Postoperative pain and early quality of life after radiofrequency ablation and mechanochemical endovenous ablation of incompetent great saphenous veins
Postoperative pain and early quality of life afterradiofrequency ablation and mechanochemicalendovenous ablation of incompetent greatsaphenous veins Ramon R. J. P. van Eekeren, MD,a Doeke Boersma, MD,b Vincent Konijn, MD,aJean Paul P. M. de Vries, MD, PhD,b and Michel M. J. P. Reijnen, MP, PhD,a Arnhem and Nieuwegein,
The Netherlands
Objective: Thermal ablative techniques of varicose veins carry a risk of heat-related complications, including postoperative
pain. Mechanochemical endovenous ablation (MOCA) might avoid these complications and reduce postoperative pain
because of the absence of thermal energy. This study evaluated postoperative pain and quality of life after radiofrequency
ablation (RFA) and MOCA for great saphenous vein (GSV) incompetence.
Methods: Sixty-eight patients with unilateral GSV incompetence were treated with either RFA or MOCA in this
prospective observational study. Patients monitored their pain for the first 14 postoperative days on a 100-mm visual
analog scale (VAS). They also completed the general (RAND 36-Item Short-Form Health Survey) and disease-specific
(Aberdeen Varicose Vein Questionnaire) quality of life questionnaires before and 6 weeks after treatment.
Results: Patients treated with MOCA reported significantly less postoperative pain than patients treated with RFA during
the first 14 days after treatment (4.8 ⴞ 9.7 mm vs 18.6 ⴞ 17.0 mm; P < .001) (mean VAS over 14 days). The lower
postoperative pain score was associated with a significantly earlier return to normal activities (1.2 ⴞ 1.8 vs 2.4 ⴞ 2.8 days;
P ⴝ .02) and work resumption (3.3 ⴞ 4.7 vs 5.6 ⴞ 5.8 days, respectively; P ⴝ .02). At 6 weeks, patients in both groups
perceived an improved change in health status and an improved disease-specific quality of life.
Conclusions: MOCA is associated with significantly less postoperative pain, faster recovery, and earlier work resumption
compared with RFA in the treatment of GSV incompetence. MOCA and RFA are both related to a rapid improvement
in quality of life. ( J Vasc Surg 2012;䡲䡲:䡲䡲䡲.)
Varicose veins are a common medical problem with liquid sclerosant. The use of tumescent anesthesia is not overall prevalence of 20% to Chronic venous insuffi- necessary because no heat is used. The first studies of this ciency may have a major effect on patients' health-related technique have shown that MOCA is a safe and feasible quality of life in advanced stages of disease, leading to method for treating great saphenous vein (GSV) incompe- significant costs in total health care With tence with promising short-term results.Because heat is occlusion rates over 90%, as reported for endovenous laser not used as the mechanism of action, the risk of heat-related ablation (EVLA) and radiofrequency ablation (RFA) in complications, including postoperative pain is considered prospective more emphasis is placed on secondary to be lower. The present study assessed the postoperative outcome measures, such as postoperative pain, complica- pain and quality of life in patients treated with RFA or tions, quality of life, and return to normal activities. Ran- domized studies have reported significantly lower postop-erative pain after RFA compared with Thesestudies, however, may have been biased by the choice of wavelengths and a difference in the fibers used.
Patients. The study included 68 consecutive patients,
Mechanochemical endovenous ablation (MOCA) is a treated between January and December 2011 with RFA or recently introduced treatment that combines mechanical MOCA. All were diagnosed with unilateral symptomatic damage of the venous intimal layer with the dispersion of a GSV incompetence, and were treated in the Rijnstate Hos- From the Department of Surgery, Rijnstate Hospital, Arnhema; and the pital, Arnhem, The Netherlands. Patients treated with Department of Vascular Surgery, St Antonius Hospital, Nieuwegein.b MOCA were also included in a prospective registry study Author conflict of interest: none.
