫽ 6, g n ⫽ 2, h n⫽ 22, i n⫽ 1, j n ⫽ 12, k n ⫽ 28, l n ⫽ 39.
ANESTHESIA & ANALGESIA
Alterations in systemic hemodynamics occur when pos-
1.35 cm).5,21 If the average vertical distance between the
tural conditions are changed from supine to sitting. Reduc-
brachial artery measurement site and cerebral oximeter
tions in cardiac output, MAP, and CPP may subsequently
probe was 38 cm (measured in 10 sitting patients), and the
compromise cerebral oxygen delivery. In awake volunteers,
average MAP intraoperatively was 80 mm Hg, a "cor-
assumption of a head-up posture results in a 10% to 15%
rected" MAP value of 51.8 mm Hg at the level of the frontal
increase in HR, a 5- to 10-second decrease in MAP and
cortex is derived. This "corrected" pressure might repre-
systemic vascular resistance followed by a rapid rebound
sent an inadequate CPP in some subjects. Although the
and overshoot (15%– 40%), and a sustained reduction in
lower limit of cerebral autoregulation is generally accepted
thoracic blood volume and cardiac output (15%–30%).8–10
to be a MAP of approximately 50 mm Hg, some studies
Compensatory increases in sympathetic nervous system
have demonstrated that this lower threshold may be as
activation and systemic vascular resistance to maintain
high as 70 to 80 mm Hg in awake, normotensive subjects.22
systemic perfusion pressures are attenuated under general
Consequently, if the "waterfall" theory is correct, mainte-
anesthesia. Raising anesthetized neurosurgical patients
nance of a MAP of 80 mm Hg using a manual blood
from the supine to the sitting position resulted in signifi-
pressure cuff might have represented suboptimal blood
cant reductions in cardiac output, MAP, and CPP, which
pressure management and accounted for the lower Scto2
persisted for up to 30 minutes after positioning.11,12
values in the BCP group.
The influence of alterations in positioning on cerebral
Despite the frequent occurrence of CDEs in patients
oxygenation in anesthetized surgical patients has been
undergoing surgery in the sitting position, no obvious
examined in only 1 previous trial. In these 12 subjects, no
neurologic deficits were observed in this study cohort. This
finding is not unexpected because major adverse cerebro-
2 values were observed in the LDP, but a
small (6%), statistically significant decrease in Scto
vascular events after orthopedic procedures in the BCP
curred after assuming the sitting position.19 However,
have been rarely described in the literature. Only 13 cases
cerebral oximetry data were only collected for 5 minutes
of stroke, coma, or blindness have been reported in this
after each change in position. In the present investigation,
patient population.3,5,6 At the present time, the incidence of
clinically significant reductions in Scto
permanent neurologic events after BCP surgery has not
2 values were absent
when position was altered from supine to right or left
been assessed in a prospective or retrospective investiga-
lateral decubitus; Scto
tion. However, a survey of the membership of the Ameri-
2 remained near baseline measures
throughout the operative procedure. No episodes of CDEs
can Shoulder and Elbow Surgeons yielded an estimated
were recorded in any of the 63 LDP subjects, and no
rate of stroke of 0.00382% to 0.00461% during shoulder
interventions to treat low Scto
surgery, with all events occurring in the BCP.3
2 were required. In contrast,
pronounced reductions in Scto
incidence of adverse neurologic outcomes is likely related
2 were observed in the BCP
to the relatively limited duration of the surgical procedure.
2 decreased from a baseline mean of 80% to
mean values of ⬍70% by 9 minutes, and the mean re-
Severity and duration of ischemia are critical determinants
mained between 66% and 70% throughout the operative
of tissue damage, and viability-time thresholds must be
procedure. The median number of CDEs was significantly
exceeded to produce stroke. In a pig model, low Scto2
higher in the BCP group, despite the use of a similar
values that persisted for ⬍2 hours did not result in neuro-
protocol to maintain MAP. In addition, more interventions
logic injury.23 An analysis of NIRS data from 265 coronary
to treat reductions in Scto
artery bypass graft patients revealed a desaturation-time
2 were required in the BCP group.
