Powerpoint presentation
Lewis-Manning Hospice One of the well-recognized reasons for deficiencies in the management of pain is inadequate pain assessment and lack of knowledge about the Analgesic Lewis-Manning Hospice. The Patient in Pain. Module 1. Lewis-Manning Hospice Aims of the presentation is to improve your knowledge about: The Pain experience Pain Assessment The Analgesic Ladder Lewis-Manning Hospice Clear distinctions between types of pain is not always possible. Simple classifications of pain invariably result in some omissions and overlap. However, discussions of pain often refer simply to Acute pain – Defined by the International Association for the Study of Pain as "Pain of recent onset and probable limited duration. It usually has an identifiable temporal and causal relationship to injury or disease" Chronic pain (non-malignant) – pain that lasts for more than 3 months, and beyond the usual course of the acute disease or expected time of healing. Sometimes the pain can impair other functions and is associated with major changes to personality, lifestyle and functional ability. Lewis-Manning Hospice Definition of pain An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in such terms as tissue damage (International Association Study The definition of pain that is possibly the most appropriate for use in clinical practice was given by Margo McCaffrey in 1968, who defined pain as "whatever the experiencing person says it is, existing whenever he says it Lewis-Manning Hospice Pain is a major symptom in many medical conditions and is one of the most common reasons as to why patients seek medical opinion Acute pain is a critical component of the body's defence system. It is part of a rapid warning and defence relay, instructing the motor neurons of the central nervous system to minimize physical harm ie remove hand from the fire Lewis-Manning Hospice Classification of Pain Nociceptive pain: that is painarising from a noxious stimulation of visceral pain – pain from major
organs ie surgery or trauma somatic pain –generally well-localized
pain that results from the activation of peripheral nociceptors without injury to the peripheral nerve or central nervous Neuropathic pain – that is pain
arising from the damage to nerve eg - cancers, diabetic neuropathy or even following surgical procedures ie following amputation Lewis-Manning Hospice Accurate pain assessment is the cornerstone of pain management (Macintyre & Ready, 2001) Pain is seen as the 5th Vital Sign and MUST be recorded alongside traditional vital signs Lewis-Manning Hospice The aim of the assessment is to identify all the factors, physical and non-physical, that affect the patient's perception of pain (Biopsychosocial model) A comprehensive clinical assessment is essential to gain a thorough understanding of the patient's pain: • Select an appropriate pain assessment tool • Select an appropriate analgesic therapy • Evaluate the effectiveness of interventions and modify therapy according to the patient's response Lewis-Manning Hospice Assess location and intensity of pain
Assessing a patient in pain using "SOCRATES"