(NCT01459263 at clinical.trials.gov). The regional medi- Reprint requests: Michel M.J.P. Reijnen, MP, PhD, Department of Surgery, cal ethics committee approved the study. Patients were Rijnstate Hospital, Wagnerlaan 55, 6815 AD, Arnhem, The Netherlands included after signing the informed consent form in this The editors and reviewers of this article have no relevant financial relationships prospective observational trial. Patients, who did not want to disclose per the JVS policy that requires reviewers to decline review of any to be treated with MOCA, were routinely offered treat- manuscript for which they may have a conflict of interest.
ment with RFA. All patients had primary GSV incompe- tence, as demonstrated by duplex imaging, performed by Copyright 2012 by the Society for Vascular Surgery.
two certified vascular practitioners. Reflux was defined as a JOURNAL OF VASCULAR SURGERY 2 van Eekeren et al
retrograde flow of ⱖ0.5 seconds after calf compression eral and disease-specific quality of life, respectively. The measured with the patient upright.
Dutch version of RAND-36 covers health status in eight Eligibility criteria were age over 18 years, C to C dimensions: physical functioning, social functioning, role varicose veins and primary GSV incompetence. Exclusion limitations due to physical health problems and emotional criteria included pregnancy and lactation, the use of anti- problems, general mental health, vitality, bodily pain, and coagulants, previous surgical treatment of varicose veins or general health perceptions. Also included is one item that history of deep venous thrombosis. Allergy to polidocanol provides an indication of perceived changes in health. A was a contra-indication for MOCA.
high score indicates good health status.
Treatment. Both treatments were performed under
At the end of the procedure patients marked their pain local anesthesia by a specialized team consisting of a vascu- perception on a 100-mm visual analog scale (VAS). Proce- lar surgeon and vascular practitioner. Patients were treated dural pain was defined as the amount of pain patients as outpatients in daily care. No sedation or antibiotics were experienced during the procedure. Afterward patients were instructed to complete a 14-day diary card to record the MOCA was performed using the ClariVein catheter level of pain on a 100-mm VAS. On the diary card, patients (Vascular Insights, Madison, Wisc), as previously de- were also asked to provide information about returning to Briefly, a Seldinger technique was used to intro- normal activities and the amount of analgesics used was duce a 4F introducer sheath into the GSV, and the recorded. The dosage of medication was not listed. At the ClariVein catheter was positioned with the tip of the dis- 6-week follow-up, RAND-36 and AVVQ were completed persion wire 0.5 cm distal of the saphenofemoral junction again, and a vascular surgeon assessed the VCSS.
(SFJ) under ultrasound guidance. After the tip was properly Statistical analysis. The primary end point of this
positioned, the wire was activated for a few seconds to study was postoperative pain. A sample size calculation was induce spasm of the proximal vein. Then, the activated performed based on the assumption that MOCA would catheter with rotating tip was steadily withdrawn at 1 cm reduce postoperative pain during the first 3 days by 50% every 7 seconds, simultaneously dispersing liquid polido- compared with RFA. To describe a significant difference, canol (Aethoxysklerol; Kreussler Pharma, Wiesbaden, Ger- 34 patients were necessary in each group.
many) to the damaged vein wall. The proximal 10 to 15 cm Intergroup analysis was done using the Student t-test was treated with 2 mL polidocanol 2% and the remaining or Mann-Whitney U test for continuous data and the 2 or vein with polidocanol 1.5%. The total amount of liquid Fisher exact test for categoric data. Variables are presented sclerosant used was determined by the diameter of the as means ⫾ standard deviation (SD) if distributed paramet- varicose vein near the SFJ and length of GSV.
rically, or as median with interquartile range (IQR, 25th to In patients treated with RFA, a 6F introducer sheath 75th percentiles) if distributed nonparametrically. Two- was inserted in the GSV under ultrasound guidance using a sided significance was set at P ⬍ .05. The primary end point Seldinger technique. Then, the VNUS ClosureFAST- was analyzed using the Mann-Whitney U test. Analysis of catheter (VNUS Medical Technologies, Sunnyvale, Calif) pain was performed using repeated measurements design.
was introduced with the tip of the catheter located 2 cm Differences in scores of the AVVQ, RAND-36, and VCSS below the SFJ. Subsequently, tumescent anesthesia was before and at 6 weeks after treatment were tested using the applied using normal saline containing 1% lidocaine with Wilcoxon signed-rank test, for single group analysis. The epinephrine. After proper positioning of the catheter tip Mann-Whitney U test was used to test differences in change was confirmed, the GSV was ablated in 7 cm segments between both groups.
during a 20-second treatment cycle. The temperature was Statistical analyses were performed using SPSS 15.0 maintained at 120° during withdrawal of the catheter by software (SPSS Inc, Chicago, Ill). A statistician supervised using a feedback system at the heating source.
all analyses.
