Microsoft word - als_package.revisedfeb2010[1].doc
SOUTH WEST HEALTHCAREWARRNAMBOOL
ADVANCED LIFE SUPPORT
LEARNING PACKAGE
Prepared by:
J. Brown, ICU
Last revised February, 2010.
C. Joseph, Nursing Education.
CONTENTS:
Basic Life Support Choking and airway obstruction Defibrillation in ALS Automated External Defibrillators Temporary external pacing Medications used in ALS Treatment of arrhythmias Correcting reversible causes OBJECTIVES:
1. Demonstrate / describe what constitutes effective BLS:
• Assessment of airway
• Breathing
• Circulation / Compressions
• Demonstrate the above on manikin
2. Give the rationale for early defibrillation, early access to the
emergency response system and early BLS.
3. Recognises those rhythms that require defibrillation and those
that do not.
4. Describe the protocol for the use of a defibrillator in both the
manual and Automated External Defibrillator (AED) mode.
5. Give the rationale for the use of and indications for delivering
either a single shock or a series of 3 rapid stacked shocks.
6. Demonstrate techniques which provide access to appropriate
skin sites for placement / attachment of the defibrillator electrodes
and:
• Describe when it might be necessary to dry the skin • Demonstrate preparation of defibrillator electrodes for attachment to the skin. • Describe the technique to avoid trapping of air between the electrodes and the skin. • Attach the electrodes to the skin at appropriate sites in a manner that facilitates safe and effective defibrillation. 7. Demonstrate electrode placement on either a manikin which
generates an ECG signal, or to a separate ECG signal generator,
including:
• Turning on defibrillator / attaching electrode cable to • The technique for initiating analysis of the ECG signal in the • The technique for charging the defibrillator. • When AED mode in use, deliver first shock when prompted • The delivery of a shock after giving a warning for bystanders • The provision of further shocks and Basic Life Support (BLS) according to SWH protocol and by prompts from the AED, including the prompt that a non-shockable rhythm is present. The participant should demonstrate preparation of AED, attachment of the electrodes to manikins chest etc. in a two minute time frame. The participant must also demonstrate how to operate the AED in the manual mode (Critical Care and Emergency trained staff only).
8. Demonstrate appropriate responses to perfusing and non-
perfusing rhythms on a manikin that generates various rhythms for
interpretation. In the case of the manual biphasic defibrillator, the
participant must demonstrate use, response to rhythms, select
joules, charge, defibrillate and demonstrate use and understanding
of all buttons on the defibrillator.
9. Describe the possible complications of external defibrillation.
10. Describe the safety precautions of defibrillation, including the
importance of the "stand clear" command.
11. Describe the possible problems which may arise during the
use of the defibrillator and how to respond to such problems.
12. Demonstrate a maintenance check of and basic fault finding in
a defibrillator:
• Checking leads for damage. • Turning on the defibrillator to check for potential function. • Checking the presence of paper in the paper drive and that the electronic data collection module is in place. 13. Outline troubleshooting of the defibrillator when there is failure
to discharge or failure to defibrillate.
14. State the steps in the ALS algorithm and the points at which
medications are appropriate.
15. Choose the most appropriate drug or drugs in light of:
• The point that has been reached in the ALS algorithm. • The cardiac rhythm. • The duration of the arrest. • The patient's serum electrolyte levels and acid-base status. • The patient's response to drugs, which have already been • The patient's history and previous medication exposure. • Identify the need to exclude reversible causes and identify
16. State the initial dose of the selected drug, different modes of
administration including the use of minijets, time to onset of
action, likely duration of effect, subsequent doses, maximum
doses, side effects and management of side effects.
BASIC LIFE SUPPORT
Definition:
The preservation and restoration of life by the establishment of and/or maintenance of airway, breathing and circulation and related emergency care.
D - Danger:
• The area should be assessed for any signs of danger for the patient and/or bystanders. Remove the source of danger if possible. R - Response:
• Check the patient for a response, touch and • Call for help, call a Code Blue, dial 33, and
state patient location.