These findings suggest that CDEs (as defined in this
threshold of 50 minutes that was associated with cognitive
investigation) occur frequently during sitting position sur-
decline and longer hospital length of stay.24 In the present
gery and that cerebral oxygenation in the frontal cortices
investigation, the duration of CDEs was limited, with no
may potentially be compromised in these patients under-
CDEs exceeding previously defined viability-time thresh-
going general anesthesia.
olds. However, the degree and duration of cerebral isch-
Hemodynamic and systemic oxygenation variables (HR,
emia required to produce overt neurologic symptoms in a
relatively healthy patient population is unknown at the
2) were not different between the BCP and LDP
groups throughout the intraoperative period. HR and MAP
present time. The use of a protocol designed to detect, treat,
decreased from initial values in both groups over time, but
and reduce the duration of CDEs (as used in this study)
were within 20% of baseline measures. MAP is a primary
would likely minimize the risk of obvious neurologic
determinant of CPP and oxygenation, and reductions in
MAP are associated with comparable decreases in
A number of recovery variables were assessed in the
PACU to determine whether CDEs in the operating room
2.15,20 MAP values, measured at the brachial artery, did
not differ between the 2 groups of patients. It is possible,
were associated with impaired early recovery from anes-
however, that MAP measured at the brachial artery may
thesia and surgery. A larger number of patients in the LDP
overestimate the actual pressure at the level of the brain
group received interscalene blocks, per surgeon preference.
when the sitting position is assumed. According to the
The use of regional anesthesia may facilitate recovery from
"open model" or "waterfall" theory, as blood flows verti-
anesthesia and surgery; therefore, we performed an analy-
cally from the heart, there is a reduction in arterial pressure
sis only on subjects not administered regional anesthesia.
directly related to the weight of the column of blood.5,21
The times required to achieve immediate recovery land-
When the sitting position is used, an arithmetic correction
marks (time to open eyes, squeeze hand, tracheal extuba-
of MAPs obtained from other sites is required to determine
tion, and arrive in the PACU) and meet PACU recovery
blood pressure at the level of the brain (1 mm Hg for each
criteria did not differ between patients with and without
August 2010 • Volume 111 • Number 2
Cerebral Desaturation in the Beach Chair Position
CDEs. However, an approximately 7-fold higher incidence
and subsequent Scto2 measures under very different physi-
of both nausea and vomiting was observed in subjects with
ologic conditions (awake versus anesthetized) would make
CDEs. Some authors have suggested that an important
the determination of changes in Scto2 due to alterations in
perioperative cause of nausea and vomiting is anesthetic-
patient positioning extremely difficult. Third, neurocogni-
induced systemic hypotension, which produces a reduction
tive testing to assess the presence or absence of subtle
in cerebral perfusion and oxygenation.25 In patients under-
neurologic dysfunction potentially related to CDEs was not
going prostate resection surgery, spinal anesthesia resulted
performed. In addition, transcranial Doppler, which can be
in decreases in CPP and oxygenation, and an association
used to indirectly measure cerebral blood flow changes
between intraoperative CDEs and nausea at the end of
related to alterations in position, was not used intraopera-
surgery was observed.26 Our findings provide further
tively. Fourth, arterial carbon dioxide levels were not
support for an association between CDEs in the operating
measured (ventilation was determined on the basis of Etco2
room and nausea and vomiting during early recovery.
