Opmaak
07-prior:Opmaak 1 20/06/11 09:51 Pagina 109 F, V & V IN OBGYN, 2011, 3 (2): 109-120 Viewpoint Progesterone for Symptomatic Perimenopause Treatment –Progesterone politics, physiology and potential for peri-
menopause
Professor, Endocrinology, University of British Columbia, and Vancouver Coastal Health Research. Institute, Vancouver,Canada V5Z 1M9. Scientific Director, Centre for Menstrual Cycle and Ovulation Research (www.cemcor.ubc.ca). Correspondence at: Professor J. C. Prior, Suite 4111, 2775 Laurel Street, Division of Endocrinology, Department of Medicine, University of British Columbia and Vancouver Coastal Health Research Institute, Vancouver, BC V5Z 1M9.
Telephone (604) 875-5927, Fax (604) 875-5915; email [email protected]; websites: www.cemcor.ubc.ca andwww.estrogenerrors.com Perimenopause, women's normal midlife reproductive transition, is highly symptomatic for about 20% of womenwho are currently inaccurately counseled and inappropriately treated with oral contraceptives, menopausal hormonetherapy or hysterectomy. About 80% of perimenopausal women experience vasomotor symptoms (VMS), 25% havemenorrhagia, and about 10% experience mastalgia. The majority of women describe varying intensities of sleep, coping or mood difficulties. Women are more symptomatic because common knowledge inaccurately says that estra-diol (E2) levels are dropping/deficient. Evidence shows that with disturbed brain-ovary feedbacks, E2 levels average26% higher and soar erratically – some women describe feeling pregnant! Also, ovulation and progesterone (P4) levelsbecome insufficient or absent. The most symptomatic women have higher E2 and lower P4 levels. Because P4 and E2 complement/counterbalance each other's tissue effects, oral micronized P4 (OMP4 300 mg at bedtime) is a physiological therapy for treatment-seeking, symptomatic perimenopausal women. Given cyclically(cycle d 14-27, or 14 on/off) in menstruating midlife women, OMP4 decreases cyclic VMS, improves sleep and pre-menstrual mastalgia. Menorrhagia is treated with ibuprofen 200mg/6h plus OMP4 cycle d 4-28. For insulin resistance,metformin plus cyclic or daily OMP4 decreases insulin resistance and weight gain. Non-responsive migraines needdaily OMP4 plus usual therapies. VMS and insomnia in late perimenopause respond to daily OMP4. In summary, OMP4is a physiology-based therapy that improves sleep, treats VMS, does not increase breast proliferation or cancer risk,increases bone formation and has beneficial cardiovascular effects. A controlled trial is testing OMP4 for peri-menopausal VMS – more evidence-based data are needed.
Key words: Perimenopause, vasomotor symptoms, night sweats, menorrhagia, sleep disturbance, anovulation, shortluteal phase, ovulatory disturbances, oral micronized progesterone, treatment, midlife women, estradiol levels, progesterone levels, infertility, nausea, migraine headaches, mastalgia, insulin resistance, osteoporosis, rapid boneloss, cardiovascular disease, breast cancer, estradiol-progesterone tissue interactions, self-actualization, feminism,history.
She is weeping and her normally attractive face has Your medical record shows that Emily, we'll call her, become twisted and swollen – almost inarticulate, she is 44 years old, apparently happily married, with a complains of extreme fatigue, flooding menstruation son in high school and a daughter in her early teens.
and night sweats robbing her of sleep. She is a social worker and a community leader in You have delivered her two babies and done her yearly your moderate-sized city. She has always been a Pap tests, but the woman in front of you seems a
stranger. What has changed? Why is she so miser-
vibrantly well woman in exceptional health who eats well, doesn't smoke and exercises regularly.
07-prior:Opmaak 1 20/06/11 09:51 Pagina 110 You're puzzled over Emily's current situation.
cultural and pharmaceutical reasons, perimenopause You inquire about her husband, her children – she and menopause came to be seen as a single, homo - mumbles and then vehemently snorts, "They're
genous downhill slide into waning hormones, loss of health and decreased attractiveness. "How are your periods besides the heavy flow?" Emily's symptoms don't make sense within this you ask. "Spot on regular!" she retorts, "That's current view of midlife's decreasing hormone levels what's so frustrating – maybe a bit shorter, about – with her shorter cycles and heavy flow she is highly unlikely to have deficient estradiol levels.
"I don't have a clue what's happening." She goes However, if her estradiol levels are not low, why is on. "I don't feel like myself – when do I get my life
she having night sweats? Before addressing these questions about what is causing Emily's symptoms let's start with current Midlife women all over the world are similarly official ideas. The North American Menopause challenging their gynaecologists. They want help to Society (NAMS) website says, "The years between understand the changes they are experiencing, some puberty (when periods start) and menopause are idea of the time course of these changes and, only called premenopause." (http://www.menopause.org/ occasionally, do they want and need some therapeu- expertadvice.asp). This statement totally eliminates tic intervention. The purpose of this review is to first any midlife transitional phase. identify the current concepts, policies and politics In the next sentence, however, NAMS contradicts that prevent many of us, as physicians, from under- that earlier sentence by saying: "Physical signs of standing our midlife patients' concerns. I will define menopause begin many years before the final and describe the phases of the long and varying per- menstrual period. This menopause transition phase imenopausal transition. Then I will reframe peri- is called perimenopause (literally meaning ‘around menopause physiology in a new and hormonally more accurate manner before embarking on my Did you notice? In that NAMS quotation the primary purpose – describing the evidence that oral word, "menopause," means two different things – in
micronized progesterone therapy is safe, appropriate the phrase, "physical signs of menopause," the word and effective for those (relatively few) symptomatic means (as the average woman defines menopause) perimenopausal women who require medical inter- everything changing and symptomatic in midlife.