• Note the time of the event. A - Airway:
• Check patency of the airway, look inside the airway for any signs of obstruction, clear or suction the airway if required. • Insert Guedel airway if required, measure from patients ear to lip.
B - Breathing:
• Look, listen and feel for any spontaneous • Perform the head tilt/chin lift (not in infants). • Administer two good breaths with Laerdal bag. Ventilation oxygenates the patient. • Assist Doctors to intubate the patient if required. C - Circulation:
• Check for a carotid pulse, located at the corner of the mouth and half way down the neck. Do not spend more than 10 seconds trying to locate the pulse. • For a witnessed or monitored arrest a precordial thump should be administered. • Attach FR2 automatic defibrillator if on general ward and follow prompts from the machine. • If in ICU, ED or OR attach the HeartStart XL defibrillator. • It is important to continue CPR when the patient has no output, as this helps cellular perfusion and the circulation of drugs. Avoid interruptions to CPR, if interruptions occur, for example ALS interventions, 2 minutes of uninterrupted CPR must be performed before performing any further interventions. • Check for output during CPR by palpating either the carotid or femoral pulse. • Reassess the patient's rhythm and for signs of spontaneous output every 2 minutes. COMPRESSION/VENTILATION RATIOS:
• Adult ratio: 30:2 compressions / ventilations for one or
two operators, aiming for a rate of 100 compressions/ minute. • Paediatric ratio (all ages except newborn): 15:2
compressions / ventilations for one or two operators. • Newborn ratio (first minutes to hours after birth): 3:1
compressions / ventilations for one or two operators, providing a rate of 120 compressions and 40 – 60 breaths /minute. Note the newborn period is the first minutes to hours after birth.
Compression techniques:
• Compress the centre of the patient's chest with the heel of both hands. It is now recommended by the Australian Resuscitation Council (ARC) to use both hands for adults and children except in infants and newborns. • The compression should be 1/3 of the depth of the chest for all patients, which is 4-5cm. • Compressions for infants (<1 year) should be with two For further reading refer to the
SWH Resuscitation Policy, accessed through Clinical
Guidelines on the intranet.
Or visit the Australian Resuscitation Council (ARC) website at
MANAGEMENT OF FOREIGN BODY AIRWAY
OBSTRUCTION - (CHOKING)
A foreign body airway obstruction (FBAO) is a life threatening
emergency. Chest thrusts, back blows or abdominal thrusts are
effective for FBAO in conscious adults and children >1 year of age.
Some injuries have been reported with the use of abdominal
thrusts therefore the ARC no longer recommends the use of lateral
chest thrusts.
Assess Severity
The simplest way to assess the severity of a FBAO is to assess
whether the cough is effective or ineffective.
Effective Cough (mild obstruction):
The victim with an effective cough should be reassured and
encouraged to keep coughing to expel the foreign body.
Ineffective Cough (severe airway obstruction):
Conscious Victim:
• Perform up to 5 sharp back blows with the heel of one hand in the middle of the back between the shoulder blades. • Check to see if each back blow has cleared the obstruction. An infant may be placed in a head down position prior to giving the back blows. • If the back blows are unsuccessful the rescuer should perform 5 chest thrusts, checking to see if each thrust has relieved the obstruction. To perform chest thrusts identify the same compression point as for CPR and give 5 thrusts. The infant should be placed in a head down supine position. If the obstruction is still not relieved continue alternating 5 back blows with 5 chest thrusts.
Unconscious Victim:
• The finger sweep can be used in the unconscious victim with an airway obstruction if the foreign body is visible. A Code Blue should be activated and CPR commenced immediately if the victim is unconscious and the rescuer is unable to remove the foreign body. ADVANCED LIFE SUPPORT
Defibrillation in advance cardiac life support:
Research has shown that early defibrillation in cardiac arrest for
patients presenting with VF and pulseless VT dramatically
increases the chance of survival. A direct current passed through
the patient's chest can produce simultaneous depolarisation of
myocardial cells leading to organised electrical activity. Research
has shown survival decreases by 5.5% per minute without the
initiation of defibrillation, BLS and ALS.