values). Large inter- and intraindividual variations in arte-
A CDE was defined in this investigation as a ⱖ20%
rial to Etco2 gradients have been reported, and the degree
of this variability may be influenced by patient position-
2 values from baseline measures or an Scto2
of ⱕ55%. At the present time, there is not a universally
ing.39 Finally, cerebral oxygenation data were recorded
accepted threshold used to identify pathological cerebral
using the FORE-SIGHT cerebral oximeter. Another Food
saturation. The threshold for identifying cerebral ischemia
and Drug Administration–approved NIRS device (INVOS;
may be influenced by a number of patient-specific (pres-
Somanetics Corp., Troy, MI) has been used in the majority
ence of cerebrovascular disease, incomplete circle of Willis)
of previous perioperative studies, and there are fewer data
or technology-dependent variables. Because of wide
supporting a beneficial effect of the FORE-SIGHT cerebral
patient-to-patient variability in baseline Scto
oximeter on clinical outcomes. However, a recent volunteer
study has demonstrated that the FORE-SIGHT monitor has
authors recommend monitoring changes from baseline
greater precision with respect to measuring absolute Scto
measurements; a reduction of 15% to 20% from baseline has
than the INVOS monitor.32
been used as a critical threshold in many investigations. In
In conclusion, our findings demonstrate that significant
awake patients undergoing carotid endarterectomy, a 20%
reductions in Scto
2 occur when position is changed from
2 was associated with symptoms of cerebral
supine to sitting in patients undergoing general anesthesia.
ischemia.27 In another group of carotid endarterectomy
These changes occurred despite the use of a protocol
patients, a 15% to 20% decrease in Scto2 was associated
designed to maintain systemic MAP within 20% of baseline
with a 20-fold increase in the odds for developing cerebral
values. Furthermore, intraoperative CDEs were associated
ischemia on electroencephalography.28 In addition, 15% to
with a higher incidence of nausea and vomiting in the
25% decreases in Scto2 have been significantly correlated
PACU. Future larger-scale investigations are required to
with cognitive dysfunction after cardiac surgery,29 longer
define the degree and duration of reduction in Scto
PACU and hospital admissions after abdominal surgery,30
associated with permanent neurologic injury.
and greater release of biochemical markers of brain injuryafter liver transplantation.31 Preclinical studies suggest that
AUTHOR CONTRIBUTIONS
when quantitative NIRS technology is used, absolute Scto2
GSM helped design and conduct the study, analyze the data,
values of ⱕ55% represent cerebral ischemia.18,32 Recent
and write the manuscript. This author has seen the original
studies have demonstrated that FORE-SIGHT– derived val-
study data, reviewed the analysis of the data, approved the
ues below this threshold were associated with adverse
final manuscript, and is the author responsible for archiving
outcomes after cardiac and aortic surgery.29,33
the study files. JWS helped design and conduct the study and
There are several limitations to the present investigation.
write the manuscript. This author approved the final manu-
First, NIRS devices measure saturation in an uncertain mix
script. JHM helped design and conduct the study. This author
of arterial, venous, and capillary compartments. In the
approved the final manuscript. SBG helped conduct the study.
supine position, the venous contribution to cerebral oxim-
This author approved the final manuscript. MJA helped designthe study, analyze the data, and write the manuscript. This
etry predominates, with 70% to 84% of Scto2 values deter-
author has seen the original study data, reviewed the analysis
mined by venous blood.34,35 Changes in body position may
of the data, and approved the final manuscript. JSV helped
alter venous and arterial blood pressure and affect the ratio
design the study. This author approved the final manuscript.
of the compartments in the cerebral circulation.36 There-
JV helped conduct the study. This author approved the final
fore, reductions in Scto2 may not only reflect decreases in
manuscript. MN helped conduct the study. This author has
oxygen supply but also changes in cerebral blood
seen the original study data and approved the final manu-
volumes/compartments. Second, baseline Scto2 values
used to define a clinically significant reduction in cerebraloxygenation were measured after induction of anesthesia,
because we were interested in assessing position-related
GSM received honoraria from CASMED. All other authors
report no conflicts of interest.