However, in the phrase, "around menopause," the My perspective is that of an endocrinologist who, gynaecological definition of menopause is used, herself, suffered a long, perplexing and highly meaning the literal last menstrual period. If this is symptomatic perimenopause. I am also a clinician- not confusing enough, there is yet a third, epidemi- scientist, doing epidemiological, clinical observa- ological, meaning of menopause (and this is how I tional and randomized controlled trial research on will consistently use the word in this paper) – perimenopause. In the early 1990s, despite my train- menopause is the normal woman's life phase that
ing and roles, I like Emily, struggled to understand begins one year after the last menstruation (and is the changes I personally experienced – I found the sometimes called "postmenopause"). Thus the hormonal changes to be the opposite of what I had confusing use of two key words (menopause and been taught and always thought; instead, estradiol perimenopause) in official documents, rather than erratically soared and progesterone progressively helping Emily understand what is happening to her, decreased. Before we get to that, however, we must illustrate the unhelpfully inconsistent messages first review how we got to a situation where Emily medicine and gynaecology are giving about is seeking yet not finding help. Historical and Medico-political Context of Peri-
Timelines and Definitions
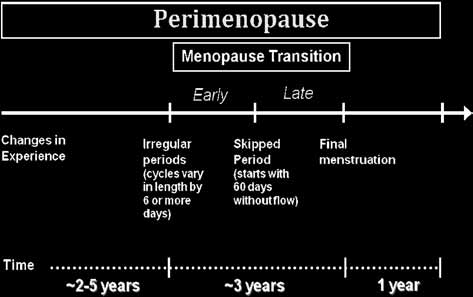
I will clarify how I use language describing the With the discovery of estradiol in the mid-1920's transition between fertile cycles and menopause by came the concept that it was the female hormone
showing a diagram that incorporates the latest evi- (Oudshoorn, 1994; Baxter and Prior, 2009) and that dence defining the phases of this midlife transition.
all symptomatic women must be "estrogen defi- It uses the world-wide epidemiology/cohort-based cient." Given the model of puberty, we would expect data from the ReStage Collaboration to refine the a long biological transition between potentially re- onset of the Early Menopause Transition (Harlow et productive, menstruating premenopausal and al., 2008), and the onset of the Late Menopause ‘hormonally deficient' menopausal women. But for Transition (Harlow et al., 2006), of the Stages of F, V & V IN OBGYN
07-prior:Opmaak 1 20/06/11 09:51 Pagina 111
production within a shorter follicular phase (Landgren et al., 1980).
The early menopause transition as shown in
Figure 1 requires cycle variability of +/- 6 days (Harlow et al., 2008). Women often describe thisvariation as "irregular" cycles but they also may notnotice this degree of variability (given that 29% of apopulation-based sample of women experience atleast one cycle-to-cycle length variability of 14-daysa year (Munster et al., 1992) and some women maynever have established, nor learned to recognize, regular cycles.
Fig. 1. — The ReSTAGE Collaboration refinements of the
Women begin the late menopause transition with
Stages of Reproductive Aging Workshop (STRAW) definitions
60 days between flow episodes or what women
of the phases of midlife. The estimated timelines are based onextensive clinical experience (Prior, 2010).
commonly call a "skipped period" (Harlow et al.,2006). Note that, in neither the early nor latemenopause transition did the ReStage investigatorsfind that the elevated FSH levels required by
Reproductive Aging Workshop (STRAW) definitions
STRAW (Soules et al., 2001) contributed to the
(Soules et al., 2001) of the menopausal transition
menstrual cycle-based classification (Harlow et al.,
and perimenopause.
2006; Harlow et al., 2008) and thus routine cycle day
Early perimenopause, before the irregular or
3 FSH testing to determine perimenopausal status is
skipped cycles of the menopause transition begin, is
not cost-effective. The late perimenopause, meaning
characterized by a several-year stretch of changes in
the time from the final menstruation until
experience without any cycle interval changes (Prior,
menopause, is a year during which women's breast,
2005a). In my view, this is the most frustrating and
heavy flow and premenstrual symptoms have
symptomatic time for many women. Evidence shows
improved but hot flushes and sleep problems are
that hormone levels have already changed although
commonly worsening, but alternatively may be
regular cycling hasn't. For these reasons, a series of
decreasing (Dennerstein et al., 2000).
experience-changes, any three of which a woman no-tices, can be used to make a "diagnosis" of the onset
Current Evidence for the Hormonal Changes of
of early perimenopause (Table 1) (Prior, 2005a).
Emily, the highly distraught woman whose story
began this paper, is clearly in early perimenopause
Symptomatic parous women often describe feeling
because she is miserable with heavy flow (#1 in
pregnant during perimenopause. I had such a vivid
Table 1), has regular but shorter cycles (#2) and is
dream in early perimenopause – when I described it
suffering with night sweats (#6). Evidence suggests
to an audience of midlife women someone at the
that the shorter cycle lengths documented with re-
back hollered, "That's not a dream, it's a night-
productive aging (Vollman, 1977) are associated
mare!" Likewise, a hunter-gatherer !Kung woman of
with, and are likely caused by, higher cycle estradiol
the Kalahari desert told her anthropologist inter-viewer: "Not long ago I had a dream that I was pregnant. I thought, ‘What? Haven't I stoppedmenstruating?'" (Shostak, 1981). At the time Nisawas thought to be in her early 50s and from her
Table 1. — A ‘diagnosis' of early perimenopause can be
made in midlife women who continue to have regular
description, was in late perimenopause (Fig. 1).
flow if they are experiencing – any 3 of these nine
Likewise, in the introduction to her book, "Under-
experience changes.
standing Menopause" activist Canadian sociologist
also reported feeling pregnant during perimenopause
1. New onset heavy and/or longer flow
(O'Leary Cobb, 2005). Why did all of us, culturally,
2. Shorter menstrual cycles (≤ 25 days)3. New sore, swollen or lumpy breasts
ethnically and economically very different midlife
4. New mid-sleep wakening
women, report feeling pregnant? I believe it is
5. Increased cramps
because we all were experiencing the sore breasts,
6. Onset of night sweats, in particular premenstrually
weight gain, bloating and other high estrogen
7. New or markedly increased migraine headaches
symptoms that are common in perimenopause and
8. New / increased premenstrual mood swings9. Weight gain without changes in exercise or eating
in pregnancy. Our subconscious minds told us whatour physicians didn't.
P4 FOR SYMPTOMATIC PERIMENOPAUSE – PRIOR 111
07-prior:Opmaak 1 20/06/11 09:51 Pagina 112
Fig. 2. — The cross-sectional mid-follicular phase estradiol levels by menstrual cycle characteristics in menstruating women ages 45-
55 randomly selected and enrolled in the Melbourne Midlife Women's Health Project baseline data – annotated by including the mean
E2 level for premenopausal follicular phase women from the Burger lab as the lower horizontal line (surrounded +/- one SD by yellow
colour), and the second horizontal line as the mean E2 peak level (orange). Above that are very high E2 levels importantly higher than
ever seen during normal premenopausal menstrual cycles (red). Reprinted from Burger et al. (1995) with adaptations by the author.