Socrates is an acronym used by Health Care Professionals to evaluate the nature of pain that a patient is experiencing. It is used to gain an insight into the patients condition and to allow the practitioner to develop a plan for Also consider whether patient normally takes any analgesia – take a full drug history (possibly examine patient) When did pain start and was it sudden C haracter
What is the pain like ie stabbing, burning R adiation
Does the pain radiate anywhere A ssociations
Any other signs or symptoms associated with the pain T ime course
Does the pain follow any pattern E xacerbating /
Does anything change the pain Relieving factors S everity
How bad is the pain Pain Assessment Tools recommended at PHNT Verbal Report Visual Analogue Scale Numerical Rating Scale Wong and Baker (Paediatric) •Assess pain and document score on Obs chart •Please use one of the assessment tools •Self reporting scores are more reliable than behaviour •Use the most appropriate tool for the patient •Treat if moderate or severe. Reassess every 30mins
•If moderate or severe pain persists, patient should be reviewed by medical team and analgesic regime reviewed Lewis-Manning Hospice FLACC Score: non verbal adults Face No particula r expression Occasional grimace or frown,
Frequent to constant quivering or smile, eye contact and withdrawn, disinterested, worried chin, clenched jaw, deep furrows interest in surroundings eyebrows lowered, eyes closed, mouth eyes partially closed, mouth pursed opened, deep lines around nose and Legs Normal position or relaxed Uneasy, restless, tense, increased Kicking or legs drawn up,
tone, rigidity, intermittent hypertonicity, exaggerated flexion/extension of limbs flexion/extension of limbs, Activity Lying quietly, normal
Squirming, shifting back and forth, Arched, rigid, jerking, fixed position, moves easily and tense, hesitant to move, guarding, position, rocking, side to head pressure on body part movement, rubbing of body part Moans and whimpers, occasional Crying steadily, screams or sobs, (awake or asleep) cries, sighs, occasional complaint moans, grunts, frequent complaints Consola- Calm, content, relaxed, Reassured by occasional touching, Difficult to console or comfort
does not require consoling hugging or being talked to Pain assessment in non verbal adults remains a chal enge. Distress behaviours may be unrelated to pain. The FLACC may have an advantage over other behaviour tools for integration into routine care because of its simplicity and relative ease of use. Further study in a variety of settings involving diverse cultures and races would provide data for further validation and generalization of this scale. Lewis-Manning Hospice Harmful effects of unrelieved acute or chronic pain: Surgery, trauma (acute) and tumour growth and the pain associated with them, trigger a number of physiologic stress responses in the body These stress responses activate the sympathetic nervous system and alert the body to impending or existing harm. The purpose of the stress responses are protective in nature These include preventing further damage, minimizing blood loss, maintaining perfusion to vital organs, promoting healing, and preventing and fighting infection
Pain and stress responses, especially when prolonged, can
produce a number of harmful effects …………
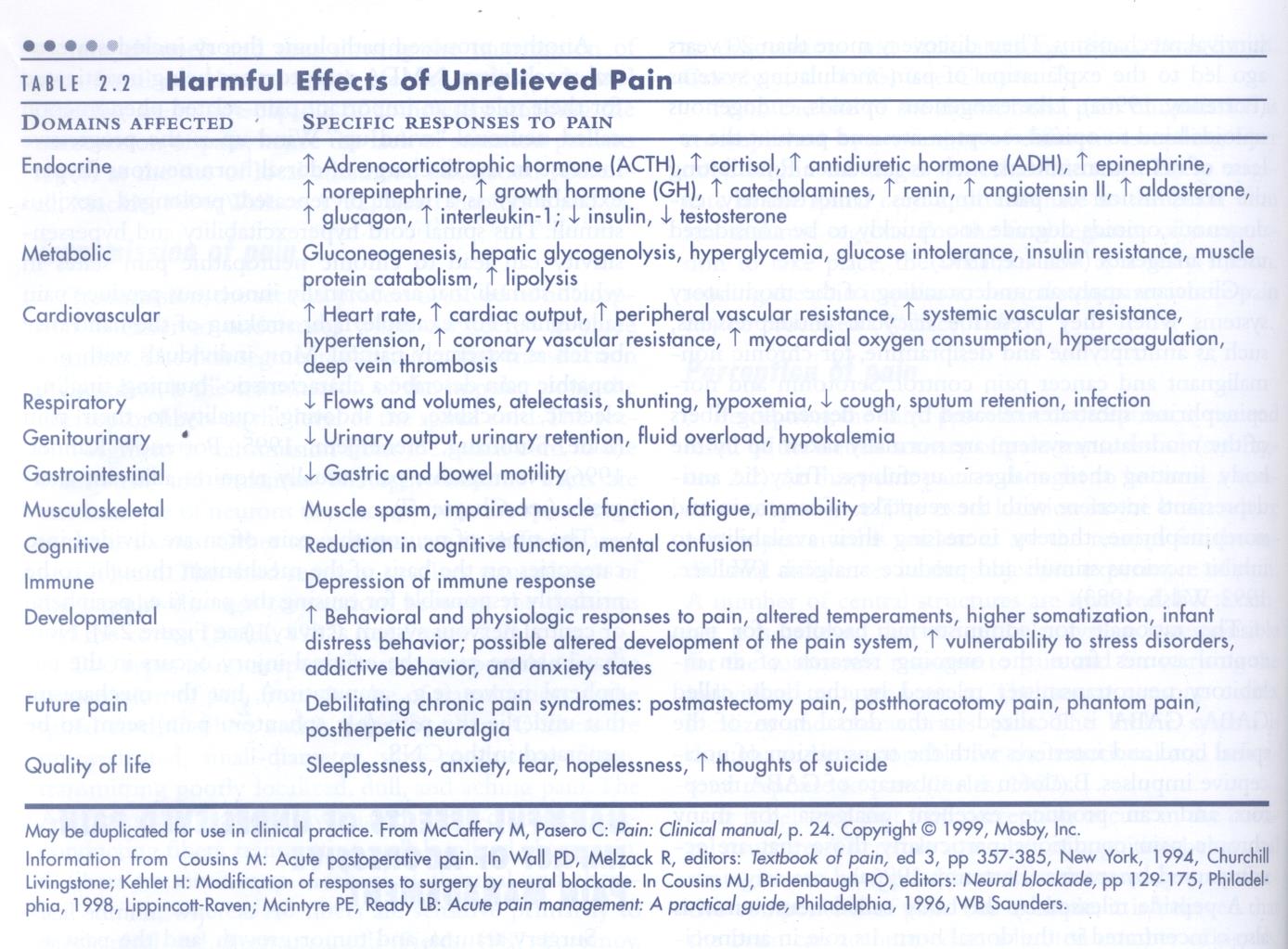
Lewis-Manning Hospice
Lewis-Manning Hospice
So how do we treat acute pain?