under identical anesthetic conditions
(similar Fio2, MAP, Etco2, and BIS values). At the presenttime, there is no consensus on the setting under which
baseline measures should be obtained; previous investiga-
1. Gelber PE, Reina F, Caceres E, Monllau JC. A comparison of
risk between the lateral decubitus and the beach-chair position
tors have collected these data before24,30 and after37,38
when establishing an anteroinferior shoulder portal: a cadav-
induction of anesthesia. We believe that assessing baseline
eric study. Arthroscopy 2007;23:522– 8
ANESTHESIA & ANALGESIA
2. Skyhar MJ, Altchek DW, Warren RF, Wickiewicz TL, O'Brien
24. Slater JP, Guarino T, Stack J, Vinod K, Bustami RT, Brown JM III,
SJ. Shoulder arthroscopy with the patient in the beach-chair
Rodriguez AL, Magovern CJ, Zaubler T, Freundlich K, Parr GV.
position. Arthroscopy 1988;4:256 –9
Cerebral oxygen desaturation predicts cognitive decline and
3. Friedman DJ, Parnes NZ, Zimmer Z, Higgins LD, Warner JJ.
longer hospital stay after cardiac surgery. Ann Thorac Surg
Prevalence of cerebrovascular events during shoulder sur-
gery and association with patient position. Orthopedics
25. Borgeat A, Ekatodramis G, Schenker CA. Postoperative nausea
and vomiting in regional anesthesia: a review. Anesthesiology
4. Weber SC, Abrams JS, Nottage WM. Complications associated
2003;98:530 – 47
with arthroscopic shoulder surgery. Arthroscopy 2002;18:88–95
26. Atallah MM, Hoeft A, El-Ghorouri MA, Hammouda GE, Saied
5. Pohl A, Cullen DJ. Cerebral ischemia during shoulder surgery
MM. Does spinal anesthesia affect cerebral oxygenation during
in the upright position: a case series. J Clin Anesth
transurethral prostatectomy? Reg Anesth Pain Med 1998;
6. Bhatti MT, Enneking FK. Visual loss and ophthalmoplegia
after shoulder surgery. Anesth Analg 2003;96:899 –902
27. Samra SK, Dy EA, Welch K, Dorje P, Zelenock GB, Stanley JC.
7. Papadonikolakis A, Wiesler ER, Olympio MA, Poehling GG.
Evaluation of a cerebral oximeter as a monitor of cerebral
Avoiding catastrophic complications of stroke and death re-
ischemia during carotid endarterectomy. Anesthesiology
lated to shoulder surgery in the sitting position. Arthroscopy
2000;93:964 –70
28. Rigamonti A, Scandroglio M, Minicucci F, Magrin S, Carozzo
8. Smith JJ, Porth CM, Erickson M. Hemodynamic response to the
A, Casati A. A clinical evaluation of near-infrared cerebral
upright posture. J Clin Pharmacol 1994;34:375– 86
oximetry in the awake patient to monitor cerebral perfusion
9. Frey MA, Tomaselli CM, Hoffler WG. Cardiovascular re-
during carotid endarterectomy. J Clin Anesth 2005;17:426 –30
sponses to postural changes: differences with age for women
29. MacLeod D, White W, Ikeda K, Newman M, Mathew J.
and men. J Clin Pharmacol 1994;34:394 – 402
Decreased forebrain cerebral tissue oxygen saturation is asso-
10. Van Lieshout JJ, Wieling W, Karemaker JM, Secher NH.
ciated with cognitive decline after cardiac surgery. Anesth
Syncope, cerebral perfusion, and oxygenation. J Appl Physiol
Analg 2009;108(SCA Suppl):SCA 8
2003;94:833– 48
30. Casati A, Fanelli G, Pietropaoli P, Proietti R, Tufano R, Danelli
11. Smelt WL, de Lange JJ, Booij LH. Cardiorespiratory effects of
G, Fierro G, De Cosmo G, Servillo G. Continuous monitoring of
the sitting position in neurosurgery. Acta Anaesthesiol Belg
cerebral oxygen saturation in elderly patients undergoing
major abdominal surgery minimizes brain exposure to poten-
12. Dalrymple DG, MacGowan SW, MacLeod GF. Cardiorespira-
tial hypoxia. Anesth Analg 2005;101:740 –7
tory effects of the sitting position in neurosurgery. Br J Anaesth
31. Plachky J, Hofer S, Volkmann M, Martin E, Bardenheuer HJ,
1979;51:1079 – 82
Weigand MA. Regional cerebral oxygen saturation is a sensi-
13. Casati A, Spreafico E, Putzu M, Fanelli G. New technology for
tive marker of cerebral hypoperfusion during orthotopic liver
noninvasive brain monitoring: continuous cerebral oximetry.