SWH has Philips HeartStart XL defibrillators, located in ICU, Acute
Care, E.D and the Operating Theatre. These can be used in
manual and semi-automatic modes. The remainder of the hospital
has Philips FR2 automatic defibrillators that may also be operated
in manual mode (by Critical Care or Emergency trained SWH
staff). All the defibrillators are bi-phasic meaning the electrical
energy travels back and forth between the adhesive pads. This
reduces the impedence of the chest wall allowing fewer joules to
be used.
Note: The latest ARC Guidelines (2006) recommend that
energy levels for adults should be set at 200J for all shocks,
unless relevant clinical data for a specific defibrillator
suggests that an alternative energy level provides adequate
shock success.
It is recommended by Philips that the HeartStart XL and FR2
defibrillators be set for adults at 150J for all shocks, therefore
SWH protocol stipulates the use of 150J based on these
recommendations.
Procedure for applying defibrillator pads:
• The adhesive pads should be rolled onto the patient's skin to avoid trapping of air. • If the patient's skin is moist then attempt to dry off. • Do not operate the defibrillator if in contact with water. • One pad is placed on the upper right anterior chest wall below the clavicle and the other pad placed on the lower left anterolateral chest wall below the axilla (as illustrated on pads). Pad Placement
• Special care should be taken not to place the pads over the patient's nipples, ECG electrodes, GTN patches, implantable defibrillators or pacemakers. • If ECG electrodes are not connected to the patient, the lead select must be changed to ‘pads' to visualise the patient's rhythm. If ECG leads are connected, change the lead select to whichever lead shows the best waveform, usually lead II. • Ensure that the patient is not in contact with any metal fixtures, eg: bed rails. • Call loudly "stand clear" when shock is to be delivered and
visualise that no person is in contact with the patient before delivering the shock. • Oxygen should be pointed away from the patient to prevent • The adhesive defibrillator pads can deliver up to 50 shocks before they need to be replaced. Troubleshooting failure to defibrillate:
• Are the pads connected to the defibrillator? • If some time has lapsed between the charge and defibrillation, then the defibrillator may have dumped the load. • Is the synchronise button on? The synchronise feature is only used for elective cardioversions. • Have the joules been selected? • Is the defibrillator battery flat? • If all the above is NAD, apply a new set of pads. AUTOMATIC EXTERNAL DEFIBRILLATORS (AED)
AED (FR2) defibrillators are located on all ward emergency trolleys throughout the hospital. The AED is programmed to deliver a shock of 150J. Ward staff are educated to attach the AED in an arrest situation as part of the BLS protocol, and defibrillate if instructed to do so by the FR2. Staff who have completed the ALS competency and are critical care trained are able to override the AED and use it in the manual mode to defibrillate patients if they wish to do so. Otherwise the FR2 should remain in the automatic mode. Refer to the manual or a trainer in your ward or department for instructions on how to operate the AED in the manual mode. The HeartStart XL can be operated in both the manual and AED mode. SWH protocol allows ALS trained staff to choose which mode they will use, however the benefits of using the AED make it the preferred mode to use. The benefits are as follows: In AED mode the defibrillator will analyse the rhythm and advise if a shock is to be delivered. Once the defibrillator has delivered a shock or has advised CPR, the pause button should be pressed to enable the defibrillator to count down two minutes of CPR. The patient's rhythm will automatically be re-analysed once two minutes time has lapsed. TEMPORARY EXTERNAL PACING
The HeartStart XL defibrillators are capable of performing
temporary external (transcutaneous) pacing.
Indications:
• Patients that may require pacing include bradycardias that do not respond to drug therapy, causing haemodynamic compromise or asystole. • External pacing may also be required whilst temporary transvenous pacing is being arranged. There are two available modes of pacing; demand and
fixed.
• In the demand mode the pacer delivers paced pulses
when the patient's heart rate is lower than the set rate. This mode is selected when the patient has some spontaneous beats, eg: heart blocks or bradycardias. • The fixed mode allows the pacer to deliver paced
pulses at a set rate to be used when the patient has no
spontaneous electrical activity. The demand mode is
used whenever possible.