Lewis-Manning Hospice
The Analgesic Ladder
What is the "Analgesic Ladder "?
A conceptual framework for the prescription of
analgesic drugs put forward by WHO (1986) Although initially for cancer patients it can be
used in all pain settings
It is the simultaneous use of drugs from
different pharmacological backgrounds to
produce greater degree of analgesia otherwise
known as "balanced analgesia"
Lewis-Manning Hospice
Why recommend Balanced Analgesia?
Underlying principle is that following good pain assessment and a
thorough knowledge of a small number of analgesics, a simple
approach should produce effective pain relief
Reduces unwanted side effects Increases safety margins Sometimes pain is continuous – give "simple" analgesia on a regular
basis even if patients have a low pain score
The Analgesic Ladder should be seen as a "two way process" that
you use to manage fluctuating levels of pain
Lewis-Manning Hospice
Analgesic Ladder
for non-malignant acute pain
Surgical Patients
If pain unresolved:
eGFR ≥ 30ml/min
Oramorph dose PRN 2hrly
Identify type of pain and
consider adjuvant medication
As for moderate pain
Surgical Patients
Contact Medical Team or
PRN Oramorph 20-30mg
Senior Nurse for review
Oxynorm dose PRN 2hrly
Regular Paracetamol 1g qds
(maximum paracetamol
(adjust by age - see notes)
dosage 60mg/kg/day if weight
< 50kg. See drug chart for
Regular Paracetamol 1g qds
Medical Patients
(maximum paracetamol
Regular Oramorph 5mg 4
dosage 60mg/kg/day if weight
Regular NSAID
< 50kg.See drug chart for
(unless contraindicated e.g.
Increase to 10mg 4 hourly if
This guideline is to be used in conjunction
necessary
with the BNF and PHNT joint formulary.
eGFR < 60ml/min. See drug
>75 yrs reduce to 2.5mg 4
Ensure a full pain history is taken from all
chart for further advice)
eGFR ≥ 60ml/min
patients and regular analgesics are
PRN intermediate opioid
Plus Oramorph of the same
Be aware of the dose equivalence of
Consider PRN NSAID unless
(eg:Codeine 30-60mg qds,
dose 2 hourly PRN
opioids prescribed – particular care is
contraindicated (see drug chart
Tramadol 50-100mg qds)
needed with opioid patches.
for further advice)
Consider subcutaneous route rather than
repeated im injections.
eGFR < 60ml/min
eGFR < 60ml/min
eGFR < 30ml/min
Be aware of the influence of renal impairment, age and opioid tolerance on
Avoid non-steroidal anti-
opioid prescribing. Refer to opioid
inflammatory drugs.
prescribing guidelines if unsure.
2 hourly (ad
Avoid non-steroidal anti-
pioid equivalence:
(adjust by age - see notes)
inflammatory drugs.