Minerva Anestesiol 2006;72:605–25
transplantation. Anesth Analg 2004;99:344 –9
14. Fassoulaki A, Kaliontzi H, Petropoulos G, Tsaroucha A. The
32. MacLeod D, Ikeda K, Vacchiano C. Simultaneous comparison
effect of desflurane and sevoflurane on cerebral oximetry
of FORE-SIGHT and INVOS cerebral oximeters to jugular bulb
under steady-state conditions. Anesth Analg 2006;102:
and arterial co-oximetry measurements in healthy volunteers.
Anesth Analg 2009;108(SCA Suppl):SCA 56
15. Chu LC, Hsu YW, Lee TC, Lin YC, Huang CJ, Chen CC, Hung
33. Fischer G, Lin H, DiLuozzo G, Griepp R, Reich D. Decreased
YC. Changes of regional cerebral oxygen saturation during
cerebral tissue oxygen saturation during aortic surgery in-
spinal anesthesia. Acta Anaesthesiol Taiwan 2007;45:155– 62
creases risk of postoperative complications. Anesth Analg
16. Lovell AT, Owen-Reece H, Elwell CE, Smith M, Goldstone JC.
2009;108(SCA Suppl):SCA 54
Continuous measurement of cerebral oxygenation by near
34. Kurth CD, Steven JM, Benaron D, Chance B. Near-infrared
infrared spectroscopy during induction of anesthesia. Anesth
monitoring of the cerebral circulation. J Clin Monit 1993;9:163–70
Analg 1999;88:554 – 8
35. Watzman HM, Kurth CD, Montenegro LM, Rome J, Steven JM,
17. Strangman G, Boas DA, Sutton JP. Non-invasive neuroimaging
Nicolson SC. Arterial and venous contributions to near-
using near-infrared light. Biol Psychiatry 2002;52:679 –93
infrared cerebral oximetry. Anesthesiology 2000;93:947–53
18. Fischer GW. Recent advances in application of cerebral oxim-
36. Pollard V, Prough DS, DeMelo AE, Deyo DJ, Uchida T,
etry in adult cardiovascular surgery. Semin Cardiothorac Vasc
Widman R. The influence of carbon dioxide and body position
Anesth 2008;12:60 –9
on near-infrared spectroscopic assessment of cerebral hemo-
19. Fuchs G, Schwarz G, Kulier A, Litscher G. The influence of
globin oxygen saturation. Anesth Analg 1996;82:278 – 87
positioning on spectroscopic measurements of brain oxygen-
37. Reents W, Muellges W, Franke D, Babin-Ebell J, Elert O.
ation. J Neurosurg Anesthesiol 2000;12:75– 80
Cerebral oxygen saturation assessed by near-infrared spectros-
20. Dunham CM, Sosnowski C, Porter JM, Siegal J, Kohli C.
copy during coronary artery bypass grafting and early post-
Correlation of noninvasive cerebral oximetry with cerebralperfusion in the severe head injured patient: a pilot study.
operative cognitive function. Ann Thorac Surg 2002;74:109 –14
J Trauma 2002;52:40 – 6
38. Kussman BD, Wypij D, DiNardo JA, Newburger JW, Mayer JE
21. Drummond JC, Hargens AR, Patel PM. Hydrostatic gradient is
Jr, del Nido PJ, Bacha EA, Pigula F, McGrath E, Laussen PC.