After the procedures, patients were discharged with instructions to wear a compression stocking (30-40 mmHg) for 2 weeks. Patients were instructed to use analgesics only when they experienced postoperative pain. No stan- During the study period, 68 patients (25 men, 43 dard analgesics were prescribed. No concomitant phlebec- women) were treated, 34 in each group, and all completed tomies or sclerotherapy were performed. Treatment time their 6-week follow-up assessment. Patients were a mean was defined as duration of the treatment starting with age of 58 ⫾ 17 years. Patient characteristics are summa- puncturing the vein and ending with removal of the cath- rized in There were no significant differences between the groups regarding demographic data, CEAP Assessment. Patients were examined during the out-
classification, preoperative VCSS, and initial AVVQ. The patient visit by a vascular surgeon, who recorded their treated GSV was significantly wider at the SFJ in the RFA CEAP and Venous Clinical Severity Score group than in the MOCA group (P ⫽ .03). Treatment time Before the procedure, patients were asked to was significantly shorter in the MOCA group (P ⫽ .02). No complete the Dutch versions of the RAND-36-Item Short- major complications occurred in either group, and there Form Health Survey and the Aberdeen Var- was no difference in the incidence of minor complications icose Vein Questionnaire to observe the gen- between the two groups
JOURNAL OF VASCULAR SURGERYVolume 䡲䡲, Number 䡲
van Eekeren et al 3
Table I. Patient characteristics and technical data
(n ⫽ 34)
(n ⫽ 34)
Length of vein ablated, cm
Time of procedure, minutes
Procedural pain (0-100 mm VAS)
Number RFA cycles
Amount of polidocanol, mg
Total volume of polidocanol, mL
AVVQ, Aberdeen Varicose Vein Questionnaire; BMI, body mass index; CEAP, Clinical Etiologic Anatomical Pathophysiological classification; GSV, greatsaphenous vein; MOCA, mechanochemical endovenous ablation; RFA, radiofrequency ablation; VAS, visual analog scale; VCSS, Venous Clinical SeverityScore.
aStudent t-test.
b2 test.
cMann-Whitney U test.
Table II. Complications in the first 6 weeks after MOCA
and RFA
(n ⫽ 34)
(n ⫽ 34)
Major complications
Deep venous thrombosis
Pulmonary embolism
Minor complications
MOCA, Mechanochemical endovenous ablation; RFA, radiofrequency ab-
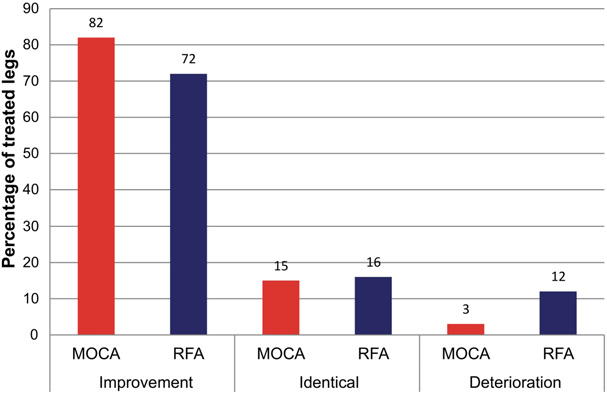
Fig 1. Assessment of the Venous Clinical Severity Score (VCSS) 6
weeks after treatment with mechanochemical endovenous ablation
aFisher exact test.
(MOCA) and radiofrequency ablation (RFA).