Reliable evidence about the hormonal changes of
data and was flabbergasted and angry that the
perimenopause was absent from the medical litera-
authors did not see the high E2 levels in their data.
ture until the mid-1990s, not only because peri-
So, with colleagues, I challenged in a letter to the
menopause and menopause were subsumed into the
editor "that the data be allowed to speak" (Prior et
same process, but perhaps also because no question-
al., 1996). Burger and colleagues responded by
naires about "menopause" included questions about
admitting that perimenopausal "estradiol levels are
either flow or breast tenderness which are clinically
preserved. ." (Burger, 1996).
important and distinctive for perimenopause. The
These illustrative but traditionally interpreted
first, population-based data of follicular phase estra-
population data, however, were quickly followed by
diol (E2) levels in menstruating Melbourne Australia
confirmatory cross-sectional data, this time urinary
women ages 45-55 were cross-sectional with data
hormone levels across one cycle in women younger
segregated by menstrual cycle characteristics (I =
than 37 years old with regular cycles compared with
regular cycles, interpreted as "premenopausal"; II =
symptomatic menstruating women older than age 37
changes in flow; III changes in cycle interval; IV
(Santoro et al., 1996). These data showed that estro-
changes in both flow and cycle interval; IV no flow
gen excretion products were significantly higher and
for 3-11.9 months) (Burger et al., 1995). Figure 2
pregnanediol levels were importantly lower in the
shows that early follicular phase (cycle days 3-8)
perimenopausal women. These authors recognized
fasting E2 levels had a large variance but the majority
the uniqueness of their observation and clearly re-
fell outside of the plus/minus 1 SD of the fasting nor-
ported the higher estradiol level they observed.
mal range (yellow). Note the number of women in
I subsequently performed a meta-analysis of
all phases (I-V) whose E2 levels are extremely high
within-centre pre- versus perimenopausal serum
estradiol levels that showed, in perimenopausal
In reporting these results, the authors did not
women (n = 415) in the follicular phase E2 levels
describe observing higher than expected estradiol
were 225 pmol/L versus 175 pmol/L in premeno -
levels (Burger et al., 1995). Moreover, their abstract
pausal women (n = 276; Fisher's F = 16.12,
says: "We conclude that an increase in serum FSH
P = 0.041) (Prior, 1998). The premenstrual or luteal
and decreases in E2 and Inhibin are the major en-
phase E2 levels were also significantly higher in
docrine changes cross-sectionally during the
perimenopausal and than in premenopausal women
menopausal transition" (author's emphasis). I
– in perimenopausal women (n = 69) mean E2 levels
immediately recognized myself in these hormonal
were 374 pmol/L compared with 300 pmol/L in
F, V & V IN OBGYN
07-prior:Opmaak 1 20/06/11 09:51 Pagina 113
premenopausal women (n = 290; Fisher's F = 15.46,
matic perimenopause it is necessary to see estradiol
P = 0.016) (Prior, 1998). Most recently two reports
and progesterone and their interactions as I do. Estra-
from a systematic 2-cycle thrice weekly serum hor-
diol has generally been considered the predominant,
mone study in midlife women of every STRAW
most important woman's reproductive hormone and
stage compared with mid-reproductive aged women
‘what makes a girl, a girl' (Baxter and Prior, 2009).
confirmed the higher estradiol levels, lower proges-
Progesterone – only produced after a midcycle E2
terone levels (Hale et al. 2007) and showed atypical
peak and the LH peak it subsequently triggers – is
secondary estradiol peaks called "luteal out of
present for fewer than half of all menstrual cycle
phase" or LOOP events within the luteal phases of a
days. However, P4 is secreted in extremely high quan-
third of all cycles from women in the menopausal
tities (reported as nmol versus estradiol's pmol), ris-
transition (Hale et al., 2009). Therefore, evidence
ing 1400 percent above its low follicular phase
from multiple continents and many different re-
levels; midcycle maximum E2 levels, by contrast, rise
searchers confirms what perimenopausal women's
only 220 percent above its low during flow (Nielsen
experiences (shorter cycles, heavy flow, breast ten-
et al., 1990). Progesterone production is dependent
derness, weight gain, insulin resistance and feeling
on preceding E2 production. However, nature does
pregnant) are telling them – they are experiencing
not spend energy making large quantities of non-
higher estradiol levels.
essential hormones. Thus high levels of P4 for at least
Why are these paradoxical increased estradiol lev-
10 days per cycle appear necessary to counter-
els occurring in women whose ovaries are running
balance or complement estradiol's powerful and
out of follicles (Richardson et al., 1987)? Evidence
essential growth-stimulating actions (Graham and
suggests that inhibin B levels (Burger et al., 1998)
Clarke, 1997). To provide a few reproductive
decrease thus allowing small increases in FSH levels
examples of estradiol-progesterone partnerships: E2
which, in turn, recruit more follicles each of which
stimulates cervical gland production of slippery,
can make estradiol and even stimulate non-typical
clear mucus to aid sperm transit while P4 inhibits cer-
additional waves of follicle maturation (as in LOOP)
vical mucus production; E2 stimulates breast glandu-
cycles (Hale et al., 2009). Furthermore, these higher
lar development in puberty (Tanner stages I-III)
estradiol levels do not reliably suppress FSH levels,
while P4 (plus E2) is required for final breast matura-
at least partly because of decreases in inhibin B
tion to Tanner stages IV-V as the areolar diameter
(Klein et al., 1996; Prior, 1998).
expands and the ductal system and nipple mature
The decreasing progesterone production across
(Prior et al., 1989); both E2 and P4 induce intermedi-
the menopausal transition (Santoro et al., 2008)
ate cell vaginal maturation – 12-mo. following pre-
(Prior, 2002b) is also related to disturbed hypo -
menopausal ovariectomy during randomized
thalamic-pituitary-ovarian feedback loops so that
double-blind treatment with conjugated equine es-
estradiol peaks can occur and not be followed by LH
trogen (CEE, 0.6 mg/d) or medroxyprogesterone
peak levels; both estradiol and LH peak levels can
(MPA, 10 mg/d) the majority of cells were interme-
also occur and not be followed by ovulation (Weiss
diate cells, although CEE produced significantly
et al., 2004) although the complete physiological
more superficial cells (Prior et al., 1994). E2 and P4
reasons for these observations are not yet clear. In an
work together in normal bone remodelling so that
earlier as well as a recent study of daily urinary hor-
estradiol reduces bone resorption while progesterone
mone levels, perimenopause is a time of unopposed
stimulates bone formation (Prior, 1990; Seifert-
and higher estrogen production often without coun-
Klauss and Prior, 2010). In two randomized
terbalancing ovulatory progesterone production
controlled human trials with breast biopsy cellular
(Metcalf and MacKenzie, 1985; O'Connor et al.,
changes as the primary objective, topical estradiol
caused breast epithelial cell proliferation while
These multiple physiological ovarian hormonal
progesterone decreased it (Chang et al., 1995;
(higher estradiol and FSH levels, lower inhibin B and
Foidart et al., 1998). In addition, the large French
progesterone levels) and hypothalamic-pituitary-
cohort study (E3N) shows estradiol treatment to be
ovarian feedback disturbances to me represent a
associated with a 29% increased risk for breast
planned way of ending the potential for menstruation
cancer compared with untreated menopausal
and pregnancy as women become menopausal.
women, estrogen plus progestin increased risk by69%, but estrogen with progesterone had no in-
The Physiological Rationale for Progesterone
creased breast cancer risk (HR 1.0, 95% CI 0.82,
Treatment of Symptomatic Perimenopause
1.22) (Fournier et al., 2008). In the vascular endothe-lium, both E2 and P4 similarly increase endogenous
In order to understand why I consider progesterone
nitric oxide activity to improve blood flow (Mather
an important, safe and effective therapy for sympto-
et al., 2000). In the brain, estradiol is neuroexcitatory
P4 FOR SYMPTOMATIC PERIMENOPAUSE – PRIOR 113
07-prior:Opmaak 1 20/06/11 09:51 Pagina 114
and supported the probable safety of progesteronetherapy, I need to indicate why I consider the currentrecommendations that symptomatic perimenopausalwomen be treated with oral contraceptives ormenopausal type hormone therapy (National Insti-tutes of Health 2005) to be inappropriate and unsafe.