Pacing Procedure:
Step
Place the adhesive pads on the patient's chest using either the anterior/anterior or anterior/posterior placement.
Anterior / anterior:
Anterior / posterior:
Turn Philips HeartStart XL on in manual mode. Apply ECG monitoring electrodes to patient and connect cable to Philips HeartStart XL. Select lead that has most prominent R wave. Apply multifunction pads to clean, dry skin and firmly press down to ensure good contact. Contact pads to cable from Philips HeartStart XL
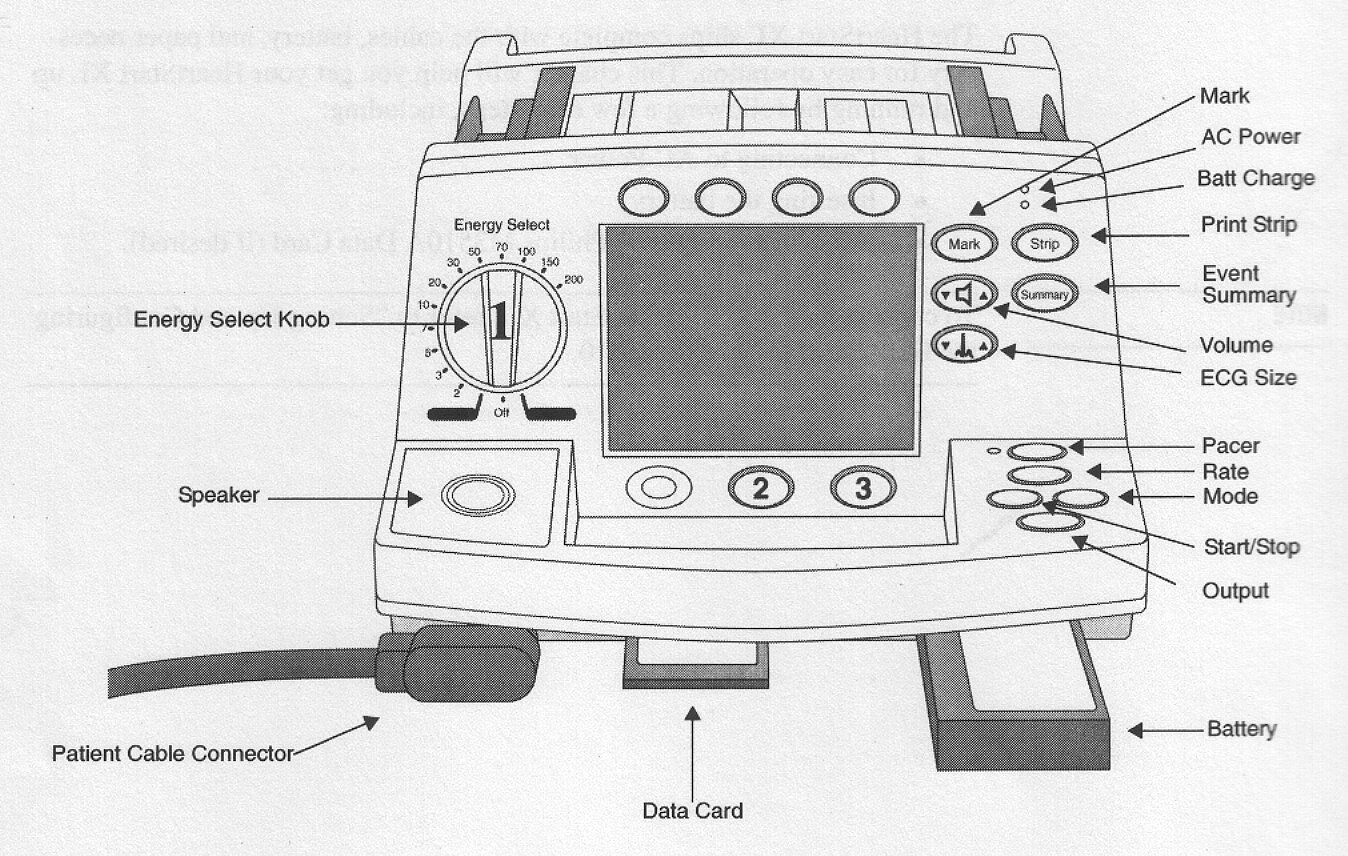
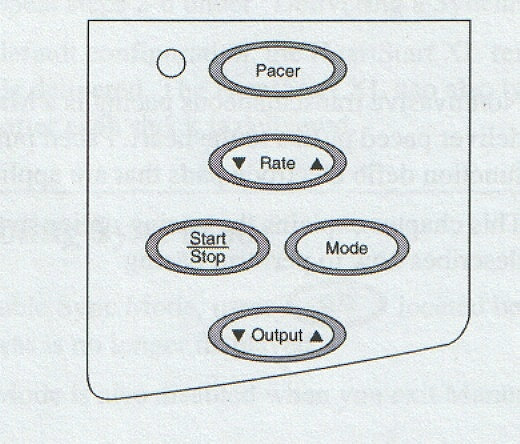
Press "PACER" key to turn pacing mode on
Dot markers should appear in the middle of the QRS complexes if the patient's intrinsic rate is greater than the pacer rate. This signifies that sensing is occurring.on ECG monitoring (see above diagram of pacing dialogue box). If dots are not present, adjust ECG size (amplitude) or select another lead.
Press "MODE" key to change between Demand and Fixed Pacing
Mode. Demand Mode is the preferred mode of pacing.
Press "RATE" key using arrows to set / adjust pacing rate. The Pacer
defaults to a rate of 70 when turned on. Set the rate 10 higher than
the patient's intrinsic rate to check sensing and capture.
Press "OUTPUT" key using arrows to set amount of energy delivered to achieve myocardial capture. The output default setting is 30mA, but can be adjusted between 10 – 200mA. The output should be increased until every beat is capturing (this is the pacing threshold). A wide QRS complex will identify capture. Set the output at 10% greater than the pacing threshold. The least amount of mA should be used.
Press "Start/Stop" button to commence pacing.
Action cont:
Observe for commencement of electrical capture and check that mechanical capture is occurring by palpating patient pulse and ensuring adequate BP.