After 6 weeks, the median VCSS significantly decreased
in both groups, from 3.0 (IQR, 2.75-5.25) to 1.0 (IQR,
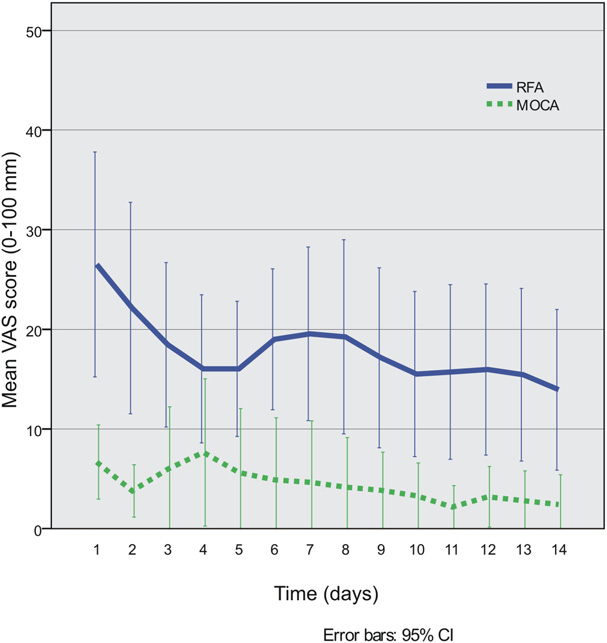
Postoperative pain. The mean procedural pain dur-
1.0-2.0) in the MOCA group (P ⬍ .001) and from 4.0
ing treatment was 22 ⫾ 16 mm for MOCA and 27 ⫾ 15
(IQR, 3.0-7.0) to 3.0 (IQR, 1.25-3.75) in the RFA group
mm for RFA (P ⫽ .16) on the 0 to 100-mm VAS. The
(P ⬍ .001). VCSS improvement was similar between
progress of postoperative pain is shown in At each
groups (P ⫽ .21). Although the VCSS improved in most
postoperative day, the difference between groups was sta-
patients, VCSS deteriorated in five patients at 6 weeks after
tistically significant. Patients receiving MOCA reported less
treatment; one in the MOCA group and four in the RFA
pain over the first 3 days, with mean pain of 6.2 ⫾ 9.2 mm
group There were three patients with reported
for MOCA and 20.5 ⫾ 25.5 mm for RFA (P ⫽ .004). The
postoperative pain after 2 weeks, one patient with a throm-
mean postoperative pain per day during the first 14 days
bophlebitis, and one patient with induration. The median
after treatment was 4.8 ⫾ 9.7 mm in the MOCA group and
deterioration in VCSS was 1.0 (IQR, 1.0-2.0).
18.6 ⫾ 17.0 mm in the RFA group (P ⬍ .001). Thrombo-
JOURNAL OF VASCULAR SURGERY
4 van Eekeren et al
the MOCA group than in the RFA group (P ⫽ .02),respectively, 1.0 days (IQR, 1.0-3.75) vs 2.0 days (IQR,2.0-7.0).
This study has demonstrated that postoperative pain is
significantly lower after MOCA compared with RFA, cor-responding to a 74% reduction in pain for the first 14postoperative days. MOCA was also associated with a sig-nificantly faster return to normal activities and work re-sumption.
Whereas occlusion rates over 90% are constantly re-
ported after endovenous treatment, secondary outcomemeasures of treatment, such as postoperative pain, return tonormal activities and health-related quality of life becomemore important to determine the optimal endovenoustreatment for patients with varicose Several stud-ies have analyzed postoperative pain after thermal endovenousablation, foam sclerotherapy, and surgical stripping. Rasmus-sen et al reported significantly less postoperative pain in pa-tients treated with RFA (1.21) and foam sclerotherapy(1.60) than those treated with EVLA (2.58) and surgical
Fig 2. Mean postoperative pain scores on a 0 to 100 mm visual
stripping The observed pain was presented as
analogue scale for 14 days after mechanochemical endovenous
mean pain during the first 10 days on a 0 to 10 cm VAS.
ablation (MOCA) and radiofrequency ablation (RFA). CI, Confi-
Other randomized studies also confirmed the superiority of
dence interval; VAS, visual analog scale.
RFA over EVLA in postoperative The postoper-ative pain in patients treated with RFA in this study isconsistent with those reports. However, results of postop-
phlebitis and induration were associated with more postop-
erative pain are difficult to compare, while outcomes of
erative pain in both groups.
postoperative pain have been valued in various ways. Most
Information about the number of days, in which pa-
reports on postoperative pain after varicose vein treatment
tients used analgesics (mostly paracetamol or ibuprofen),
use a VAS to evaluate postoperative pain, but a validation
was available in 60 patients (88%). Patients in the MOCA
study of different pain rating scales has never been per-
group used postoperative analgesics for a mean of 0.5 ⫾ 1.5
formed for this specific subject. Evidence supports the
days compared with 2.8 ⫾ 4.2 days in had significantly less
reliability and validity of most pain intensity The
days, in which postoperative analgesics were used than in
authors advocate a uniform use of outcome measures for
the RFA group, which was a significant difference (P ⫽
postoperative pain.