Given the feedback disturbances of perimenopause,it is likely that exogenous estrogen will not reliablysuppress endogenous (often high) E2 levels. Oralcontraceptives have not proven more effective thanplacebo for hot flushes in a controlled trial (Casperet al., 1997). In addition, new retrospective clinicaldata suggest breast cancer in women who weretreated in perimenopause with menopausal-type hor-mone therapy show a trend toward decreased time tobreast cancer progression and decreased overall sur-vival (P = 0.06) (Baumgartener et al., 2011). Thusoral contraceptives and hormone therapy do not ap-pear to be effective nor safe in perimenopause.
We can now begin to describe clinical data and
minimal evidence-based material available suggest-ing that progesterone is an appropriate and effectivetherapy for symptomatic perimenopause. (I addedthe adjective, "symptomatic" because peri-menopause is a normal life phase and only a smallpercentage of women need or want any medicaltreatment.)
Oral Micronized Progesterone Treatment for
Symptomatic Perimenopause
Before describing specific uses for progesterone, it
Fig. 3. — Bark painting by an aboriginal man in Australia
is useful to provide some general clinical guidelines.
depicts two stylized snakes intimately entwined. This is a photo
I think of progesterone as counterbalancing the
of art that the author purchased in Western Australia. The artist'sidentity is unknown.
tissue effects of high estrogen – given the feedbackdisturbances, it is not realistic to expect that proges-terone will suppress endogenous E2 production in
while progesterone inhibits this action, improves
perimenopause. When I say "progesterone" I mean
sleep and decreases addictive behaviours and anxiety
the molecularly identical hormone to that produced
(Gibson et al., 2009). Thus my vision is that estradiol
by the corpus luteum and not progestins. I always
and progesterone are both important for normal
recommend oral micronized progesterone (OMP),
physiology; they act together in all reproductive and
rather than transdermal progesterone for peri-
non-reproductive tissues (bone, blood vessels, brain)
menopausal women. The primary reason is that I
and are as closely tied together as the two snakes in
have experience with it – however I think trans -
this Australian aboriginal bark painting (Figure 3).
dermal progesterone may not be "strong enough" to
In addition, based on the above physiology, oral
effectively counterbalance the tissue effects of high
micronized progesterone appears safe for peri-
estrogen levels, and furthermore it has no beneficial
menopausal women – it should decrease their risks
effect on sleep disturbances that are common in
for endometrial cancer, does not show any indication
perimenopause. OMP can either be prescribed as a
of increasing venous thromboembolism risk, causes
formulary drug, or where that is not available,
women to burn 300 more kilocalories/day so will
compounding pharmacists can make it up in olive oil
help prevent rather than causing weight gain (Barr
(which is similarly well absorbed based on my
et al., 1995b) and decreases anxiety and doesn't
clinical serum tests).
cause depression (Dennerstein et al., 1985).
A physiological luteal phase dose of OMP is
Having explained the changing physiology of peri -
300 mg at bedtime – this keeps the P4 blood level
menopausal hormonal levels and feedback systems,
above a luteal phase threshold for 24 hours (Simon
F, V & V IN OBGYN
07-prior:Opmaak 1 20/06/11 09:51 Pagina 115
et al., 1992). OMP must be taken at bedtime because
its beneficial sleep enhancing effects (Schussler et
al., 2008) would cause drowsiness or almost "intox-
icated" feelings if taken when awake. To be cautious,
especially for sleep-deprived and thin women, I rec-
ommend they begin OMP on a night following
which they can sleep in. Otherwise catch-up rapid-
eye-movement sleep may make them feel that OMP
caused a "hang-over". These morning sleepy feel-
ings, if present, do not persist more than a few days.
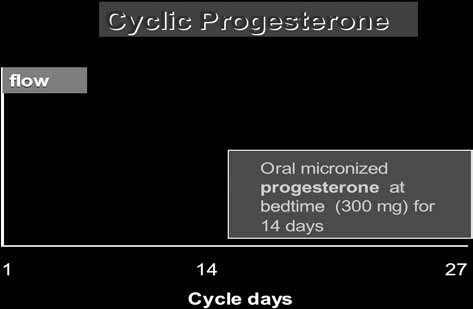
Finally, the schedule of OMP depends on
women's bleeding pattern, her desires for fertility,and whether or not she gives a history of migraine
Fig. 4. — Graph depicting the idealized regular 28-day men-
headaches. (I'll discuss the use of cyclic OMP to aid
strual cycle showing on which cycle days to prescribe 300 mg
perimenopausal fertility later.) For women with daily
of oral micronized progesterone at bedtime to provide "lutealphase replacement" progesterone therapy for treating sympto-
symptoms such as night sweats or hot flushes, espe-
matic perimenopausal women (http://www.cemcor.ubc.ca/
cially if they have irregular or skipped cycles, I pre-
scribe OMP daily. For women with regular cycles,
unless they have migraines, I always start with cyclicOMP as shown in Figure 4 (http://www.cemcor.ubc.
ca/help_yourself/articles/cyclic_progesterone
therapy). Women with migraine headaches are sen-
daily_diaries), I provide women with this practical
sitive to a host of changes thus, although OMP does
lay language handout: (http://www.cemcor.ubc.ca/
not cause migraines, its withdrawal can trigger them.