important: blood pressure should be corrected. APSF Newslett
Cerebral oximetry during infant cardiac surgery: evaluation
and relationship to early postoperative outcome. Anesth Analg
22. Drummond JC. The lower limit of autoregulation: time to
revise our thinking? Anesthesiology 1997;86:1431–3
39. Grenier B, Verche re E, Mesli A, Dubreuil M, Siao D, Vanden-
23. Kurth CD, McCann JC, Wu J, Miles L, Loepke AW. Cerebral
driessche M, Cale s J, Maurette P. Capnography monitoring
oxygen saturation-time threshold for hypoxic-ischemic injury
during neurosurgery: reliability in relation to various intraop-
in piglets. Anesth Analg 2009;108:1268 –77
erative positions. Anesth Analg 1999;88:43– 8
August 2010 • Volume 111 • Number 2
Source: http://tais-med.ru/pdf/Murphy.pdf
erdheim-chester.org
Lightheadness, Kidney issues in 1990's dx'd as multi cystic dysplastic kidney disease, controlled by meds. Chronic sinus Lesions on the brain, mass behind eye, problems. MRI showed masses behind the eyes. Surgery revealed a benign scar tissue type mass. kidney, long bones of leg. 1980's first symptoms were high blood pressure dx'd as renal artery stenosis, profuse perspiration, and itching/burning sensation after a shower. In 1999 had pain in knees, shins, lower back and flank dx'd as age related. In 2001 had night sweats, muscle cramps, anemia dx'd as myelofibrosis. In 2004 had extreme weight loss, extreme fatigue, nausea, numb upper lip, back rash, small, longstanding skin lesion bx'd, congestive heart failure, brain lesions, kidney failure, dialysis, fevers of unknown origin, kidney transplant. After transplant (2005 – 2007) had balance issues, slurred speech, loss of tooth material, Kidney, brain, adrenal gland, heart, lungs,
Catalogo unificato genitorialita' e famiglia
Rassegna bibliografica Genitorialità/Famiglia Genitorialità/Famiglia L'educazione (im)possibile Orientarsi in una società senza padri Vittorino Andreoli Rizzoli Editore, 2014 Numero pagine: 213 Educare oggi, sostiene Andreoli, vuol dire insegnare a vivere in un mondo vastissimo e così mutevole da diventare quasi misterioso. Come fare? Come si può e si deve immaginare l'educazione in una società camaleontica dove tutto si trasforma continuamente, compresi i sentimenti e legami umani (parte indispensabile di ogni processo di crescita)? Da questa domanda parte un grido d'allarme che coinvolge non solo la famiglia e la scuola ma l'intera società, giacché il fallimento educativo è un malessere profondo che riguarda tutti, genitori e no, insegnanti e no, e che può essere risolto solo con uno sforzo comune (in primis ritrovando un punto d'unione con tutte le figure chiamate in causa durante la crescita dei ragazzi e tra loro una costante comunicazione tesa ad evitare la moltiplicazione degli stili educativi). Gli adulti devono capire, sottolinea Andreoli, che i sentimenti e i legami, come anche la possibilità di una progettualità a lunga durata (vale a dire della percezione del futuro da parte degli adolescenti), devono essere prioritari in quanto veicoli di messaggi che servono a dare sicurezza ed aiutano a formare l'identità del ragazzo: l'internet e i social networks potranno anche offrire agli adolescenti stimoli ed emozioni maggiori, ma senza ricchezza e benefici dei legami affettivi "reali". Il saggio ha un forte carattere divulgativo e cerca di dare risposte esaurienti a varie problematiche adolescenziali mettendo al centro di tutto la famiglia e la sua funzione: non più una somma di Io separati, ma una piccola orchestra diretta dal "bisogno esistenziale dell'uomo e della convivenza tra uomini". Informazioni su autore: Andreoli è considerato uno dei maggiori psichiatri italiani; al grande pubblico è noto in quanto studioso dei meccanismi della mente umana e osservatore del disagio psicologico degli adolescenti e dei loro genitori (argomento al quale ha dedicato, nel corso della sua carriera professionale, numerosi saggi) Altri soggetti: paternità e maternità/aspetti socio-culturali; educazione familiare; ruolo del contesto scolastico; adolescenza; identità