Document all pacing settings, time pacing commenced, patient cardiac rhythm, BP and peripheral pulses on observation chart and in nursing notes. Perform 12 lead ECG.
Administer ordered analgesia / sedation to promote patient comfort.
• Do not leave patient unattended whilst temporary
transcutaneous cardiac pacing is in progress.
Defibrillation
during external
• If required, defibrillation can be initiated whilst in pacing
o There is no need to switch pacing off
o Charge defibrillator as normal and deliver the
o The pacer will need to be turned on again after
defibrillation to reinitiate pacing (the previous
settings will be restored).
CPR during
external
• CPR can be safely performed without electrical risk to the
operator providing the following precautions are taken:
o Do not place hands over pacing pads
o Wear rubber gloves
• Complications may include micro-shock, skin breakdown,
of external
muscle twitching and pain.
MEDICATIONS USED IN ADVANCED LIFE SUPPORT
IV access:
Administration of medications intravenously is preferable in the
event of cardiac arrest. An intravenous cannula must be inserted
into a large peripheral vein. If there is no visible peripheral access
then the external jugular vein should be considered.
Lower limb veins should be avoided due to lack of venous return.
Intravenous administration of drugs should be followed by a
flush of 30mls of compatible fluid and external cardiac
compressions. A normal saline infusion may be commenced to
aid in flushing of medications.
Minijets:
Minijets of adrenaline, atropine, lignocaine and calcium chloride
are available for use at SWH. If you are unfamiliar with the use of
minijets please see one of the ALS assessors for further
instruction. Expired minijets are available in the education centre
for training.
Endotracheal drug administration:
Endotracheal administration may be considered if intravenous
access cannot be obtained. Adrenaline, atropine and lignocaine
can all be administered via the endotracheal route.