10mg oral morphine
•5 mg Morphine SC/IM
eGFR < 30ml/min
Medical Patients
•3mg Morphine iv
Caution with tramadol and
Regular Oxynorm 2.5mg 4
•5mg oral Oxycodone
•50mg oral Tramadol •120mg oral Codeine
1-2mg for >75yo may be
•200mcg sublingual Buprenorphine
available as liquid
NB: Fentanyl patches are not to be used for
acute pain (consultant prescribing only)
Pain is the "Fifth Vital Sign" and must be assessed and recorded alongside other vital signs
All staff involved in the prescribing, dispensing and administration of controlled drugs must be familiar with
characteristics of the drug
Lewis-Manning Hospice
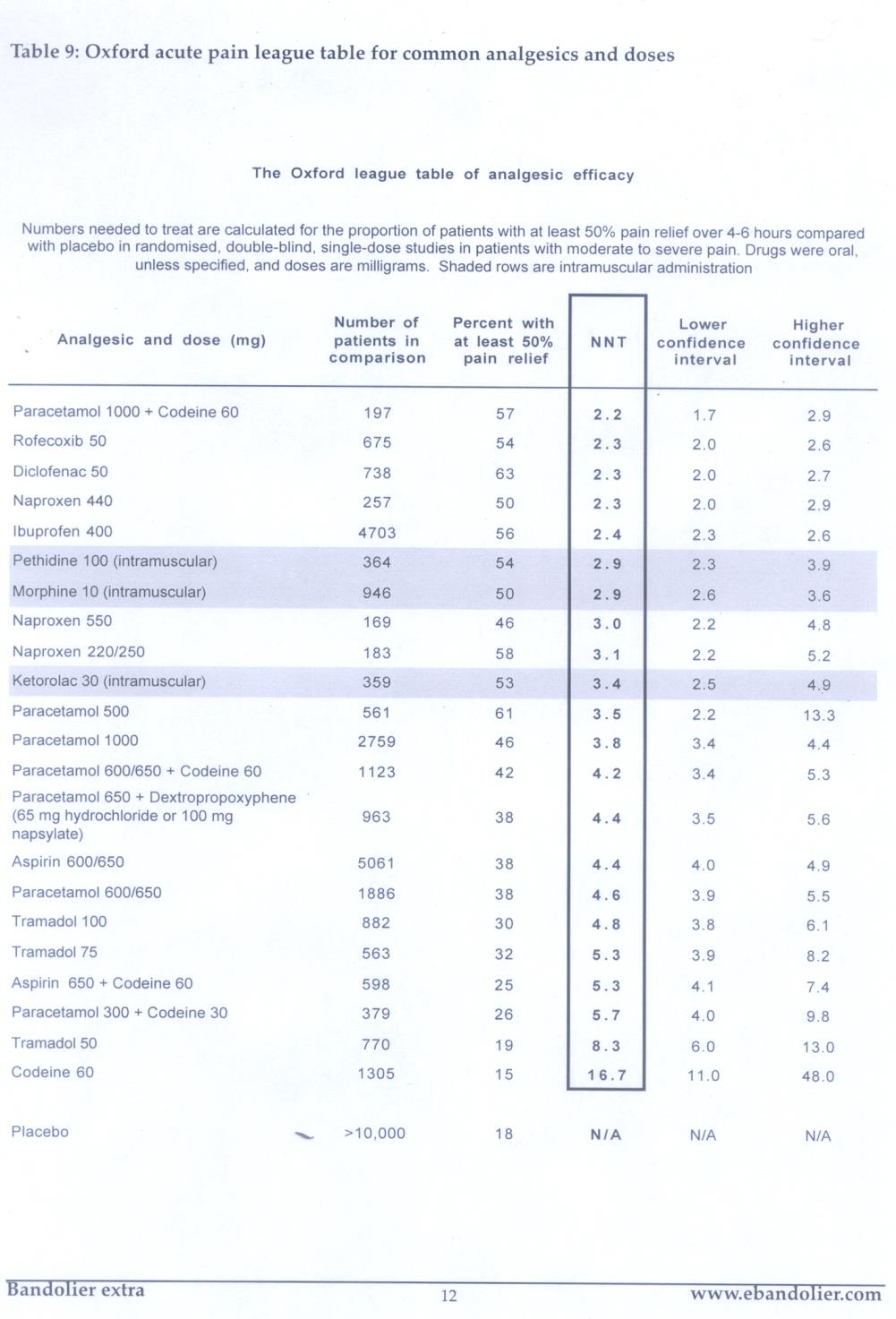
Efficacy of Analgesia
The Number Needed to Treat (NNT) is
the number of patients you need to treat
to prevent one additional bad outcome ie
poor analgesia. NNT for analgesic efficacy
is based on the number of patients who
receive the active drug to achieve at
least 50% pain relief compared with
placebo over a given period
The ideal NNT is 1 where everyone
improves with treatment. The higher the
NNT the less effective is the treatment
Example: if a drug has an NNT of 5, it
means you have to treat 5 people with
the drug to prevent one additional bad
The most effective drugs have a low NNT
of just over 2. This means that for every
two patients who receive the drug one
patient wil get at least 50% relief
because of the treatment (the other
patient may or may not obtain relief but it
does not reach the 50% level)
http://www.medicine.ox.ac.uk/bandolier/
Lewis-Manning Hospice
NNT League Table
League tables do not (or at least should not) tell us what
to do, but they should make deciding what to do easier,
and help us make choices for individual patients and for
care pathways. Remember that pain is a subjective
experience and should be tailored to an individuals
Lewis-Manning Hospice
Paracetamol- first recognised for its pain (and fever) properties
in 1893 by Von Merling (Forrest et al, 1982)
Is probably the safest non-opioid analgesic for most patients. Can be
given 4 – 6 hourly. Not to exceed max dose 4g in 24 hours
Route of administration: PO including dispersible (caution with renal
patients ie sodium levels), IV and PR
NNT of 3.8 with opioid sparing effect
Excellent baseline analgesia generally used for patients who have mild
Caution: Max dose of 3g/day in hepatocellular insufficiency, chronic
alcoholism, chronic malnutrition or dehydration. Note the therapeutic
range and the toxic blood concentration can be highly variable in