For migraneurs I always also prescribe daily OMP
I always begin therapy with an over-the-counter non-
even if they are regularly cycling – daily OMP will
steroidal anti-inflammatory (NSAID) drug such as
make perimenopausal flow light but usually doesn't
ibuprofen. NSAIDs restore a normal balance of en-
entirely prevent periods.
dometrial prostaglandins and thus cause a 25-50%decrease in flow (Lethaby et al., 2002) – I believe
Progesterone for heavy or prolonged flow
NSAIDs should be taken on all heavy flow days bywomen of all ages. For ibuprofen, the dose is 200 mg
In my experience, heavy flow occurs in all phases of
(with food) every 4-6 hours while awake.
perimenopause and is experienced by about 25% of
In addition to ibuprofen I use cyclic OMP (Fig-
all midlife women. (Heavy flow was not included in
ure 4) treatment for all perimenopausal women with
the questions asked in the Melbourne Midlife
regular cycles and the recent onset of heavy flow. I
Women's Health Study therefore we have no popu-
would continue ibuprofen and cyclic OMP for at
lation-based prospective data). The usual gynaeco-
least three cycles. If, as often happens, flow starts
logical approach to heavy bleeding is to assume
while the 14 days of OMP therapy are still being
fibroids or other pathology – it is far more likely,
taken, the full OMP duration should always be com-
however, that heavy flow is related to the disturbed
pleted. The flow-start day is called a new Day 1 –
ovarian hormonal physiology of perimenopause.
OMP is started on the next cycle day 14, even if that
Therefore, for perimenopausal women I don't rec-
gives only a few days off progesterone each cycle.
ommend endometrial biopsies or ultrasounds or
However, if I see a perimenopausal woman who
screening for bleeding disorders unless at least three
has had heavy flow for months, in addition to assess-
cycles of ibuprofen plus progesterone therapy have
ing for and treating anemia, I will usually start long-
not importantly improved the abnormal bleeding. All
cycle OMP – this means prescribing OMP for cycle
evidence, especially this case-control clinical study
days 4-28, along with ibuprofen as described above.
(Moen et al., 2004) ] strongly suggest that the higher
In my clinical experience, even in women with doc-
E2 and lower P4 levels typical in perimenopause
umented bleeding disorders, long-cycle OMP plus
cause the heavy flow. This suggests that OMP, which
ibuprofen therapies are usually effective. The natural
stabilizes the endometrium and, when given in long
history of heavy flow in perimenopause is that it im-
cycles, thins it, would be a beneficial therapy.
proves over time and the closer a woman becomes
Once I have a clear understanding of a woman's
to menopause. Therefore OMP and ibuprofen are
heavy flow experience (hopefully from Daily Peri-
temporizing measures. If these are not sufficient, my
menopause Diary records (Hale et al., 2003) that are
next approach is to recommend the levonorgestrel
downloadable from the CeMCOR website
impregnated IUD (LNG-IUD) (Irvine et al., 1998).
P4 FOR SYMPTOMATIC PERIMENOPAUSE – PRIOR 115
07-prior:Opmaak 1 20/06/11 09:51 Pagina 116
Obviously the LNG-IUD would be an earlier choice
disturbance typically occurs in three different pat-
if the perimenopausal woman with heavy flow had
terns: increased trouble falling asleep, early morning
no night sweats, breast tenderness or other experi-
wakening or, as is most common, abrupt waking
ences that may be helped by the physiological ac-
after a few hours of deep sleep. Perimenopausal
tions of OMP, and she also had practical access to it
women commonly, as did Emily, describe disturbed
(despite its high cost in some jurisdictions).
sleep as something that is troublesome for them and
One or all of the above mentioned measures to
for which they seek treatment.
treat perimenopausal menorrhagia are almost always
Oral micronized progesterone is rapidly converted
successful – in my practice, perimenopausal women
in the brain into allopregnanolone which acts
with heavy menstrual flow or flooding almost never
through the GABAA receptors to decrease anxiety
needed endometrial ablation or hysterectomy. Al-
and induce sleep (Friess et al., 1997). Randomized
though Cochrane reviews and randomized controlled
double blind cross-over trials in men (Friess et al.,
trials support the use of ibuprofen and cyclic or long-
1997) and menopausal women (Schussler et al.,
cycle progestins for heavy flow, there are no data of
2008) clearly document significant increases in early
which I'm aware that have studied OMP for peri-
rapid-eye movement sleep, decreased sleep interrup-
menopausal heavy flow.
tion and no changes in morning neurocognitive func-tion (Schussler et al., 2008). Therefore, OMP is an
effective and evidence-based treatment for sleep dis-turbances, although it has not yet been proven effec-
Unless cycles become consistently less than 21 days
tive in perimenopause. Note that usually sleep
apart, these usually do not require any therapy. How-
disturbances are associated with other experience
ever, often the shorter cycles are associated with in-
changes such as night sweats. I usually don't pre-
creased premenstrual symptoms, breast tenderness
scribe OMP only for sleep problems.
or heavy flow, and these need treatment. If cycles areroutinely less than 21 days apart I suggest cyclic
Increased Dysmenorrhea or Cramps
OMP as described above but beginning two days earlier and taken on cycle days 12-25.
In my experience perimenopausal cramps respondwell to intense ibuprofen prophylaxis in women
Breast Tenderness and/or Swelling and Nodular-
without a history of persistent severe cramps or en-
dometriosis. This handout for women describes theearly and repeated use of ibuprofen to stay ahead of
Breast tenderness is a symptom for 33% of early
the symptoms and thus prevent the pain-causing
perimenopausal women and decreases as cycles
build-up of prostaglandins (http://www.cemcor.ubc.
become irregular (Dennerstein et al., 2000). Clinical
evidence based on daily diary records suggests that
if perimenopause causes a flair of endometriosis
breast tenderness does not occur unless E2 levels ex-
symptoms, then I have found that daily OMP is ef-
ceed the usual midcycle peak values. Some non-pub-
fective along with ibuprofen therapy. As opposed to
lished data show that women with breast tenderness
premenopausal women, daily OMP will not suppress
have increased breast cell proliferation (Anne
estradiol levels and therefore inducing rapid bone
Gompel, 2011, personal communication). Given that
loss is not a concern.
progesterone decreases breast cell proliferation(Chang et al., 1995; Foidart et al., 1998), cyclic
Night Sweats and Hot Flushes
OMP is likely to be effective therapy for breast tenderness occurring, as it commonly does, premen-
Ten percent of women ages 45-55 with regular men-
strually (Hale et al., 2003). Unfortunately, no con-
struation report night sweats and ten percent hot
trolled trial data are available to document that OMP
flushes (Dennerstein et al., 2000). Often these night
causes significant symptomatic improvement of
sweats have a cyclic pattern and cluster around flow
breast tenderness although the trend in a small cross-
(Hale et al., 2003). However, at present it is unclear
over trial was toward less tenderness (Dennerstein et
how to treat vasomotor symptoms (VMS) in peri-
al., 1985).
menopausal women – estrogen-based treatments arethe gold standard for menopausal women (MacLen-
Mid-sleep Wakening or Sleep Disturbances
nan et al., 2004) but perimenopause has a differentphysiology. Although oral contraceptives and
Sleep disturbances occur in 31% of early peri-
menopausal type ovarian hormone therapy are both
menopausal women and increase to 38% in late
currently advocated for VMS treatment (National
perimenopause (Dennerstein et al., 2000). This sleep
Institutes of Health, 2005), a randomized controlled
F, V & V IN OBGYN
07-prior:Opmaak 1 20/06/11 09:51 Pagina 117
trial of 20 mg ethinyl estradiol oral contraceptive
or tricyclic anti-depressants that are often used). In
showed no meaningful improvement versus placebo
addition, most perimenopausal women with mi-
in perimenopausal women (Casper et al., 1997). Al-
graines are also symptomatic with other experience
though there are no such controlled trial data for the
changes that OMP will likely help.
use of menopausal ovarian hormone therapy forVMS in perimenopause, epidemiological data sug-
Perimenopausal Premenstrual and Mood Symp-
gest VMS don't improve during estrogen-based
treatment until women become menopausal (Jo-hannes et al., 1994).