The postoperative pain in patients treated with MOCA
Quality of life. Six weeks after treatment, the AVVQ
was consistent with our previous report. In a safety study,
improved significantly in both groups, from 7.1 (IQR,
we found that the mean postoperative pain on the first day
5.3-9.2) to 5.0 (IQR, 3.0-8.5) in the MOCA group (P ⫽
was 9 mm on a 0 to 100 mm The score decreased to
.006) and from 9.5 (IQR, 4.5-16.4) to 4.5 (IQR, 1.5-
a mean of 2 mm, 7 days after MOCA. The main objective of
11.2) in the RFA group (P ⫽ .002). The difference in
this study was to evaluate postoperative pain and early
AVVQ change between the groups was not statistically
quality of life, not to observe anatomical success. However,
significant (P ⫽ .17).
larger comparative studies are needed to assess the long-
Comparison of RAND-36 scores before and at 6 weeks
term efficacy of MOCA. Elias et al reported a 96.7% occlu-
after treatment with MOCA and RFA showed that health
sion rate at 260 days in patients treated with The
status significantly improved in two dimensions for MOCA
observed differences in postoperative pain in the present
(physical functioning and role limitations physical). For
study may be explained by the different mechanisms of
RFA there was an improvement in bodily pain after 6
action. Heating the vein and its surrounding tissue with
weeks. No deterioration in quality of life was observed.
RFA causes endothelial denudation, collagen denaturation,
Patients in both groups perceived an improved change in
and vein closure at temperatures of Perforation of
veins and heating of surrounding perivenous tissue is
Return to normal activities. The time to return to
thought to be associated with (prolonged) postoperative
normal activities was 1.0 day (IQR, 0-1.0) in the MOCA
group and 1.0 day (IQR, 1.0-3.0) in the RFA group, which
MOCA combines mechanical damage to the endothe-
was significantly longer (P ⫽ .01). The median time to
lium of the vein wall with the infusion of a sclerosant. The
work resumption for employees was significantly shorter in
liquid sclerosant produces irreversible damage to the ve-
JOURNAL OF VASCULAR SURGERYVolume 䡲䡲, Number 䡲
van Eekeren et al 5
Table III. Median (IQR) health status scores for patients before and 6 weeks after treatment with MOCA and RFA
(RAND-36)
P value intergroupb
Physical functioning
Social functioning
Health perception
IQR, Interquartile range; MOCA, mechanochemical endovenous ablation; RAND-36, RAND-36-Item Short-Form Health Survey; RFA, radiofrequencyablation.
aWilcoxon Signed-Ranks test.
bMann-Whitney U test.
nous endothelium. The cellular membranes of the endo-
Adding tumescence anesthesia to a standard treatment,
thelium are damaged, creating denudation of the endothe-
however, does not seem to contribute to a clinically rele-
lium and endofibrosis. Finally, this causes venous obliteration
vant increase in procedural pain. In addition, tumescence
and thrombus Damage of the endothelium
anesthesia is time-consuming, as reflected by the signifi-
depends on the concentration of sclerosant. The purpose of
cantly longer treatment time with RFA. In the present
the mechanical damage is fourfold: (1) promoting the
study, tumescence anesthesia was widely applied before the
coagulation activation by minimal mechanical damage to
RFA treatment was initiated. Because insufficient tumes-
the endothelium, (2) inducing a vasospasm that reduces the
cent anesthesia may contribute to increased pain, the ade-
diameter of the vein, (3) increasing the action of sclerosant
quacy was assessed by duplex ultrasound imaging and by
by an increase in surface, and (4) ensuring an even distri-
controlling the temperature of the catheter on the monitor.
bution of the sclerosant at the endothelium. A recent study
Patients treated with MOCA needed significantly less
showed that adding mechanical balloon catheter injury to
time to return to normal activities, and the time to resume
standard foam sclerotherapy increased endothelial cell
work was also significantly shorter. The observation that
No (in vivo) histologic studies on MOCA are to
patients treated with MOCA resume their work 1 day
date, but the authors hypothesize that the rotating wire also
earlier than patients treated with RFA might have a signif-
increases endothelial cell loss. Moreover, endothelial cell
icant effect on the total health care burden of varicose vein
loss and damage to the media are significantly greater with
treatment. This observation urges the initiation of further
sodium tetradecyl sulfate compared with In
randomized studies to confirm the observation.