• The ETT must be suctioned prior to administration. • Insert a clean suction catheter down the ETT and instil the
medication via the catheter.
• Administer twice the intravenous dose diluted to 10mls of
normal saline or water.
• This is to be followed by at least two vigorous ventilations. • In the paediatric patient intraosseous administration may
also be considered. The same dose is administered as the intravenous dose.
Nurse-initiated medications for ALS:
Adrenaline, Atropine and Amiodarone are first line
drugs that may be administered during a cardiac
arrest by nurses at SWH, whom have undertaken the
Advanced Life Support education package and been
deemed competent.
MEDICATIONS USED IN ADVANCED LIFE SUPPORT:
Adrenaline (Epinephrine)
A naturally occurring catecholamine with alpha and beta effects,
leading to peripheral vasoconstriction via its alpha-adrenergic
action, directing blood to the myocardium and brain.
Indications:
• Ventricular Fibrillation / pulseless Ventricular Tachycardia
after initial shocks have failed.
• Asystole, pulseless electrical activity (PEA)
Dose:
Initial adult dose is 1mg (1ml of 1:1,000 or 10mls of 1:10,000)
This dose may be repeated every three minutes during CPR. An
infusion of adrenaline may be required after return of circulation.
Adrenaline by infusion should be delivered by a dedicated central
line as soon as possible. Adrenaline must not be mixed with
sodium bicarbonate.
Adverse effects:
• Tachyarrhythmia's • Severe hypertension post resuscitation • Tissue necrosis.
Amiodarone
Amiodarone is an antiarrhythmic drug that has effects on sodium,
potassium and calcium channels. It also has alpha and beta-
adrenergic blocking properties.
Indications:
• First line anti-arrhythmic for failed defibrillation of VT/VF. • Prophylaxis of recurrent VF/VT.
• Initial bolus dose is 300mg diluted to 20mls of 5% dextrose
and administered over 3 minutes. An additional dose of 150mg may be considered. This may be followed by an infusion of 15mg/kg over 24 hours.
Adverse effects: Hypotension, bradycardia and heart block.
Atropine
A parasympathetic antagonist that blocks the action of the vagus
nerve on the heart.
Indications:
• Bradycardia leading to haemodynamic compromise • Asystole.
Dose:
Unconscious patients: 1.0 mg bolus that may be repeated every
3-5 mins, up to a total of 3mg.
Conscious patients: 0.6mg bolus that may be repeated every 3-5
mins, up to a total of 3mg.
Adverse effects: Tachycardia, excitement, delirium, urinary
retention, dilated pupils, hyperthermia in large doses.
MEDICATIONS THAT MAY BE USED IN ADVANCED
LIFE SUPPORT BY ORDER OF A MEDICAL OFFICER:
Lignocaine
An anti-arrhythmic drug acting as a sodium channel blocker.
Indications:
• Second line anti-arrhythmic for failed defibrillation of VT/VF. • Also used as a prophylactic for recurrent VT/VF.
Dose: 1mg/kg bolus initially. An additional dose of 0.5mg/kg may
be considered. A lignocaine infusion may be considered once
there is a return of spontaneous circulation.
Adverse effects: Slurred speech, altered consciousness,
muscle twitching, seizures, bradycardia, hypotension, heart block
and asystole.
A beta sympathomimetic agonist, with positive inotropic and
chronotropic actions.
Indications: Bradycardias not responding to atropine.
Dose: Initial dose is 20mcg, which may be repeated every two
minutes until adequate perfusion is achieved. To prepare isuprel
dilute 200mcg/ml into 10mls of Normal Saline so that each ml
contains 20mcg.
Adverse Effects: Tachycardia, hyper/hypotension, angina,
nausea, headaches and flushing.
Adenosine
Suppresses the conduction through the atrioventricular node,
interrupting re-entry tachycardia.
Indications: SVT causing haemodynamic compromise (must be
administered quickly as it has a short half life).
Dose: 1st dose 3.0mg, 2nd dose 6.0mg, and 3rd dose 12.0mg.