Premenstrual symptoms are of obscure etiology in
A recent randomized controlled trial showed that
premenopausal women (Harvey, 2009) but clearly
OMP was effective for both daytime and night VMS
increase in perimenopause, and typically become
in healthy early menopausal women (Prior and
most evident in women with regular cycles. Approx-
Hitchcock, 2010). The mechanisms through which
imately 30 percent of women across perimenopause
OMP helps VMS are not known, but probably in-
reported depression and "nervous tension" experi-
volve actions in the hypothalamus, on temperature
ences in the last two weeks (Dennerstein et al.,
centres and by decreasing neuroexcitotoxicity and
2000). What is even more fascinating is that women
inflammation in the brain (Gibson et al., 2009). The
who reported PMS when they still had regular cycles
Centre for Menstrual Cycle and Ovulation Research
were more likely to later experience night sweats and
has just secured Canadian Institutes for Health Re-
VMS (Morse et al., 1989). It makes most sense to
search funding to perform a similar trial in 175 per-
me that women with a genetic or other predisposition
imenopausal women. This trial will use daily OMP
to estrogen sensitivity will develop increased breast
(to avoid the problems of heavy bleeding or need to
tenderness, bloating, inappropriately increased
exclude migraneurs) and stratify women into "early
appetite and mood symptoms premenstrually in
perimenopause" if they have not had a 60-day cycle
perimenopause as they experience higher E2 and
and "late perimenopause" if they have. Results are
lower P4 levels (Prior, 2002a). Calcium carbonate
not expected until at least 2014.
supplementation is the only evidence-based treat-
In the mean time, extensive clinical evidence says
ment for premenopausal premenstrual symptoms
that OMP is effective for perimenopausal VMS. In
(Thys-Jacobs and Alvir, 1995; Douglas, 2002). How-
addition, it improves the sleep disturbances with
ever, women with severe depression that has a pre-
which night sweats are often associated. Cyclic
menstrual exacerbation will be helped by serotonin
OMP is effective for cyclic night sweats in regularly
reuptake inhibitors (Douglas, 2002). Cyclic OMP
cycling early perimenopausal women. However,
may be an appropriate treatment for women who
once VMS occur more consistently across the cycle,
have become unable to cope because of combined
as often happens by the early menopause transition,
sleep disturbances, night sweats and breast tender-
daily OMP is then necessary.
ness with or without premenstrual mood swings.
Again, although there are numerous negative trials
of cyclic progesterone for premenstrual symptomsin premenopausal women with premenstrual symp-
Headaches are common in perimenopause and 32-
toms (Douglas, 2002), none to my knowledge have
36% of perimenopausal women across all phases re-
been performed in perimenopause. However, I have
port their experience in the last two weeks
never prescribed cyclic OMP only for premenstrual
(Dennerstein et al., 2000). Migraine headaches may
mood symptoms.
occur for the first time in perimenopause. However,typically a woman will have experienced them at pu-
Weight Gain Despite Appropriate Diet and
berty or when first using oral contraceptives. What
Exercise
is unique about perimenopausal migraines is thatthey seem more refractory to management with acute
Before I experienced perimenopausal weight gain
therapies, and often occur at midcycle and peri-men-
and perpetual hunger (that a patient once aptly
strually, thus twice a month. This can be debilitating
described as, "my teeth feel hungry"), I was a skeptic
if each migraine episode lasts for 3-5 days. To my
that overweight could be increased by perimeno -
knowledge there are no data on OMP for migraine
pausal metabolic change and not simply by over-
therapy however, it has multiple anti-oxidative, anti-
eating and/or under-exercising. However, there are
apoptotic effects and decreases neuroexcitotoxicity
clearly changes in metabolic rate that occur in
(Gibson et al., 2009). Therefore it appears to be an
midlife women based on the 1.5 BMI unit gain in the
appropriate therapy to try as a neuromodulating
45-54 decade in population based data from
treatment (rather than the less specific beta blockers
Canadian women; men experienced a more gradual
P4 FOR SYMPTOMATIC PERIMENOPAUSE – PRIOR 117
07-prior:Opmaak 1 20/06/11 09:51 Pagina 118
0.5 BMI gain per decade starting in their 30s
yet isn't getting restful sleep and is having night
(Hopman et al., 2007). Perimenopausal women with
sweats as well as heavy flow. "Lack of energy," al-
a past history of gestational diabetes, those with a
though non-specific, is the most prevalent experience
Type 2 diabetes mellitus family history and those
of perimenopausal women. It occurs for 38-43% of
who are most generally symptomatic seem to be at
women and is equally likely throughout all phases
increased risk for weight gain. Obviously, before
of perimenopause (Dennerstein et al., 2000). After
doing anything else, the health care provider must
assessing and treating for anemia or hypothyroidism,
review actual exercise and food records and work to
I would treat her sleep disturbance and night sweats
ensure that both of these are optimal with at least
with cyclic OMP. She also needs ibuprofen 200 mg
30 minutes of moderate exercise daily. There is some
every 4-6 hours on every heavy flow day. In my ex-
rationale for treatment with OMP given that proges-
perience, once Emily understands the hormonal
terone increases core temperature and requires
changes she is experiencing and has an idea of
300 kcal/d to do that in weight stable premenopausal
what's ahead for her, effective treatment of night
women (Barr et al., 1995). However, I have rarely
sweats and sleep disturbances will allow her to re-
treated women with OMP only to assist them in
gain her ability to cope. But, given the unpredictabil-
weight control. Instead I have found that metformin,
ity of perimenopause, she needs a skilled and
a drug which makes insulin more effective and thus
empathetic physician to work with her through this
decreases insulin resistance, is a very helpful therapy
protracted and sometimes difficult "estrogen's storm
for women who have an increasing waist circumfer-
season" of perimenopause (Prior, 2005b).
ence (normal for Caucasians is less than 88 cm) or arising hemoglobin A1C level to values of 6.0 or
References
higher (Mogul et al., 2001). Obviously, if a womanwith increasing weight also has night sweats or
National Institutes of Health State-of-the-Science Conference
statement: management of menopause-related symptoms.
breast tenderness or sleep disturbances, cyclic or
Ann Intern Med. 2005;142:1003-13.
daily OMP will be a helpful therapy.