certain individuals. Overdose can be potentially fatal
Maximum dose 60mg/kg/day if weight <50kg
In repeated use does not result in tolerance or physical dependence
Causes no respiratory or cardiovascular depression
Lewis-Manning Hospice
Step 1 (or 2)
NSAID's – Diclofenac (Voltarol), Ibuprofen, Ketorolac,
Mefenamic acid, Naproxen, Piroxicam etc
Considerations:
Various routes of administration. Can be given PO, IV, IM,
Relieves pain through multiple mechanisms
Frequency of administration dependent on the NSAIDs
prescribed ie OD, BD, TDS, QDS
Efficacy unclear
NNT: Diclofenac(50mgs) 2.7 & (100mgs) 1.8, Ibuprofen
but consider NNH (numbers needed to harm)
Act on CNS and at the site of injury
Allergy reaction
Lewis-Manning Hospice
Adverse Events associated with NSAIDs –patients have
different degrees of risk and certain NSAIDs carry higher
risks than others:
NSAIDs are contraindicated in:
significant renal insufficiency
Avoid if eGFR <30ml/min (Stage 4 CKD. Refer to BNF prescribing in renal impairment)
Caution if eGFR <60ml/min (Monitor eGFR, UEs & Creatinine closely)
Gastrointestinal complications. GI ulceration and bleeding. Caution with
patients with inflammatory bowel disease ie Crohns or Ulcerative Colitis
due to tendency to cause ulceration of gastric lining Previous adverse event ie asthma associated
Cardiac – congestive heart failure, heart failure. Can increase the risk
of myocardial infarction In the presence of thrombocytopenia or coagulopathy
Other: implications in cases of Stevens-Johnson Syndrome
First and third trimester of pregnancy
Some evidence to suggest NSAIDs effects bone healing processes
Caution with drug interactions ie Warfarin
Lewis-Manning Hospice
Opioids ("Morphine like drugs")
Opioid analgesia is the preferred name given to "narcotics"- derived from
the Greek word "stupor"
Opioids are drugs that relieve pain by binding to multiple types of
specific receptors in the nervous system (spinal cord and brain stem)
Until the mid 1970s very little was known about the mechanism of action
of opioid drugs. Since then, not only have receptor sites for these drugs
been identified but it has also been discovered that the body is capable
of producing its own opioids (endogenouse opioids ie endorphins,
enkephalins & dynorphins)
Opioids produce an agonist effect –
When a drug combines with a receptor site to produce the action of that
receptor it is considered an agonist. Consequently a drug that binds with
a receptor and inhibits activity is considered an antagonist.