Adverse effects: Flushing, dyspnoea, chest pain and AV
blocks.
Potassium
Potassium is an electrolyte essential for membrane stability.
Hypokalaemia can lead to ventricular arrhythmias, especially when
associated with hypomagnesaemia and digoxin therapy.
Indications: Persistent ventricular arrhythmias especially when
associated with documented hypokalaemia.
Dose: Bolus of 5mmol of potassium chloride.
Adverse effects: Hyperkalaemia may lead to bradycardia,
hypotension and possibly asystole, extravasation and tissue
necrosis.
Magnesium
Magnesium is an electrolyte essential for membrane stability.
Hypomagnesaemia can lead to myocardial hyperexcitability
particularly in the presence of hypokalaemia and digoxin therapy.
Indications:
• Torsades de pointes,
• Cardiac arrest associated with digoxin toxicity,
• Failure to revert VF/VT,
• Documented hypokalaemia,
• Documented hypomagnesaemia.
Dose: 5mmol bolus, which may be repeated once. This may be
followed by an infusion of 20mmol over 5 hours.
Adverse effects:
• Excessive use may lead to muscle weakness and respiratory
• Hypotension, bradycardia, and flushing.
Calcium is essential for normal muscle activity and nerve
conduction. It increases myocardial nerve excitability and
contractility and increases peripheral resistance.
Indications: Hyperkalaemia, hypocalcaemia, overdose of
calcium-channel blocking agents.
Dose: 5-10mls of 10% calcium chloride given as a bolus.
Adverse effects: Possible increase in myocardial and cerebral
injury by mediating cell death, tissue necrosis and extravasation.
Sodium Bicarbonate
Alkalising solution.
Indications:
• Hyperkalaemia, • Treatment of documented metabolic acidosis, • Overdose with tricyclic antidepressants, and • Prolonged arrest.
Early efficient CPR and adequate ventilation usually negates the
need for sodium bicarbonate.
Dose: 1mmol/kg over 2-3 minutes. This may be repeated if
required, and as guided by arterial blood gases.
Adverse Effects:
• Due to the risk of alkalosis, hyperosmolality and
hypernatraemia, sodium bicarbonate is not part of initial routine therapy.
• Intracellular acidosis may develop or worsen, • Sodium bicarbonate and adrenaline or calcium when mixed
together may inactivate each other, precipitate and block the IV line.
TREATMENT OF ARRHYTHMIAS
For further reading refer to the SWH Resuscitation Policy and
the ARC Guidelines, accessed at
www.resus.org.au
Ventricular Fibrillation and Pulseless Ventricular
Tachycardia:
Ventricular Tachycardia
Ventricular Fibrillation
For pulseless VT and VF it is advised that only 1 shock of
150J is delivered. If the arrest (VT/VF) has been witnessed by
a rescuer then 3 stacked shocks of 150J should be
administered. The rhythm should be quickly checked between the
stacked shocks to ensure the patient is still in a shockable rhythm.
• After defibrillation immediately perform 2 minutes of CPR. • During CPR consider the administration of adrenaline. • Administer adrenaline 1mg followed by at least 2 minutes of
• Check patient's rhythm; if the patient remains in a shockable
rhythm defibrillation is repeated as a single shock (150J) and followed by adrenaline and CPR. Further doses of 1mg of adrenaline may be repeated every 3 minutes, until return of a spontaneous rhythm.
• Amiodarone may also be administered after defibrillation, if
adrenaline and CPR have failed.
• Correct reversible causes. • Consider inducing hypothermia following VF arrest; refer
SWH Hypothermic Therapy following Cardiac Arrest Policy.
Torsades de Pointes
• First line treatment for Torsades is Magnesium. • Administer Magnesium 5mmol, followed by 2 minutes of
CPR if the patient is pulseless. Magnesium 5mmol may be repeated once, followed by an infusion of 20mmol over 5 hours.
• Defibrillation (1 single shock of150J) may be considered if
magnesium fails to revert the patient and the patient is pulseless.
• Continue CPR until the return of a spontaneous rhythm. • Correct reversible causes.
Asystole
• If the rhythm is asystole this should be confirmed by
changing leads to ensure rhythm is not fine VF (ECG leads must be connected to do this).
• Adrenaline 1mg every 3min followed by 2 minutes of CPR. • Consider Atropine 1mg repeated every 3-5 mins up to 3mg. • Continue CPR until the return of a spontaneous rhythm. • Correct reversible causes.
Pulseless Electrical Activity (PEA)
PEA is also referred to as Electromechanical Dissociation (EMD).The patient may have a normal rhythm on the monitor but has no cardiac output, ie: there is a mechanical dissociation where the myocardium is failing to pump. Therefore there is no palpable pulse.
• Adrenaline 1mg every 3 min followed by 2 minutes of CPR. • Atropine 1mg every 3-5 minutes up to a total of 3mg may
also be considered.
• Continue CPR until the return of a spontaneous rhythm. • Correct reversible causes.
Bradycardia with haemodynamic compromise &
Junctional Rhythm
Bradycardias may present as a number of different rhythms, for example sinus bradycardia, heart blocks, ventricular standstill, junctional rhythms and idioventricular rhythm.
• If the patient is compromised by any bradycardia then
treatment should be initiated.
• Atropine 1.0mg may be given every 3-5 minutes up to a
• If the patient has no recordable blood pressure or has a
loss of consciousness, then CPR must also be performed.
• Isoprenaline 20mcg boluses may be administered by
order of a medical officer. Consider Isoprenaline infusion.
• Temporary external pacing may be considered if the
above measures fail.
• The patient may also require the insertion of a
transvenous temporary pacing wire.
• Correct reversible causes.
Correcting reversible causes
Certain conditions may lead to cardiorespiratory arrest, and must be considered and treated during the resuscitation.
• Hypoxia • Hypovolaemia • Hypo/hyperthermia • Hypo/hyperkalaemia & metabolic disturbances. • Tamponade • Tension pneumothorax • Thrombosis – pulmonary / coronary • Toxins/poisons/drugs
REFERENCES
Advanced Life Support Revision and Update Packages, (2003). The Royal Melbourne Hospital. Australian Resuscitation Council Guidelines (2006). Drug Protocols. (2003). Cardiology Department, The Royal Melbourne Hospital. Heartstream AED's Technical Reference Manual, Philips Medical Systems. Heartstart XL Technical Reference Manual, Philips Medical Systems. Intensive Care Advanced Life Support Competencies Learning Package. (2000). St. Vincent's Hospital, Melbourne. International Liaison Committee on Resuscitation. (2005). Part 4: Advanced life support. Resuscitation, 67, 213-247. SWH Advanced Life Support Competency Assessment Education Package. (2004). SWH Temporary Transcutaneous Pacing Protocol. (2008).
Source: http://www.southwesthealthcare.com.au/assets/A/1230/25f8975adcee972db1fd7f9bc383e846/402134902ALS_packageRevisedFeb2010.pdf
Depth dependent properties of ito thin films grown by pulsed dc sputtering
ARTICLE IN PRESS Contents lists available at Materials Science and Engineering B Depth dependent properties of ITO thin films grown by pulsed DC sputtering A. Sytchkova , D. Zola , L.R. Bailey , B. Mackenzie , G. Proudfoot , M. Tian , A. Ulyashin a ENEA Optical Coatings Laboratory, via Anguillarese 301, 00123 Rome, Italy b Oxford Instruments Plasma Technology, Yatton, Bristol, BS49 4AP, UK
Indiana pharamcists alliance (ipa) continuing pharmacy education (cpe)
INDIANA PHARAMCISTS ALLIANCE (IPA) 2014 CONTINUING PHARMACY EDUCATION (CPE) Article Evaluation of Oral and Topical Therapies for Mild to Moderate Ulcerative Colitis inflammation and ulceration of the intestinal Jasmine Ho, PharmD mucosa and submucosa. The disease affects Columbus Regional Hospital approximately 700,000 Americans.1 Disease