Barr SI, Janelle KC, Prior JC. Energy intakes are higher during
the luteal phase of ovulatory menstrual cycles. Am J Clin
Cyclic Progesterone Treatment for Infertility in
Baumgartner AK, Hausler A, Seifert-Klauss V et al. Breast
Early Perimenopause
cancer after hormone replacement therapy – does the prognosis differ in perimenopausal and postmenopausal
Because perimenopause physiology involves ovula-
women? Breast J. 2011; in press.
Baxter S, Prior JC. The Estrogen Errors: Why Progesterone is
tory disturbances with decreases in progesterone
Better For Women's Health. Westport: Praeger Publishers,
levels (Santoro et al., 1996) and in luteal phase
lengths even within regular, ovulatory cycles (Hale
Burger HG. The controversial endocrinology of the menopausal
transition - Author's Response. J Clin Endocrinol Metab.
et al., 2007; Prior, 2002b), it makes sense that infer-
tility might be related to these ovulatory distur-
Burger HG, Dudley EC, Hopper JL et al. The endocrinology of
bances. The natural extension of that thought is to
the menopausal transition: a cross-sectional study of a
supplement with cyclic OMP (Figure 4). However,
population-based sample. J Clin Endocrinol Metab.
1995;80:3537-45.
OMP has the potential to interfere with the LH peak
Casper RF, Dodin S, Reid RL. The effect of 20 ug ethinyl
and ovulation if given too early in the cycle. There-
estradiol/1 mg norethindrone acetate (Minestrin™), a low-
fore I recommend that women who observe in-
dose oral contraceptive, on vaginal bleeding patterns, hotflashes, and quality of life in symptomatic perimenopausal
creased clear cervical mucus at midcycle should wait
women. Menopause. 1997;4:139-47.
to start their 14 days of OMP until after that mucus
Chang KJ, Lee TTY, Linares-Cruz G et al. Influence of percu-
is decreasing or has disappeared. My clinical expe-
taneous administration of estradiol and progesterone onhuman breast epithelial cell cycle in vivo. Fertil Steril.
rience is that at a large number of fertility desiring
women were able to achieve fertility only by using
Check JH, Giangreco J. Three successful pregnancies following
cyclic OMP. Again, there are no controlled or even
natural conception over an 8-year time span despite serum
observational studies in support of this idea. But
follicle stimulating hormone level greater than 15 mIU/ml.
Clin Exp Obstet Gynecol. 2009;36:12-4.
repeated spontaneous perimenopausal conceptions
Dennerstein L, Dudley EC, Hopper JL et al. A prospective
and full term pregnancies have been documented
population-based study of menopausal symptoms. Obstet
despite markers suggesting in vitro fertility treat-
Dennerstein L, Spencer-Gardner C, Gotts G et al. Progesterone
ments are futile (Check and Giangreco, 2009).
and the premenstrual syndrome: a double blind crossovertrial. Br Med J. 1985;290:1617-21.
How to help Emily
Douglas S. Premenstrual syndrome. Evidence-based treatment
in family practice. Can Fam Physician. 2002;48:1789-97.
Foidart J, Collin C, Denoo X et al. Estradiol and progesterone
We started this discussion with a familiar but
regulate the proliferation of human breast epithelial cells.
strangely distraught patient. Emily is extremely tired
Fertil Steril. 1998;5:963-9.
F, V & V IN OBGYN
07-prior:Opmaak 1 20/06/11 09:51 Pagina 119
Fournier A, Berrino F, Clavel-Chapelon F. Unequal risks for
Mogul HR, Peterson SJ, Weinstein BI et al. Metformin and car-
breast cancer associated with different hormone replacement
bohydrapte-modified diet: a novel obestiy treatment protocol:
therapies: results from the E3N cohort study. Breast Cancer
Preliminary findings from a case series of nondiabetic
Res Treat. 2008;107:103-11.
women with midlife weight gain and hyperinsulinemia. Heart
Friess E, Tagaya H, Trachsel L et al. Progesterone-induced
changes in sleep in male subjects. Am J Physiol. 1997;272:
Morse CA, Dudley E, Guthrie J et al. Relationships between
premenstrual complaints and perimenopausal experiences.
Gibson CL, Coomber B, Rathbone J. Is progesterone a candidate
J Psychosom Obstet Gynaecol. 1989;19:182-91.
neuroprotective factor for treatment following ischemic
Munster K, Schmidt L, Helm P. Length and variation in the men-
stroke? Neuroscientist. 2009;15:324-32.
strual cycle – a cross-sectional study from a Danish county.
Graham JD, Clarke CL. Physiological action of progesterone in
Br J Obstet Gynaecol. 1992;99:422-9.
target tissue. Endocr Rev. 1997; 18:502-19.
Nielsen HK, Brixen K, Bouillon R et al. Changes in biochemical
Hale GE, Hitchcock CL, Williams LA et al. Cyclicity of breast
markers of osteoblastic activity during the menstrual cycle.
tenderness and night-time vasomotor symptoms in mid-life
J Clin Endocrinol Metab. 1990;70:1431-7.
women: information collected using the Daily Peri-
O'Connor KA, Ferrell RJ, Brindle E et al. Total and Unopposed
menopause Diary. Climacteric. 2003;6:128-39.
Estrogen Exposure across Stages of the Transition to
Hale GE, Hughes CL, Burger HG et al. Atypical estradiol
Menopause. Cancer Epidemiol Biomarkers Prev. 2009;
secretion and ovulation patterns caused by luteal out-of-phase
(LOOP) events underlying irregular ovulatory menstrual
O'Leary Cobb J. Understanding Menopause. Toronto: Key
cycles in the menopausal transition. Menopause. 2009;16:50-
Porter Books, 2005.
Oudshoorn N. Beyond the Natural Body: an archeology of sex
Hale GE, Zhao X, Hughes CL et al. Endocrine features of
hormones. London: Routledge, 1994.
menstrual cycles in middle and late reproductive age and the
Prior JC. Progesterone as a bone-trophic hormone. Endocr Rev.
menopausal transition classified according to the Staging of
Reproductive Aging Workshop (STRAW) staging system.
Prior JC. Perimenopause: The complex endocrinology of the
J Clin Endocrinol Metab. 2007;92:3060-7.
menopausal transition. Endocr Rev. 1998;19:397-428.
Harlow SD, Cain K, Crawford S et al. Evaluation of four
Prior JC. Premenstrual symptoms and signs. In: Rabel RE,
proposed bleeding criteria for the onset of late menopausal
Bope ET, editors. Conn's Current Therapy 2002. New York:
transition. J Clin Endocrinol Metab. 2006;91:3432-8.