Examples of Commonly used Opioids in Derriford: Codeine, Morphine,
Fentanyl, Oxycodone, Diamorphine, Pethidine, Tramadol

Lewis-Manning Hospice
3 main Opioid receptors producing the
following effect
(analgesia, respiratory depression,
euphoria, bradycardia, pruritus, miosis,
N&V, inhibits gut motility, physical
(analgesia, sedation, psychotomimetic
effects, dysphoria, diuresis)
The first clinical indicator that a patient is
accumulating opioids is that their sedation
score will deteriorate. Close monitoring is
vital when initiating opioids, especially to an opioid naive patient
Lewis-Manning Hospice
Common weak opioids
Lewis-Manning Hospice
Usually prescribed at 30 – 60 mgs 4- 6 hrly, Max 240 mgs / 24
hrs (ceiling dose)
General rule - give at same time as Paracetamol (Bandolier)
consider NNT – Codeine 60mgs = 16.7 whereas 2.2 when
given with 1 g Paracetamol
Metabolized in the liver, excreted by the kidneys so use
cautiously with patients with renal impairment
Approx 10% of white population lacks the enzyme to
metabolise this drug, therefore will obtain little of no pain relief
Opioid side effects, especially constipation can cause concern
Caution -Number of preparations containing Codeine (in
different combinations)
Lewis-Manning Hospice
Tramadol :
Unusual opioid in that it is thought to provide analgesia via at least two mechanisms. Some
analgesia may be derived from the relatively weak interaction of Tramadol with the Mu
receptor. The second and major mechanism, thought to account for at least 70% of the
medications activity, is via inhibiting the reuptake of noradrenaline and serotonin
Preparations – available in injection and oral form
Immediate release: capsules or dispersible available medication, 50 - 100 mgs QDS
Modified release: capsules
Max dose 400mgs / 24 hours
(NNT 50mgs = 8.3 & 100mgs = 4.8)
Some evidence to suggest it is effective for neuropathic pain
Advantages – said to be absence of tolerance, a lower abuse potential, less evidence of
respiratory depression, less constipation. Although when used in post op setting N&V and
sedation may stil occur
Tramadol may enhance the seizure risk in patients taking monoamine oxidase inhibitors,
neuroleptics or other drugs that lower the seizure threshold in patients with epilepsy so should
Adverse effect – "Seretonin Syndrome": Excess serotonin activity producing a spectrum of
specific symptoms including cognitive, autonomic and somatic effects
Lewis-Manning Hospice
Common Strong Opioid preparations
Lewis-Manning Hospice
Immediate & Modified Release Opioid Preparations
Immediate release
Slow Release (Modified released -12hrly)
General y used for pain of longer duration
Oromorph liquid (10mgs / 5mls)
Sevredol liquid / caps
Oxycodone modified release (OxyContin tabs)
Oxycodone immediate release (Oxynorm liquid /
prescribing is now caps)
required in most
establishments Oxycodone Fentanyl
Patch (not to be used for acute pain) NB: use
blue opioid prescription label
(recent marketing of Abstral – sublingual tablet)
Consultant prescribing only
prescription label
Less common opioid preparations include:
Always refer to BNF if unfamiliar with opioid and equivalent analgesia
Pethidine – not recommended by Pain Specialists
Lewis-Manning Hospice
Strict protocols are in place for the administration of IV Morphine
Refer to: Appendix 2 –Information pack for IV Morphine in acute care areas Appendix 3 – Algorithm for IV Morphine Injectable Drug Administration Policy is available Not recommended for those clinical areas who cannot provide close monitoring
One-to-one care during administration
Strict monitoring of vital signs
Ensure you titrate incrementally to patients response
If IV morphine is not possible then contact medical team to prescribe
an opioid via different route
If there is a requirement for regular IV Morphine then consider an
IVPCA or syringe driver.