this study polidocanol was used as single sclerosant regis-
As assessed by the RAND-36 results, the health status
tered in The Netherlands.
of patients was improved 6 weeks after MOCA in the
Although the VAS was threefold lower in the MOCA
dimensions of physical functioning and role limitations
group, the procedural pain was not significantly different
physical. This suggests that these patients perceived fewer
between the groups. This may have been caused by the
problems with their daily physical activities, also related
small sample size, because the study was powered a reduc-
toward employment. Both groups, however, had a signifi-
tion of 50% in the postoperative course. Previous studies
cant improvement in perceived health change. In addition,
have not assessed procedural pain as an outcome measure.
the disease-specific quality of life improved in both groups,
JOURNAL OF VASCULAR SURGERY
6 van Eekeren et al
without differences between groups. These results regard-
6. Darwood RJ, Theivacumar N, Dellagrammaticas D, Mavor AI, Gough
ing quality of life are in line with existing reports. However,
MJ. Randomized clinical trial comparing endovenous laser ablation
differences in quality of life are usually observed 1 year after
with surgery for the treatment of primary great saphenous varicoseveins. Br J Surg 2008;95:294-301.
7. Goode SD, Chowdhury A, Crockett M, Beech A, Simpson R, Richards
The present trial had some limitations. First, the study
T, et al. Laser and radiofrequency ablation study (LARA study): a
has a small population, although the expected 50% reduc-
randomized study comparing radiofrequency ablation and endovenous
tion in postoperative pain was achieved. Second, the study
laser ablation (810 nm). Eur J Vasc Endovasc Surg 2010;40:246-53.
did not document other variables that can be associated
8. Shepherd AC, Gohel MS, Lim CS, Hamish M, Davies AH. Pain
following 980-nm endovenous laser ablation and segmental radiofre-
with postoperative pain, such as depth of the vein from skin
quency ablation for varicose veins: a prospective observational study.
level, amount of tumescence fluid, quality of tumescence
Vasc Endovascular Surg 2010;44:212-6.
anesthesia, and incidence of perforation of the treated vein.
9. Van Eekeren RR, Boersma D, Elias S, Holewijn S, Werson DA, De Vries
The quality of tumescence anesthesia, in particular, is a
JP, et al. Endovenous mechanochemical ablation of great saphenous
complex parameter to observe, whereas we presume this
vein incompetence using the ClariVeinTM device: a safety study. JEndovasc Ther 2011;18:328-34.
parameter is the most important factor of pain after endo-
10. Elias S, Raines JK. Mechanochemical tumescent-less endovenous abla-
thermal ablation. Finally, as with all nonrandomized stud-
tion: final results of the initial clinical trial. Phlebology 2012;27:67-72.
ies, results are more susceptible to selection and measure-
11. Kistner RL, Eklof B, Masuda EM. Diagnosis of chronic venous disease
ment biases.
of the lower extremities: the "CEAP" classification. Mayo Clin Proc
In conclusion, MOCA is associated with significantly
12. Rutherford RB, Padberg FT, Comerota AJ, Kistner RL, Meissner MH,
less postoperative pain and a faster recovery and work
Moneta GL. Venous severity scoring: an adjunct to venous outcome
resumption, compared with RFA in the treatment of great
assessment. J Vasc Surg 2000;31:1307-12.
saphenous incompetence. These observations should be
13. Bowling A. Measuring health. A review of quality of life measurement
confirmed in a randomized controlled trial. Outcomes of
scales. Buckingham: Open University Press; 1991.
postoperative pain after endovenous ablative techniques for
14. Klem TM, Sybrandy JE, Wittens CH, Essink Bot ML. Reliability and
validity of the Dutch translated Aberdeen varicose vein questionnaire.
varicose veins may be helpful for clinicians in the decision
Eur J Vasc Endovasc Surg 2009;37:232-8.
making for optimal treatment.
15. Van den Bos R, Arends L, Kockaert M, Neumann M, Nijsten T.
Endovenous therapies of lower extremity varicosities: a meta-analysis. J
Vasc Surg 2009;49:230-9.
Conception and design: RE, DB, VK, JV, MR
16. Rasmussen LH, Lawaetz M, Bjoern L, Vennits B, Blemings A, Eklof B.
Randomized clinical trial comparing endovenous laser ablation, radio-
Analysis and interpretation: RE, MR
frequency ablation, foam sclerotherapy and surgical stripping for great
Data collection: RE, VK
saphenous varicose veins. Br J Surg 2011;98:1079-87.
Writing the article: RE
17. Nordon IM, Hinchliffe RJ, Brar R, Moxey P, Black SA, Thompson
Critical revision of the article: DB, VK, JV, MR
MM, et al. A prospective double-blind randomized controlled trial of
Final approval of the article: RE, DB, VK, JV, MR
radiofrequency versus laser treatment of great saphenous vein in pa-tients with varicose veins. Ann Surg 2011;254:876-87.
Statistical analysis: RE
18. Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain
Obtained funding: Not applicable
intensity rating scales. Pain 2011;152:2399-404.
Overall responsibility: MR
19. Weiss RA. Comparison of endovenous radiofrequency ablation versus
810 nm diode laser occlusion of large veins in an animal model.
Dermatol Surg 2002;28:56-61.
20. Kern P. Sclerotherapy of varicose leg vein legs. Technique, indications
1. Callam MJ. Epidemiology of varicose veins. Br J Surg 1994;81:167-73.
and complications. Int Angiol 2002;21:40-5.
2. Andreozzi GM, Cordova RM, Scomparin A, Martini R, D'Eri A,
21. Ikponmwosa A, Abbott C, Graham A, Homer-Vanniasinkam S, Gough
Andreozzi F, et al. Quality of life in chronic venous insufficiency. An
MJ. The impact of different concentrations of sodium tetradecyl sul-
Italian pilot study of the Triveneto region. Int Angiol 2005;24:272-7.
phate and initial balloon denudation on endothelial cell loss and tunica
3. Kurz X, Lamping DL, Kahn SR, Baccaglini U, Zuccarelli F, Spreafico G,
media injury in a model of foam sclerotherapy. Eur J Vasc Endovasc
et al. Do varicose veins affect quality of life? Results of an international
population-based study. J Vasc Surg 2001;34:641-8.
22. McAree B, Ikponmwosa A, Brockbank K, Abbott C, Homer-
4. Ravi R, Trayler EA, Barrett DA, Diethrich EB. Endovenous thermal
Vanniasinkam S, Gough MJ. Comparative stability of sodium tetradecyl
ablation of superficial venous insufficiency of the lower extremity: single
sulphate (STD) and polidocanol foam: impact on vein damage in an in
center experience with 3000 limbs treated in a 7-year period. J Endovasc
vitro model. Eur J Vasc Endovasc Surg 2012;43:721-5.
Ther 2009;16:500-5.
5. Min RJ, Khilnani N, Zimmet SE. Endovenous laser treatment of
saphenous vein reflux: long-term results. J Vasc Interv Radiol 2003;14:991-6.
Submitted Jun 14, 2012; accepted Jul 29, 2012.
Source: http://files.beneficium.cz/200001199-2c5e52d581/ClariVein-Article-van-Eckeren-et-al-JVS-November-2012.pdf
naturalmolecular.ca
Natural Molecular Today Issue 1 // September 2012 EMBRACING PHARMACOGENOMICS LEADERSHIP INSIDE THIS ROLE, NMTC LAUNCHES PRIDE® REGISTRY WRITTEN BY: KEN WALLACE, NMTC Director of Business Development .revolutionizing Dr. Huey McDaniel ON A DAILY BASIS we see that personalized medicine is having a dramatic positive
02_cowings_oryginall.indd
Pol J Aviat Med Psychol 2013; 19(3): 9-16 PSYCHOPHYSIOLOGY OF SPACEFLIGHT AND AVIATION Patricia S. COWINGSNASA Ames Research Center, Moff e Field, CA, United States Source of support: Own sources Author's address: P. Cowings, NASA Ames Research Center, Moff e Field, CA, e-mail: [email protected] Background: In space, the absence of gravity alone causes unique physiological stress. Signifi cant