W.B. Saunders Company, 2002a:1078-80.
Harlow SD, Mitchell ES, Crawford S et al. The ReSTAGE
Prior JC. The ageing female reproductive axis II: ovulatory
Collaboration: defining optimal bleeding criteria for onset of
changes with perimenopause. In: Chadwick DJ, Goode JA,
early menopausal transition. Fertil Steril. 2008;89:129-40.
editors. Endocrine Facets of Ageing. Chichester, UK: John
Harvey A, Hitchcock CL and Prior JC. Ovulation disturbances
Wiley and Sons Ltd, 2002b:172-86.
and mood across the menstrual cycles of healthy women.
Prior JC. Clearing confusion about perimenopause. BC Med J.
J Psychosom Obstet Gynaecol. 2009;30:207-14.
Hopman WM, Leroux C, Berger C et al. Changes in body mass
Prior JC. Estrogen's Storm Season- Stories of Perimenopause.
index in Canadians over a five-year period: results of a
Vancouver, BC: CeMCOR, 2005b.
prospective, population-based study. BMC. Public Health.
Prior JC, Alojado N, Vigna YM et al. Estrogen and progestin are
equally effective in symptom control post-ovariectomy – a
Irvine GA, Campbell-Brown MB, Lumsden MA et al.
one-year, double-blind, randomized trial in premenopausal
Randomised comparative trial of the levonorgestrel intra -
women. Program of the 76th Annual Meeting of the
uterine system and norethisterone for treatment of idiopathic
Endocrine Society, Anaheim, Ca. Abstract 12H, 411. 1994.
menorrhagia. Br J Obstet Gynaecol. 1998;105:592-8.
Prior JC, Barr SI, Vigna YM. The controversial endocrinology
Johannes CB, Crawford SL, Posner JG et al. Longitudinal
of the menopausal transition (letter). J Clin Endocrinol
patterns and correlates of hormone replacement therapy use
in middle-aged women. Am J Epidemiol. 1994;140:439-52.
Prior JC, Hitchcock CL. Progesterone for vasomotor symptoms:
Klein NA, Illingworth PJ, Groome NP et al. Decreased inhibin
A 12-week randomized, masked placebo-controlled trial in
B secretion is associated with the monotropic FSH rise in
healthy, normal-weight women 1-10 years since final
older, ovulatory women: A study of serum and follicular fluid
menstrual flow. Endocr Rev. 2010;31:S51.
levels of dimeric inhibin A and B in spontaneous menstrual
Prior JC, Vigna YM, Watson D. Spironolactone with physio -
cycles. J Clin Endocrinol Metab. 1996;81:7: 2742-5.
logical female gonadal steroids in the presurgical therapy of
Landgren BH, Unden AL, Diczfalusy E. Hormonal profile of the
male to female transexuals: a new observation. Arch Sex Beh.
cycle in 68 normally menstruating women. Acta Endocr
1989; 18:49-57.
Richardson SJ, Senikas V, Nelson JF. Follicular depletion during
Lethaby A, Augood C, Duckitt K. Nonsteroidal anti-inflamma-
the menopausal transition: evidence for accelerated loss and
tory drugs for heavy menstrual bleeding. Cochrane Database
ultimate exhaustion. J Clin Endocrinol Metab. 1987;65:1231.
Syst Rev. 2002;CD000400.
Santoro N, Crawford SL, Lasley WL et al. Factors related to
MacLennan AH, Broadbent JL, Lester S et al. Oral oestrogen
declining luteal function in women during the menopausal
and combined oestrogen/progestogen therapy versus placebo
transition. J Clin Endocrinol Metab. 2008;93:1711-21.
for hot flushes. Cochrane Database Syst Rev. 2004;
Santoro N, Rosenberg J, Adel T et al. Characterization of repro-
ductive hormonal dynamics in the perimenopause. J Clin
Mather KJ, Norman EG, Prior JC et al. Preserved forearm en-
Endocrinol Metab. 1996;81:1495-1501.
dothelial responses with acute exposure to progesterone: a
Schussler P, Kluge M, Yassouridis A et al. Progesterone reduces
randomized cross-over trial of 17-b estradiol, progesterone,
wakefulness in sleep EEG and has no effect on cognition in
and 17-b estradiol with progesterone in healthy menopausal
healthy postmenopausal women. Psychoneuroendocr. 2008;
women. J Clin Endocrinol Metab. 2000;85: 4644-9.
Metcalf MG, MacKenzie JA. Menstrual cycle and exposure to
Seifert-Klauss V, Prior JC. Progesterone and bone: Actions
estrogens unopposed by progesterone: relevance to studies
promoting bone health in women. J Osteop. 2010; 845180.
on breast cancer incidence. J Endocrinol. 1985;104:137-41.
Shostak M Nisa: the life and words of a !Kung woman. New
Moen MH, Kahn H, Bjerve KS et al. Menometrorrhagia in the
York: Vintage Books, 1981.
perimenopause is associated with increased serum estradiol.
Simon JA, Shangold MM, Andrews MC et al. Micronized prog-
esterone therapy: the importance of route of administration
P4 FOR SYMPTOMATIC PERIMENOPAUSE – PRIOR 119
07-prior:Opmaak 1 20/06/11 09:51 Pagina 120
and pharmacokinetics on clinical outcome. J Contracept
Vollman RF. The menstrual cycle. In: Friedman EA, editor.
Fertil Sex. 1992;20:13-8.
Major Problems in Obstetrics and Gynecology, Vol 7.
Soules MR, Sherman S, Parrott E et al. Executive summary:
Toronto: W.B. Saunders Company, 1977:11-193.
stages of reproductive aging workshop (STRAW). Fertil
Weiss G, Skurnick JH, Goldsmith LT et al. Menopause and
hypothalamic-pituitary sensitivity to estrogen. JAMA.
Thys-Jacobs S, Alvir MJ. Calcium-regulating hormones across
the menstrual cycle: evidence of a secondary hyerparathy-roidism in women with PMS. J Clin Endocrinol Metab.
1995;80:2227-32.
F, V & V IN OBGYN
Source: http://www.fvvo.be/assets/188/09-Prior.pdf
mnassa.org.za
The Celestial by Magda Streicher It is only appropriate to conclude the Image source: Starry Night Pro IYA2009 by considering one of the most vital parts of the telescope – the reticle – immortalised by the constel- lation Reticulum. Reticulum is Latin for ‘net'. One can imagine astronomers fishing out the discoveries from among rhomboidal crosshairs which he used to
Microsoft powerpoint - 16. drugs and hygiene [compatibility mode]
KS4 Physical These icons indicate that teacher's notes or useful web addresses are available in the Notes Page. This icon indicates that the slide contains activities created in Flash. These activities are not editable. For more detailed instructions, see the Getting Started presentation. What we will learn in this presentation: