Sa pathology newsletter

Reference interval changes 2 Significance of ANCA 4 Type 1 diabetes 6
INSIDe Clinical Utility of Bone Turnover Markers 8 Ulysses Syndrome – is it the
liver? 10 Test ordering standardisation 11 Order of Draw Quick Guide 12
HbA1cFor our patients and our population


transport improvement, will enable us to
Complement method change
From the Executive Director
meet future challenges and maintain
To improve turnaround times for
our hard earned reputation.
complement C3 and C4 results,
As part of a highly regarded health system
SA Pathology changed the method
that provides outstanding patient care,
and analyser platform to the
integrated research and teaching activities
ADVIA 2400 on 26 August 2013.
we aim to continually improve the depth
Results for both C3 and C4 using the
and breadth of our services whilst returning
new method are approximately
value for money to South Australian
10% higher than those of the old
method. The reference interval has changed to reflect this shift and a
As a clinical support service SA Pathology
paediatric range is included.
recognises that it needs to positively
IMVS IS headed by ProfeSSor ruth SaloM a MedIcal graduate
respond to the changing clinical landscape
who haS SPecIalISed aS a
in order to meet the needs of hospitals,
clinicians and the community. We also
recognise the need to manage demand and budget pressures, while ensuring our plans
are consistent with the major developments
MR KEN BARR IS EXECUTIVE
that are occurring within the health system,
DIRECTOR OF SA PATHOLOGY
including the new Royal Adelaide Hospital
and the South Australian Health and
Medical Research Institute (SAHMRI), plus the major research and teaching goals
>10 years and
of the three universities.
i am delighted to present this edition of the SA Pathology Newsletter (formerly
SA Pathology will be explicitly moving
the IMVS Newsletter). SA Pathology
away from the ‘one hospital, one
is proud to be the public provider of
laboratory' model as advances in analytical,
pathology services within South Australia
transport and IT technology provide
to ensure all our population, communities
new opportunities for us to build a more
DGA reference interval change
and patients have 24/7 access to a
flexible, efficient and effective state-wide
comprehensive range of services,
pathology network.
SA Pathology changed the
irrespective of their income and location.
Deaminated Gliadin Antibody (DGA)
Be assured that our services will continue
method and analyser platform on
The priorities and direction contained
to be clinically led, and that patient safety
9 December 2013. Whilst the new
within our 2013-16 strategic plan
and improving health outcomes remains
method is clinically identical to the
outline our clear intention to build on
our primary goal. We look forward to
current method the results will be
a longstanding record of quality and
working with you so that we can continue
considerably different.
excellence as a regulated and accredited
to provide the very best pathology service
pathology service across all disciplines
to support our patients and our population.
New reference interval
and our expanding Point of Care Testing
The new reference interval for DGA
network. Our plans for service, IT and
will be: <11 U/mL.
If you have any questions
SA Pathology Newsletter
Published by SA Pathology
regarding these changes
Editorial Committee
please contact the
John Bahnisch, Mark Fitz-Gerald, Ming Qiao,
SA Pathology Photo and Imaging
Immunology Consultant
Dianne Zurcher and David Johnston
via SA Pathology enquiries
on (08) 8222 3000
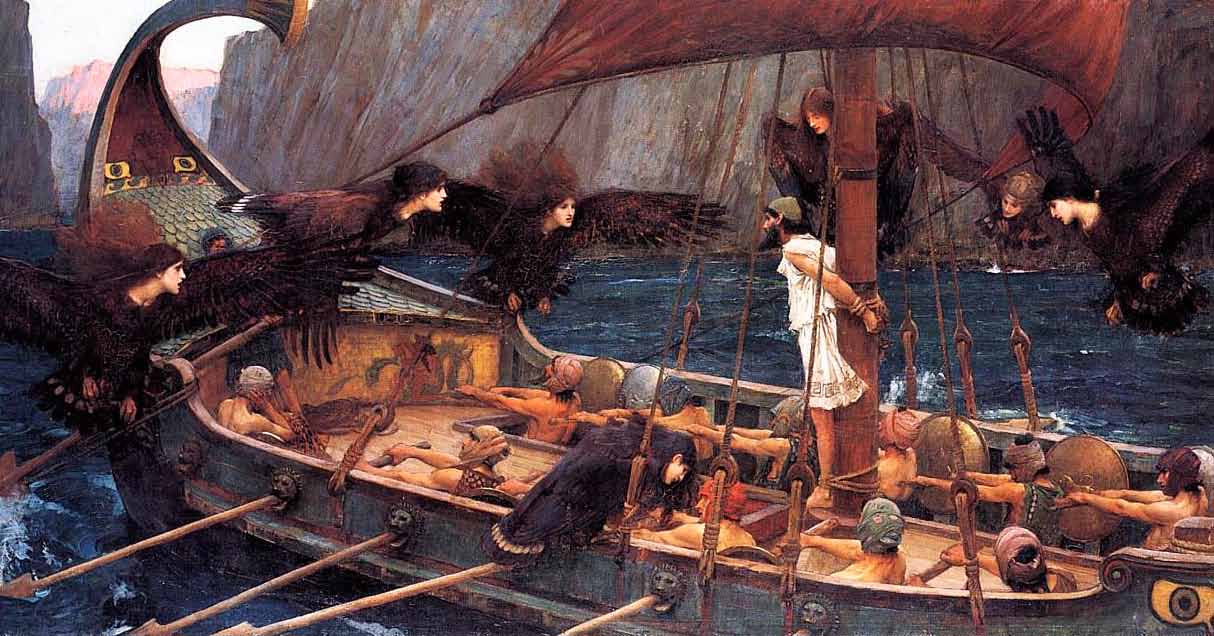
cover: Ulysses and the Sirens
ISSN 2203 – 2339 Print
by John William Waterhouse 1891
ISSN 2203 – 2347 Online
See page 10 for Ulysses syndrome
SA Pathology Newsletter > 1 – 2013


Red Blood Cell Folate (RCF)
What do I need to do
SA Pathology has moved from serum folate to Red Blood Cell Folate (RCF)
You will need to collect an
Citrate Blood Tubes
testing as the standard measurement
EDTA specimen (purple top).
to assess folate nutritional status.
When collecting blood into
Can I specifically request
citrate tubes (blue tops) you
Due to the 120 day average lifespan
serum folate testing?
must fill to the indicator line.
of the red cell, RCF folate is less
Yes. Serum folate levels will
susceptible to rapid changes in diet
A: continue to be available on
compared with serum folate, and will
provide more reliable and accurate results. In practice this change will:
Can I request tests to
n identify an additional 5% of
differentiate between B12
patients with folate deficiency with
and folate deficiencies?
spuriously high serum levels
Yes. Specific tests to identify
n more accurately reflect
and differentiate between
the patient's folate status over the
B12 and folate deficiencies,
preceding 2 to 3 months.
such as homocysteine and methylmalonic acid levels,
will continue to be performed. For B12 and RCF please collect both serum (white top) and whole blood (purple top).
> Mandatory folate
The reason is that the ratio of
fortification of flour
blood to anticoagulant is critical
has been in place since
for clotting tests.
2009 in Australia.
An under-filled tube will have too much citrate making results
Clinically related questions
invalid; similarly, overfilling
Please contact Professor Luen Bik To, Haematology Clinical Director on
the tube dilutes the citrate
(08) 8222 3633 or Dr Penelope Coates, Chemical Pathology Clinical Director
concentration invalidating the
on (08) 8222 3391.
Collection by vacuum is the method preferred as this takes
Warfarin reversal guidelines
To aid decision making in this patient
the correct amount of blood.
group the recently updated Warfarin
However if the tubes are old the
In-patients receiving warfarin and
Reversal Guidelines are now available
vacuum may be reduced resulting
experiencing bleeding is a relatively
on the SA Pathology internet site.
in under filling; please replace old
common event, with approximately
From the Home page go to: For
or defective tubes.
2-3% of such individuals having a
Clinicians Quick Guide for Clinicians
major complication each year.
Over or under filled samples will
Emergency Information.
be rejected and a new sample will
Patients on warfarin will also often
Further advice can be obtained
be required. This applies to all
have high INR values without
from the duty haematologist on-call
clinically evident bleeding. Guidelines
through the RAH switch board,
for the management of both bleeding
For additional information please
phone (08) 8222 4000.
and non-bleeding patients with
call the Haemostasis Reference
an elevated INR result have been
Laboratory on (08) 8222 3918.
developed by the Australian Society of Haemostasis and Thrombosis.
SA Pathology Newsletter > 1 – 2013
Dr TATjAnA BAnovic – CONsULTANT pATHOLOGIsT – ImmUNOLOGY
Anti neutrophil cytoplasmic antibodies (ANCA) are associated with a spectrum of systemic vasculitic conditions affecting small and medium vessels throughout the body.
The syndromes of small vessel
False positive results have been
vasculitides (SVV) systemic
reported in a variety of disorders
vasculitides are characterised by:
including infections, drug-induced vasculitis, other autoimmune diseases,
n overlapping clinical and histological
malignancies and inflammatory bowel
features with frequent involvement disease (IBD). Conversely, negative
results have been reported in patients
n the need for aggressive
with biopsy proven vasculitides.
immunosuppressive treatment
Results therefore should always be
n serious morbidity and a significant
evaluated in the context of other
laboratory and clinical findings and should not be used as the principal
The management of these vasculitides
indication for treatment.
often requires critical and timely decision making to prevent the
There are three major patterns
consequences of disease and the
associated with a positive ANCA
the aNca group of autoantibodies are directed
hazards of mistreatment. The
against cytoplasmic components in human
importance of understanding the
1 Cytoplasmic or cANCA
tests for ANCA used in the diagnosis cannot be overemphasised.
2 Perinuclear or pANCA
3 Atypical-ANCA pattern
There are many different antigen
specificities in the ANCA group
The limits of ANCA testing need
The atypical ANCA pattern has
of autoantibodies but only two
to be understood. To maximise the
been reported in IBD, cystic fibrosis,
have proven clinical associations,
predictive value of ANCA screening
autoimmune liver disease, drug-
anti proteinase 3 (PR3) and anti
it should only be performed on
induced ANCA and rheumatic
myeloperoxidase (MPO) antibodies.
appropriately selected patients.
diseases. In rheumatoid arthritis the
Tests for other ANCA specificities
The clinical indications of suspected
prevalence of atypical-ANCA has been are not currently clinically useful
ANCA-associated vasculitis include:
detected in 20 – 70% of patients and
and none have been proven specific
been associated with more severe
or diagnostically important for any
n glomerulonephritis
and long-standing disease.
particular disease. Therefore all
n pulmonary haemorrhage
positive ANCA screens must have
n cutaneous vasculitis, especially
their identity confirmed to PR3 and
with systemic features
n multiple lung nodules
n chronic destructive disease of
Results should be evaluated
the upper airways; long standing sinusitis or otitis
in context of other laboratory
n subglottic tracheal stenosis
and clinical findings
n retro-orbital mass.
SA Pathology Newsletter > 1 – 2013
What is ANCA?ANCA is a group of autoantibodies directed against cytoplasmic
components in human neutrophils, the two main antigenic targets being proteinase-3 (PR3) and myeloperoxidase (MPO). Clinical studies done at SA Pathology have found the combination of an ANCA screen and confirmation tests yield the best diagnostic information.
If an ANCA screen on initial
sensitivity around 60% for
Other factors besides diagnostic
presentation is positive but negative
microscopic polyangiitis and 50%
tests need to be considered before
for both PR3 and MPO antibodies it
for Churg Strauss syndrome. About
deciding to administer toxic
is more likely to be related to other
25% of patients with Wagner's
immunosuppressive therapy, they
diseases than ANCA associated
Granulomatosis are also anti MPO
vasculitides. However results must
positive. Anti MPO levels do not
n probability of improvement
be interpreted in context with
appear to reflect the disease activity
and potential side effects with
clinical findings as it may represent
of patients with primary vasculitides
additional biopsy investigations
a limited form of disease. Patients
and the effects of treatment are not
for whom there is a high index of
well documented.
n consequences and costs of
suspicion should be monitored with
mistreating nonvasculitic disorders
PR3 and MPO antibodies, which may
Anti MPO antibody is occasionally
n consequences and costs of delaying
become detectable as the disease
found in other forms of
or missing the diagnosis.
glomerulonephritis. It is present in about 30 – 40% of patients with anti
In the appropriate clinical setting for
Clinical associations
glomerular basement membrane
those patients with renal findings
(GBM) disease, and these patients
suggestive of vasculitis, initiation of
To date only PR3 and MPO antibodies
appear to have a better prognosis
immunosuppression based on ANCA
have been shown to be of value in the
than those with GBM antibodies
results alone without renal biopsy
diagnosis of vasculitides.
alone. Antibodies also occur in drug-
appears justified.
induced lupus and occasionally
The strongest disease association
in certain other connective tissue
In other clinical settings, a positive
is between anti PR3 antibody and
ANCA screen and MPO/PR3
Wagner's granulomatosis, which has
antibodies are not sufficient for
been reported in about 80% of active
In general, anti MPO and anti PR3
diagnostic decisions on patient
cases, however sensitivity varies
do not occur in the same patient
treatment. Positive ANCA results
according to disease activity and
in these settings must be confirmed
extent. The more limited forms have
with biopsy investigation.
sensitivities in the order of 67%,
while generalised forms are nearly
In a successfully treated vasculitis
100% of patients.
Systemic necrotising vasculitides
patient ANCA levels should disappear
are serious life threatening
or decrease significantly. If this is
PR3 antibody levels appear to
diseases, fatal if untreated. Since
not the case, or the levels reappear,
parallel disease activity. In general
the introduction of combination
a clinical exacerbation is likely to
high levels of anti-PR3 antibodies
corticosteroid and cyclophosphamide
occur within the next few weeks or
indicate active vasculitis and a sharp
therapy clinical outcomes have
rise in levels signifies disease flare.
improved dramatically. The current
Monitoring ANCA levels may be useful treatment schemes also include in discriminating between a disease
aggressive immunosuppressive
flare and non-specific infections in
patients with SVV.
Treatment should be started early
The presence of anti MPO antibody
as there is good evidence that the
strongly suggests necrotising
extent of organ involvement at onset
vasculitis. It has a reported
determines the ultimate prognosis, hence prompt diagnosis is critical.
SA Pathology Newsletter > 1 – 2013
diabetes: diagnosis
Drs jessicA PhiliPs, jenny couPer, jAn FAirchilD, AlexiA PeñA AnD elAine ThAm – pAEDIATRIC; ENDOCRINOLOGY WOmEN's AND CHILDREN's HOspITAL
Every day in Australia two children will be diagnosed with type 1 diabetes. Currently Australia has the world's sixth highest rate for new diagnoses of type 1 diabetes. The incidence is highest amongst teenagers, with a second smaller peak amongst 5-9 year olds, but it can occur at any age, including infancy.
A combination of genetic and
ketoacidosis (DKA), a life threatening
environmental factors is thought
complication and the leading cause of
to precipitate the autoimmune
death in children with type 1 diabetes.
Children with type 1 diabetes usually
destruction of the pancreas which
Recognising the symptoms and signs
present with a 2-6 week history of
leads to Type 1 diabetes. Despite
of the disease and starting insulin
polyuria, polydipsia, and weight loss.
years of research, improvements in
early can prevent morbidity and
Bedwetting is also common.
insulin and insulin delivery devices
These symptoms are often attributed
a cure remains elusive.
The following case study illustrates
to urinary tract infections or
Over 30% of children with type 1
the importance of early diagnosis and
psychogenic polydipsia. If these
diabetes still present in diabetic
early symptoms are not recognised and ketoacidosis develops, vomiting, abdominal pain, dehydration, reduced consciousness and hyperventilation
will ensue, and can be mistaken for gastroenteritis, acute abdominal pain,
Mia is 4 years old. Her mother takes her to the GP as she is concerned Mia
asthma or pneumonia.
might have a bladder infection. She has been going to the toilet frequently and has started wetting the bed again after being mostly dry overnight for
over a year. Today Mia complained of a sore tummy. She has had no fever
Once suspected, type 1 diabetes can be
or vomiting, but has been quite thirsty.
easily diagnosed with a blood glucose
Mia has no significant past medical
Because of the glucosuria, her
meter. The diagnosis is made if the
history. Her grandfather has type 2
BGL is checked and is 14mmol/L.
blood glucose level (BGL) is elevated:
Her GP thinks Mia may have type
n fasting BGL ≥7mmol/L or
1 diabetes and asks them to return
n random BGL ≥11.1mmol/L
Her GP agrees a urinary tract
in the morning for a fasting blood
infection is likely, though is
A fasting BGL, oral glucose tolerance
wondering about type 1 diabetes.
test (OGTT) or an HbA1c are not
Overnight Mia starts vomiting and
required for diagnosis. Waiting for the
Her urinalysis results are:
the abdominal pain worsens. Her
results of extra tests will only delay
mother takes her to the emergency
the diagnosis and management.
department. Her BGL on arrival is
18mmol/L with blood ketones of
Testing blood or urine ketones will
3.7mmol/L. A blood gas shows a
help determine if ketoacidosis is likely.
metabolic acidosis with a pH of
Children diagnosed with type 1
7.15 and bicarbonate of 10mmol/L.
diabetes require immediate referral
Mia is admitted to the paediatric
to a hospital with paediatric services
intensive care unit and an insulin
to commence insulin and organise
infusion started.
multidisciplinary education and management.
SA Pathology Newsletter > 1 – 2013
Leading Light Award
Children with diabetes can deteriorate
Polyuria, polydipsia, bedwetting and
quickly, and it is not uncommon for
weight loss are usual early symptoms.
a child to present in severe DKA whilst waiting to have a fasting BGL.
A random blood glucose level >11.1mmol/L, in a symptomatic child
The fasting BGL is not necessary
is enough to make the diagnosis.
associate Professor Susan branford
for a symptomatic patient with elevated random BGL. Very early on
Fasting blood glucose, OGTT or
Associate Professor Susan Branford
in the disease post-prandial BGLs
HbA1c are not necessary to make the
of the Leukaemia Unit, Department
are the first to rise and fasting BGLs
diagnosis and can delay treatment.
of Molecular and Genetic Pathology,
Centre for Cancer Biology at
Early diagnosis and immediate
SA Pathology won the Australian
referral to a doctor experienced in
Society for Medical Research (ASMR)
the management of type 1 diabetes
SA Leading Light Award in September
Type 1 diabetes can occur at any age,
in children can prevent diabetic
and is easily diagnosed if suspected.
This prestigious award recognises the exceptional research output by mid-career researchers who have pursued their own research direction,
Children with diabetes can
and highlights the outstanding work being undertaken by up and coming
deteriorate quickly
researchers in South Australia. The award was presented by Professor Ian Frazer.
Young Investigator
world diabetes day
Raising awareness within the community
KNOW THE DIABETES WARNING SIGNS!
about the four common signs of diabetes – weight loss, increased
thirst, increasing
urination and fatigue, reduces the number of children diagnosed late as in Mia's case.
dr Julia Kuliwaba
A recent Australian
Excessive
study demonstrated that
SA Pathology's Dr Julia Kuliwaba,
a population awareness
a researcher in surgical pathology, is
campaign was effective
the recipient of an International Bone
If your child shows these signs,
in reducing the number
and Mineral Society (IBMS) 2013 Sun
seek immediate medical attention.
of children who present
Valley Young Investigator Award – the
in DKA by 64%. ¥
Alice L. Jee Award – for her research investigating the pathophysiology of
Diabetes can affect children at any age. If left untreated, diabetes is deadly.
The award was presented at the 43rd International Sun Valley Workshop on
Musculoskeletal Biology, Sun Valley, Idaho, in August 2013.
SA Pathology Newsletter > 1 – 2013
Dr DevikA ThomAs
Osteoporosis is a major public health issue. Diagnosis relies on a bone mineral density (BMD) measurement, using dual energy X ray absorptiometry, and is defined as a bone density more than 2.5 standard deviations below the young normal (peak bone) values at the lumbar spine or the hip. Bone turnover markers (BTM) can be used as a complement to BMD in monitoring treatment response as well as fracture prediction in patients with osteoporosis.
Bone Turnover Markers
serum. Total alkaline phosphatase
may be used in place of bone specific
Fasting morning serum CTX and
BTM are products of bone formation
alkaline phosphate in the absence of
P1NP are convenient measures of
and resorption. Bone is dynamic
liver disease.
bone turnover. Diurnal variations and
tissue with formation and resorption
effects of food intake affect marker
occurring concurrently at many
levels, and serial collections for
multi-cellular bone remodelling units,
Products of osteoclasts and terminal
monitoring should be collected under
hence the measurement of BTM
telopeptides of mature type 1
the same conditions, at the same
reflects bone turnover and rates of
collagen (like serum crosslaps –
time of day and analysed by the same
formation and resorption.
CTX) are bone resorption markers.
laboratory to minimise biological and
Currently CTX is the most widely
used bone resorption marker having
Products of osteoblasts (osteocalcin,
replaced the urine-based crosslinks
Who to test and when?
bone specific alkaline phosphatase)
test. Products of osteoclasts are not
and type 1 procollagen extension
BTM testing is not a screen for
routinely measured in clinical
products (P1NP) are markers of bone
osteoporosis and has not been
formation that can be measured in
validated as a diagnostic test, which still requires bone density measurement. However, BTM testing is useful for monitoring the treatment
response to antiresorptive agents in patients with osteoporosis, and in the
early recognition of non responders. This is an important indication because alternative treatment may
be offered to non responders.
BTM testing may be requested prior
to commencement of treatment. Following initiation of anti-resorptive therapy it is useful to measure BTM again at three to six months to ensure
adequate response, followed by re-assessment once or twice a year while treatment continues.
SA Pathology Newsletter > 1 – 2013
Follow up with BTM testing is still
When monitoring treatment response
useful even without a baseline value,
the target would be a 30% fall in bone
if the blood samples are collected
resorption markers within weeks of
n There is no consensus on the
under recommended conditions
commencing therapy. The desirable
use and interpretation of BTM
(ie: morning fasting samples) and
limit for P1NP in postmenopausal
and no recommendations in
analysed by the same laboratory to
women is <75 ug/L.
clinical guidelines.
n Reference intervals and desirable
Table 1 p1Np reference range
limits vary between laboratories.
n The baseline BTM level cannot be
BTM are not specific to a disease
used for diagnosis of osteoporosis,
and therefore cannot be used for
it does not direct treatment choice
diagnosis, however raised bone
nor will it predict treatment
resorption as reflected by raised CTX
may suggest bone loss and loss of
n Only a fall in BTM greater than
bone microarchitecture not captured
the least significant change
by bone density measurements.
(30% for serum markers) may be
Therefore changes in BTM precede
regarded as a response to
treatment and proof of compliance.
BTM are raised in Paget's
n It is not known to what extent
disease, osteoporosis and other
BTM should fall to optimise anti-
conditions where bone turnover
fracture efficacy.
is high, such as rheumatoid
n Bone markers may be higher in
arthritis, hyperparathyroidism and
BTM are also useful in recognising
patients with renal failure and
hyperthyroidism. They are also
non compliance and sometimes,
dialysis dependent patients due
generally higher in patients with renal
helps identify those who may take
to accumulation over time, and
impairment due to low clearance.
the medication incorrectly (i.e. taking
may not directly reflect bone
bisphosphonate tablets with food or
turnover rate.
Monitoring therapy
calcium tablets).
There is no consensus on a BTM
target with as many as 50% of women
Fracture prediction
with osteoporosis having a BTM in
There is clear and convincing evidence BTM can be used to identify patients
the premenopausal range. The aim
from epidemiological studies that
with high bone turnover who may be
of treatment would be to return BTM
BTM are an independent predictor
at greater risk of fragility fracture.
to premenopausal levels. In patients
of fractures, particularly of the spine
Comparison between baseline and
treated with anti-resorptive agents,
and hip. Elevated CTX levels are
subsequent BTM levels can be used
levels of serum CTX of <400ng/L or
associated with significantly increased
to monitor treatment response and
at least 30% reduction from baseline
risk of fragility fractures. However
patient compliance. In patients treated
level should be the therapeutic target.
there is no evidence to support BTM
with anti-resorptive agents, at least
for predicting fractures in individual
30% reduction from baseline level
P1NP has been shown to convincingly
patients and fracture calculators do
should be the therapeutic target. ¥
and significantly rise after treatment
not incorporate BTM as yet.
with teriparatide. When treated with anti resorptive agents such as bisphosphonates, strontium ranelate and denosumab, BTM fall significantly compared to baseline values.
SA Pathology Newsletter > 1 – 2013
– is it the liver?
Dr DevikA ThomAs
This interesting case highlights the value of clinical history when interpreting test results, particularly those like liver enzymes with significant non-specificity. It reminds us that context is crucial to unravelling the complex web of influences that produce any set of test results. For more on the liver function tests refer to IMVS Newsletter 57.
DiscussionLiver enzyme patterns are used
A 20 year old football player was admitted to the emergency Department
to classify liver disease into two
with a fractured mandible. Routine biochemistry tests revealed elevated
broad categories – cholestatic
AST, ALT and LD with normal GGT, ALP and bilirubin. There were no clinical
disease (biliary obstruction) or
or historical findings to explain the elevated Liver Function Test (LFT) results.
hepatocellular disease. GGT and ALP
Following surgical repair of the mandible the patient's GP was informed of
are mainly located on cell membranes
the results and requested follow up. Repeat results by the GP revealed
and particularly line the biliary
the following.
cannaliculi, therefore they are raised in any obstructive biliary disease
anti mitochondrial, anti LKM and
(cholestasis, metastatic lesions).
anti smooth muscle – all negative
They may also be induced by alcohol
n Ceruloplasmin, alpha 1
and a variety of medications, anti-
antitrypsin, haptoglobin, serum
convulsants being the most common.
protein electrophoresis and
coagulation studies were normal
Transaminases (ALT and AST
are intracellular enzymes that are
n Iron studies showed normal iron
released due to cellular injury, and
are elevated in viral hepatitis and
n Chest, abdominal and pelvic
in cell destruction due to toxins
CT scans – normal
and medications such as high dose
n Liver biopsy revealed normal
paracetamol. Levels may rise 2 to
The GP organised a liver and biliary
hepatic and biliary tree histology
100 fold. Other causes of raised
ultrasound which was normal. The
Repeat liver function tests confirmed
transaminases are non alcoholic
patient was then referred to the liver
ALT, AST and LD remained elevated
steatohepatitis, haemochromatosis
clinic. Subsequent investigations
while GGT, ALP and bilirubin were
and autoimmune liver disease.
AST and LD are also found in red
n ALT and AST had risen to
The patient was referred to a
blood cells and muscle cells including
220 and 684 U/L respectively
haematologist but no haematological
cardiac cells. Intravascular haemolysis
n Hepatitis A IgG, Hepatitis B
cause was found for the abnormal
or haemolysis of the sample after
surface antigen and Hepatitis C
results. Following consultation
collection often raises LD and AST. In
antibody tests were negative
with a chemical pathologist, and
some haematological diseases LD may
n CMV and EBV IgM serology tests
considering the patient's routine of
be markedly elevated (myelodysplasia
playing football most days, a CK level
and pernicious anaemia).
n Autoantibody tests including
was requested, which was 2605 U/L
If cardiac causes are suspected then
ANCA, ANA, ENA, dsDNA,
a troponin T assay is recommended
SA Pathology Newsletter > 1 – 2013
‘Ulysses syndrome' is the term used to describe an unnecessary
complication of the
diagnostic decision
Test ordering standardisation
where false-positive
results or clinical
decisions trigger a
Historically ordering an MBA panel
If you request an LFT plus an
complex diagnostic
has been something of a ‘movable
additional chemistry test from
work-up to elucidate
feast'. Everyone seems to have their
the MBA suite then you will receive
the nature of what is,
own interpretation on what should
a full MBA report.
in fact, not a disease.
be reported with an MBA.
To clarify this situation SA Pathology
named after Classical
has implemented consistent panel
Greek hero Ulysses, who fought in
definitions for the basic chemistry
the Trojan War (1194 to 1184 BC)
and subsequently took 20 years to
return home to Greece; however
If you request an MBA, or any of
all his harrowing diversions proved
the test panels listed below, you
will receive the tests as listed.
along with an ECG and clinical history. AST and LD are abundant
in skeletal muscle. Although ALT
is regarded as a liver specific
transaminase, it is also present in
skeletal muscle and with persistent
SA Pathology has also now
muscle injury ALT may also be
standardised on ECU as the renal
function panel. Note that glucose
is not included in the ECU panel
and should be separately requested,
and a grey top sample collected.
A good history would have given
The grey top provides a more stable
the clue to severe muscular exertion
collection environment for glucose
as a potential cause. In this case,
and hence results are more
persistent exertions in the form
of severe exercise lead to the consistently elevated AST, ALT, LD
and CK from skeletal muscle.
(The half life of ALT is up to 57 hours
while that of AST and CK are less than 24 hours.)
The differential diagnosis could have
been supported by requesting the
Total Cholesterol
patient to have a repeat blood test
after a few days rest to confirm that the cause was indeed exertion.
Calculated Ionised
n For more information
The ‘health dollar' is a premium
please speak to a SA Pathology
commodity, and in this case it's easy
Marketing representative
to see how much time effort and money could have been saved by
including a good history with the request.
multiple Biochemical Analysis
Liver Function Test
> for list of acronyms
Renal Function Test
Electrolytes, Creatinine, Urea
SA Pathology Newsletter > 1 – 2013
Vacuum Blood Collection System
Quick Guide Surgery Draw – Quick Guide
The volume of blood taken should be age appropriate and minimal. Please c
Order of D
equency of collec
The SA Pathology Order of Draw Quick Guide
has recently been updated. Whilst many of the
Blood Cultures (pair
tests and tubes remain the same there have
Anaerobic (purple)
been a number of significant updates including
the introduction of the ‘yellow top' for tissue
INR, APTT, PT, Fibrinogen, D
typing and platelet clumping.
PSA, Tumour Markers, Iron S
For comprehensive information on all the
(Serum - Fast Clotting)
tests SA Pathology provides please visit our
oponin, Lithium,
o antibody tests, Viscosity
web site at www.sapathology.gov.au or
Cholinesterase, Lymphoc
simply scan the QR code with your
xiline, T Cell subsets
smartphone to go direct to the Pathology
Collection Guide page.
tion, Antibody Screen
4ml: CBE, ESR, Haemoglobin, H
thy/Thalassaemia S
9ml: Blood borne
EDTA + GEL
Homocysteine, Ammonia, PTH
Tissue Typing, Platelet ‘Clumping'
Fluoride
thology Collection G
Allergy Test Requests
The test information sheet, ‘Allergen
Testing Guidelines' contains
Liver Function Tests
Epstein Barr Virus
recommendations related to ordering. You can read or print the guidelines
on the SA Pathology web site.
Gamma Glutamyl Transferase
Anti Neutrophil Cytoplasmic Antigen
From the home page go to: For
Clinicians Pathology Collection Guide
Alkaline phosphatase
Anti Nuclear Antibody
and type ‘allergy' into the search box;
click on the More Info link.
Alanine Aminotransferase
Extractable Nuclear Antigen Antibody
For clinical questions please
phone SA Pathology Enquiries on
Aspartate Amino Transferase
Double stranded DNA antibody
(08) 8222 3000 and ask for the
Immunopathology Registrar or on
Lactate Dehydrogenase
Liver-Kidney microsomal Antibody
The SA Pathology Allergy Test
X-ray Computed Tomography
Request form has been discontinued.
SA Pathology enquiries
> Metropolitan 8222 3000 > Regional and Country 1800 188 077
SA Pathology Newsletter > 1 – 2013
Source: http://www.sapathology.sa.gov.au/wps/wcm/connect/5b97ce6b-278b-479e-9e7f-2370c3728bcb/SAPNL_1_e.pdf?MOD=AJPERES&CACHEID=5b97ce6b-278b-479e-9e7f-2370c3728bcb
Die wahrscheinlichkeit, dass katzen mit husten an einer atemwegserkrankung leiden, ist bei weitem größer als die wahrscheinlic
Wenn die Mieze hustet Ein Überblick über feline Atemwegserkrankungen Husten bei einer Katze sollte man nicht auf die leichte Schulter nehmen. Katzen erkälten sich nicht so leicht wie wir Menschen, Husten gehört bei ihnen nicht zum „Alltäglichen". Daher sollte eine Katze, die wiederholt hustet (ohne dabei etwas hervorzuwürgen, z. B. Haarballen) dem Tierarzt vorgestellt werden.Erste Asthma-Anzeichen zeigen sich oft im Alter von 1 – 3 Jahren, können aber auch früher oder später auftreten. Bei manchen Katzen tritt parallel Niesen und / oder Augenausfluss auf.Wenn eine Katze schwere Atemnot hat (mit geöffnetem Maul und sichtlicher Anstrengung atmet, dabei die Ellbogen evtl. etwas nach aussen dreht), muss sie unverzüglich in tierärztliche Behandlung – dieser Zustand ist lebensbedrohlich! Auch wenn es mitten in der Nacht geschehen sollte – warten Sie lieber nicht bis zum Morgen, sondern rufen Sie den tierärztlichen Notdienst oder bringen Sie Ihre Katze ins nächste Tierspital.
Insect repellents
West Nile VirusInsect Repellents and DEET Tips:Deciding on Their Use Chemical repellents are effective at reducing bites from insects that can transmit disease. But their useis not without risk of health effects, especially if repellents are applied in large amounts or improperly.This information will help you decide when and if a repellent is right for you.