IV Morphine for cardiac/chest pain – act under medical team guidance
Lewis-Manning Hospice
Transdermal Opioid patches
(Specialist prescribing)
30 mg per 24hr (previously 60mgs)
60mg per 24hr (previously 100mgs)
(Durogesic or Matrifen)
120mg per 24hr (previously 200mgs
180mg per 24hr(previously300mgs)
240mg per 24hr (previously400mgs)
Buprenorphine Patches
(Partial agonist)
30 – 60 mg per 24hr
Transtec (96hrs)
90 - 120 mg per 24hr
Butrans (7 day patch)
Lewis-Manning Hospice
Opioid patches: Prescribing practice and responsibilities
of the nurse:
Initiating Fentanyl patches should be consultant only
Buprenorphine patches are specialist prescribing only however if patient
already established on Buprenorphine this could possibly be continued.
Refer to trust guidelines: The Policy for Reducing Dosing Errors with
Opioid Medicines in Adults states "In order to ensure good clinical
practice with opioid patches it is necessary to check the patch daily and
document this on the Adult Drug Chart" (Appendix 3)
Prescription labels: transcribed on label is the following instructions:
Each day a nurse must check the applied patch, then write
" patch checked" and initial, in the daily columns on the drug
chart for this prescription. Inform doctor immediately if the
applied patch is wrong strength, missing or duplicated eg. old
patch still applied in addition to current one
This daily patch check is important to avoid possible ineffective
treatment, or severe or even fatal respiratory depression (which has
occurred with opioid patches)
Lewis-Manning Hospice
Diamorphine / Alfentanil
Can be given via various routes but please refer to specialist
If unfamiliar with drug seek advice from Medical personel
Lewis-Manning Hospice
for complications from medical condition or other!
for side effects of drugs ie adverse events
Consider complications from polypharmacy and drug
Use appropriate observation charts, "track & trigger"
Ref: NICE Guidelines 2007 "Acutely ill Patients in Hospital:
Recognition of and response to acute illness in adults in
hospital. Guideline 50.""(Appendix 4)
Lewis-Manning Hospice
Monitoring of Patients
Respond to moderate or severe pain. If
patients continue to experience
unrelieved moderate or severe acute pain
If patients' clinical condition deteriorates
Deteriorating patient : seek senior
Utilise the SBAR
Please use the ABCDE approach to
patients that trigger on their observations
Record triggers and escalations on back
of observation form and in clinical notes
Lewis-Manning Hospice
Calling for HELP! – SBAR
SBAR is an easy to remember mechanism you can use to frame
It is a structured way of communicating information that requires a
response from the receiver
SBAR can be used to escalate a clinical problem that requires
immediate attention or to facilitate efficient handover of patients
SBAR stands for Situation, Background, Assessment, Recommendation
Lewis-Manning Hospice
National Patient Safety Agency
The NPSA document "Reducing Dosing Errors with Opioid Medicines" has highlighted serious patient related adverse events associated with the prescribing, dispensing and administering of opioid medications within the NHS
Opioid patches have contributed to the death of patients around the country. Please read the BNF if unfamiliar with the drug preparation Trust
There have been numerous incidents surrounding poor opioid prescribing, administration and monitoring
The NPSA document is seen as a timely means of instituting change to policies with regard to opioid medicines
Opioid overdose of an opioid-naïve patient
is now classified as a "Never Event" Dept of

Lewis-Manning Hospice
Lewis-Manning Hospice
Naloxone
Naloxone is an Antagonist and reverses opioid side effects
When used to reverse respiratory depression, Naloxone is classified as a "critical
medicine" and therefore should never be delayed as the timeliness of its
administration is crucial to patient safety. When used in this way it does not
necessarily need prescribing as the Dr can prescribe retrospectively on review of
patient There is some evidence to suggest that in smaller doses Naloxone can reduce
pruritus and constipation
Naloxone should only be given for opioid toxicity when the patient is unrousable
and has a respiratory rate of < 8 bpm In some Health establishments Naloxone is being recorded so they can
account for its usage In some health establishments some Incidents of opioid toxicity are being
reported on Datix as a "near miss"
Lewis-Manning Hospice
Management of Opioid toxicity: follow Naloxone administration
Give oxygen via facemask
Classified as a medical emergency. Seek immediate medical assistance
Dilute Naloxone 400mcg in 4mls Normal Saline
Administer Naloxone 100mcg/1ml and await a response in respiratory
rate and sedation
Stay with patient and reassess every 2 minutes
Aim is to reverse adverse side effects of the opioid not analgesia
Sudden reversal is undesirable
NB: Naloxone has a short duration of action
Continue to monitoring closely until Respiratory rate is stabilised
Continuous infusion of IV Naloxone may be required. Refer to Injectable
Drug Administration Policy
Review prescription and consider changing / stopping opioid
Remember is Naloxone being recorded where you work? Record it in
Some patients who have been treated for opioid toxicity have been
reported on Datix as a "near miss" – does this happen at Lewis_Manning?
Lewis-Manning Hospice
Adjuvant analgesics
These are drugs that have other indications for use other than pain but may be used in specific pain circumstances such as neuropathic pain
Neuropathic pain is generally managed with:
Tricyclic-antidepressant – Amitriptyline & Nortriptyline or Duloxetine
Antiepileptic drugs - Gabapentin & Pregabalin
Topical preparations: Lidocaine medicated plasters & Capsaicin cream
Corticosteroid may help to relieve pressure in compression neuropathy
and thereby reduce pain
Recommendation: refer to Senior Clinical Cover for advice if concerns
Neuropathic pain: The pharmacological management of neuropathic pain in adults in non-specialist settings
Issued: March 2010. NICE clinical guideline 96. www.nice.org.uk/cg96
Lewis-Manning Hospice
There are no set of rules about how much pain
patients will experience or how much analgesia
Every patient must be treated as an individual &
their analgesia must be tailored to meet their
"Pain is a more terrible lord of mankind than ever
death itself …. we all die, but if I can save him
from days of torture, that is what I feel is my
great and ever new privilege" (Schweitzer, 1953)
Source: http://lewis-manning.co.uk/wp-content/uploads/2015/01/Lewis-Manning.-The-patient-in-pain.-Module-1.pdf
frauenarzt-boeblingen.de
© Schattauer 2011 Diagnostik und Behandlung des Gestationsdiabetes entsprechend den aktuellsten Leitlinien U. Schäfer-Graf Berliner Diabeteszentrum für Schwangere, Klinik für Gynäkologie & Geburtshilfe, St. Joseph Krankenhaus Keywords Definition Gestationsdiabetes, Insulinresistenz in der Gestational diabetes, insulin resistance in
bio-qualys.com
Cher confrère, Marcq-en-Barœul, le 6 Juin 2016 Recommandations 2016 pour les voyageurs Zika, sexe et moustiques…voilà l'été Zika s'ajoute à la liste des arbovirus, après la dengue et le chikungunya, dans les recommandations sanitaires 2016 pour les voyageurs. Santé publique France insiste aussi dans le Bulletin épidémiologique hebdomadaire sur la prévention contre le paludisme et la fièvre jaune dans les zones d'endémie ainsi que les infections sexuellement transmissibles. « L'infection à virus Zika est venue s'ajouter à la liste de plus en plus longue des infections émergentes à prendre en compte au retour de voyage », expliquent les Pr Éric Caumes et Daniel Camus, président et vice-président du Comité des maladies liées aux voyages et des maladies d'importattion (CMVI). « Le risque de malformations neurologiques d'importance a été estimé à 1 % des grossesses de femmes infectées » soulignent-ils dans le dernier numéro du « BEH » consacré aux recommandations sanitaires pour les voyageurs. Elles invitent les femmes enceintes au report de tout voyage en zone d'épidémie et, aux femmes vivant en zone d'épidémie et aux voyageuses en âge de procréer qui s'y rendent, de différer tout projet de grossesse tant que l'épidémie est active. Le bulletin précise que l'infection par cet arbovirus de la même famille que la dengue et la fièvre jaune se révèle asymptomatique dans 70 à 80 % des cas. Et quand les symptômes sont présents, la présentation clinique est fruste, pouvant associer, à des degrés divers, arthralgies, œdèmes des extrémités, fièvre modérée, céphalées, douleurs rétro-orbitaires, hyperhémie conjonctivale et exanthème maculo-papuleux. Les signes persistent de 2 à 5 jours. Toute personne de retour depuis moins de 15 jours d'une zone endémique et présentant au moins un des symptômes associés au Zika doit être signalée à l'ARS et faire l'objet d'une demande de confirmation biologique.