Microsoft word - adrenal insufficiency and addison
Adrenal Insufficiency and Addison's DiseaseWhat is adrenal insufficiency?
Adrenal insufficiency is an endocrine—or hormonal—disorder that occurs when the adrenal glands do not produce enough of certain hormones. The adrenal glands are located just above the kidneys. Adrenal insufficiency can be primary or secondary. Primary adrenal insufficiency, also called Addison's disease, occurs when the adrenal glands are damaged and cannot produce enough of the hormone cortisol and often the hormone aldosterone. Addison's disease affects one to four of every 100,000 people, in all age groups and both sexes.1 Secondary adrenal insufficiency occurs when the pituitary gland—a bean-sized organ in the brain—fails to produce enough adrenocorticotropin (ACTH), a hormone that stimulates the adrenal glands to produce cortisol. If ACTH output is too low, cortisol production drops. Eventually, the adrenal glands can shrink due to lack of ACTH stimulation. Secondary adrenal insufficiency is much more common than Addison's disease. 1 Munver R, Volfson IA. Adrenal insufficiency: diagnosis and management. Current Urology Reports. 2006;7:80–85. What do adrenal hormones do?
Cortisol
Cortisol belongs to a class of hormones called glucocorticoids, which affect almost every organ and tissue in the body. Cortisol's most important job is to help the body respond to stress. Among its many vital tasks, cortisol helps • maintain blood pressure and cardiovascular function • slow the immune system's inflammatory response • maintain levels of glucose—a form of sugar used for energy—in the blood • regulate the metabolism of proteins, carbohydrates, and fats The amount of cortisol produced by the adrenals is precisely balanced. Like many other hormones, cortisol is regulated by the brain's hypothalamus and the pituitary gland. First, the hypothalamus releases a "trigger" hormone called corticotropin-releasing hormone (CRH) that signals the pituitary gland. The pituitary responds by sending out ACTH, which in turn stimulates the adrenal glands. The adrenal glands respond by producing cortisol. Completing the cycle, cortisol then signals back to both the pituitary and hypothalamus to decrease these trigger hormones.
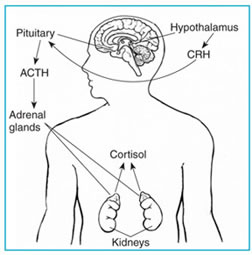
The hypothalamus sends CRH to the pituitary, which responds by sending out ACTH. ACTH then causes the adrenals to release cortisol into the bloodstream.
Aldosterone
Aldosterone belongs to a class of hormones called mineralocorticoids, also produced by the adrenal glands. Aldosterone helps maintain blood pressure and water and salt balance in the body by helping the kidneys retain sodium and excrete potassium. When aldosterone production falls too low, the kidneys are not able to regulate water and salt balance, leading to a drop in both blood volume and blood pressure.
What are the symptoms of adrenal insufficiency?
The symptoms of adrenal insufficiency usually begin gradually. The most common symptoms are
• chronic, worsening fatigue • muscle weakness • loss of appetite • weight loss
Other symptoms can include
• nausea • vomiting • diarrhea • low blood pressure that falls further when standing, causing dizziness or fainting • irritability and depression • a craving for salty foods due to salt loss • hypoglycemia, or low blood glucose • headache • sweating • in women, irregular or absent menstrual periods
Hyperpigmentation, or darkening of the skin, can occur in Addison's disease but not in secondary adrenal insufficiency. This darkening is most visible on scars; skin folds; pressure points such as the elbows, knees, knuckles, and toes; lips; and mucous membranes such as the lining of the cheek.
Because the symptoms progress slowly, they are often ignored until a stressful event like an illness or accident causes them to worsen. Sudden, severe worsening of symptoms is called an Addisonian crisis, or acute adrenal insufficiency. In most cases, symptoms of adrenal insufficiency become serious enough that people seek medical treatment before a crisis occurs. However, sometimes symptoms first appear during an Addisonian crisis.
Symptoms of an Addisonian or "adrenal" crisis include
• sudden, penetrating pain in the lower back, abdomen, or legs • severe vomiting and diarrhea • dehydration • low blood pressure • loss of consciousness
If not treated, an Addisonian crisis can be fatal.
What causes Addison's disease?
Autoimmune Disorders
The gradual destruction of the adrenal cortex, the outer layer of the adrenal glands, by the body's immune system causes up to 80 percent of Addison's disease cases.2 In autoimmune disorders, the immune system makes antibodies that attack the body's own tissues or organs and slowly destroy them.
Adrenal insufficiency occurs when at least 90 percent of the adrenal cortex has been destroyed. As a result, often both cortisol and aldosterone are lacking. Sometimes only the adrenal glands are affected. Sometimes other endocrine glands are affected as well, as in polyendocrine deficiency syndrome.
Polyendocrine deficiency syndrome is classified into two separate forms, type 1 and type 2. Type 1 is inherited and occurs in children. In addition to adrenal insufficiency, these children may have
• underactive parathyroid glands, which produce a hormone that regulates calcium
and phosphorus balance in the body
• slow sexual development • pernicious anemia, a severe type of anemia • chronic candida infections, a type of fungal infection • chronic active hepatitis, a liver disease
Type 2, sometimes called Schmidt's syndrome, usually affects young adults and may include
• an underactive thyroid gland, which produces hormones that regulate
• slow sexual development • diabetes • vitiligo, a loss of pigment on areas of the skin
Scientists think type 2 polyendocrine deficiency syndrome is also inherited because often more than one family member has one or more endocrine deficiencies.
2Martorell PM, Roep BO, Smit JWA. Autoimmunity in Addison's disease. The Netherlands Journal of Medicine. 2002;60(7):269–275.
Tuberculosis (TB), an infection that can destroy the adrenal glands, accounts for less than 20 percent of cases of Addison's disease in developed countries.3 When adrenal insufficiency was first identified by Dr. Thomas Addison in 1849, TB was the most common cause of the disease. As TB treatment improved, the incidence of adrenal insufficiency due to TB of the adrenal glands greatly decreased.
3Munver R, Volfson IA. Adrenal insufficiency: diagnosis and management. Current Urology Reports. 2006;7:80–85.
Other Causes
Less common causes of Addison's disease are
• chronic infection, mainly fungal infections • cancer cells spreading from other parts of the body to the adrenal glands • amyloidosis, a disease that causes abnormal protein buildup in, and damage to,
• surgical removal of the adrenal glands • AIDS-associated infections • bleeding into the adrenal glands • genetic defects including abnormal adrenal gland development, an inability of the
adrenal gland to respond to ACTH, or a defect in adrenal hormone production
What causes secondary adrenal insufficiency?
Secondary adrenal insufficiency can be traced to a lack of ACTH. Without ACTH to stimulate the adrenal glands, the adrenals' production of cortisol drops. Aldosterone production is not usually affected.
A temporary form of secondary adrenal insufficiency may occur when a person who has been taking a synthetic glucocorticoid hormone such as prednisone for a long time stops taking the medication, either abruptly or gradually. Glucocorticoid hormones,
which are often used to treat inflammatory illnesses such as rheumatoid arthritis, asthma, and ulcerative colitis, block the release of both CRH and ACTH. As a result, the adrenals may begin to atrophy—or shrink—from lack of ACTH stimulation and then fail to secrete sufficient levels of cortisol.
A person who stops taking a synthetic glucocorticoid hormone may have enough ACTH to function when healthy. However, when a person is under the stress of an illness, accident, or surgery, the person's body may not have enough ACTH to stimulate the adrenal glands to produce cortisol.
Another cause of secondary adrenal insufficiency is surgical removal of the noncancerous, ACTH-producing tumors of the pituitary gland that cause Cushing's disease. Cushing's disease is another disorder that leads to excess cortisol in the body. In this case, the source of ACTH is suddenly removed and replacement hormone must be taken until normal ACTH and cortisol production resumes.
Less commonly, adrenal insufficiency occurs when the pituitary gland either decreases in size or stops producing ACTH. These events can result from
• tumors or infections of the area • loss of blood flow to the pituitary • radiation for the treatment of pituitary tumors • surgical removal of parts of the hypothalamus • surgical removal of the pituitary gland
How is adrenal insufficiency diagnosed?
In its early stages, adrenal insufficiency can be difficult to diagnose. A review of a patient's medical history and symptoms may lead a doctor to suspect Addison's disease.
A diagnosis of adrenal insufficiency is confirmed through laboratory tests. The aim of these tests is first to determine whether levels of cortisol are insufficient and then to establish the cause. Radiologic exams of the adrenal and pituitary glands also are useful in helping to establish the cause.
ACTH Stimulation Test
The ACTH stimulation test is the most commonly used test for diagnosing adrenal insufficiency. In this test, blood cortisol, urine cortisol, or both are measured before and after a synthetic form of ACTH is given by injection. The normal response after an ACTH injection is a rise in blood and urine cortisol levels. People with Addison's disease or long-standing secondary adrenal insufficiency have little or no increase in cortisol levels.
Both low- and high-dose ACTH stimulation tests may be used depending on the suspected cause of adrenal insufficiency. For example, if secondary adrenal insufficiency is mild or of recent onset, the adrenal glands may still respond to ACTH because they have not yet atrophied. Some studies suggest a low dose—1 microgram—may be more effective in detecting secondary adrenal insufficiency because the low dose is still enough to raise cortisol levels in healthy people but not in people with mild or recent secondary adrenal insufficiency.
CRH Stimulation Test
When the response to the ACTH test is abnormal, a CRH stimulation test can help determine the cause of adrenal insufficiency. In this test, synthetic CRH is injected intravenously and blood cortisol is measured before and 30, 60, 90, and 120 minutes after the injection. People with Addison's disease respond by producing high levels of ACTH but no cortisol. People with secondary adrenal insufficiency have absent or delayed ACTH responses. CRH will not stimulate ACTH secretion if the pituitary is damaged, so an absent ACTH response points to the pituitary as the cause. A delayed ACTH response points to the hypothalamus as the cause.
Diagnosis during an Emergency
In patients suspected of having an Addisonian crisis, health professionals must begin treatment with injections of salt, glucose-containing fluids, and glucocorticoid hormones immediately. Although a reliable diagnosis is not possible during crisis treatment, measurement of blood ACTH and cortisol during the crisis—before glucocorticoids are given—is enough to make a preliminary diagnosis. Low blood sodium, low blood glucose, and high blood potassium are also usually present at the time of an adrenal crisis. Once the crisis is controlled, an ACTH stimulation test can be performed to obtain the specific diagnosis. More complex laboratory tests are sometimes used if the diagnosis remains unclear.
Other Tests
Once a diagnosis of Addison's disease is made, radiologic studies such as an x ray or an ultrasound of the abdomen may be taken to see if the adrenals have any signs of calcium deposits. Calcium deposits may indicate bleeding in the adrenal gland or TB, for which a tuberculin skin test also may be used. Blood tests can detect antibodies associated with autoimmune Addison's disease.
If secondary adrenal insufficiency is diagnosed, doctors may use different imaging tools to reveal the size and shape of the pituitary gland. The most common is the computerized tomography (CT) scan, which produces a series of x-ray pictures giving cross-sectional images. A magnetic resonance imaging (MRI) scan may also be used to produce a three-dimensional image of this region. The function of the pituitary and its ability to produce other hormones also are assessed with blood tests.
How is adrenal insufficiency treated?
Treatment of adrenal insufficiency involves replacing, or substituting, the hormones that the adrenal glands are not making. Cortisol is replaced with a synthetic glucocorticoid such as hydrocortisone, prednisone, or dexamethasone, taken orally once to three times each day, depending on which medication is chosen. If aldosterone is also deficient, it is replaced with oral doses of a mineralocorticoid, called fludrocortisone acetate (Florinef), taken once or twice a day. Doctors usually advise patients receiving aldosterone replacement therapy to increase their salt intake. Because people with secondary adrenal insufficiency normally maintain aldosterone production, they do not require aldosterone replacement therapy. The doses of each medication are adjusted to meet the needs of the individual.
During an Addisonian crisis, low blood pressure, low blood glucose, and high levels of potassium can be life threatening. Standard therapy involves intravenous injections of glucocorticoids and large volumes of intravenous saline solution with dextrose, a type of sugar. This treatment usually brings rapid improvement. When the patient can take fluids and medications by mouth, the amount of glucocorticoids is decreased until a maintenance dose is reached. If aldosterone is deficient, maintenance therapy also includes oral doses of fludrocortisone acetate.
What special problems can occur with adrenal insufficiency?
Because cortisol is a "stress hormone," people with chronic adrenal insufficiency who need any type of surgery requiring general anesthesia must be treated with intravenous glucocorticoids and saline. Intravenous treatment begins before surgery and continues until the patient is fully awake after surgery and able to take medication by mouth. The "stress" dosage is adjusted as the patient recovers until the presurgery maintenance dose is reached.
In addition, people who are not currently taking glucocorticoids but who have taken long-term glucocorticoids in the past year should tell their doctor before surgery. These people may have sufficient ACTH for normal events, but they may need intravenous treatment for the stress of surgery.
During illness, oral dosing of glucocorticoid may be adjusted to mimic the normal response of the adrenal glands to this stress on the body. Significant fever or injury may require triple oral dosing. Once recovery from the stress event is achieved, dosing is then returned to maintenance levels. People with adrenal insufficiency should know how to increase medication during such periods of stress. Immediate medical attention is needed if severe infections, vomiting, or diarrhea occur. These conditions can precipitate an Addisonian crisis.
Pregnancy
Women with adrenal insufficiency who become pregnant are treated with standard replacement therapy. If nausea and vomiting in early pregnancy interfere with taking medication by mouth, injections of the hormone may be necessary. During delivery, treatment is similar to that of people needing surgery. Following delivery, the dose is gradually tapered and the usual maintenance doses of oral hydrocortisone and fludrocortisone acetate are reached about 10 days after childbirth.
How can someone with adrenal insufficiency prepare for an emergency?
People with adrenal insufficiency should always carry identification stating their condition in case of an emergency. A card or medical alert tag should notify emergency health care providers of the need to inject cortisol if the person is found severely injured or unable to answer questions. The card or tag should also include the name and telephone number of the person's doctor and the name and telephone number of a family member to be notified. The dose of hydrocortisone needed may vary with a person's age or size. For example, a child younger than 2 years of age can receive 25 milligrams (mg), a child between 2 and 8 years of age can receive 50 mg, and a child older than 8 years should receive the adult dose of 100 mg. When traveling, people with adrenal insufficiency should carry a needle, syringe, and an injectable form of cortisol for emergencies.
Points to Remember
• Adrenal insufficiency is a disorder that occurs when the adrenal glands do not
produce enough of certain hormones.
• Primary adrenal insufficiency, also called Addison's disease, occurs when the
adrenal glands are damaged and cannot produce enough of the hormone cortisol and often the hormone aldosterone.
• Secondary adrenal insufficiency occurs when the pituitary gland fails to produce
enough adrenocorticotropin (ACTH), a hormone that stimulates the adrenals to produce cortisol. If ACTH output is too low, cortisol production drops.
• The most common symptoms of adrenal insufficiency are chronic, worsening
fatigue; muscle weakness; loss of appetite; and weight loss.
• Adrenal insufficiency is most often diagnosed through blood or urine tests.
Imaging studies such as x rays, ultrasound, computerized tomography (CT), and magnetic resonance imaging (MRI) may also be used.
• Treatment of adrenal insufficiency involves replacing, or substituting, the
hormones that the adrenal glands are not making.
• People with adrenal insufficiency should always carry identification stating their
condition in case of an emergency.
Hope through Research
Researchers are evaluating the use of another adrenal hormone, dehydroepiandrosterone, in improving the health-related quality of life in people with adrenal insufficiency. Scientists are also studying the occurrence of "relative" adrenal insufficiency—below normal production of adrenal hormones during critical illness—to further define this type of adrenal insufficiency, develop diagnostic tests, and identify the best treatment options.
Participants in clinical trials can play a more active role in their own health care, gain access to new research treatments before they are widely available, and help others by contributing to medical research. For information about current studies, visit www.ClinicalTrials.gov.
For More Information
The following articles about Addison's disease can be found in medical libraries, some college and university libraries, and through interlibrary loan in most public libraries.
Chrousos GP. Glucocorticoid therapy. In: Felig P, Frohman L, eds. Endocrinology and Metabolism. 4th ed. New York: McGraw-Hill; 2001:609–632.
Munver R, Volfson IA. Adrenal insufficiency: diagnosis and management. Current Urology Reports. 2006;7:80–85.
Nieman LK, Chanco Turner ML. Addison's disease. Clinics in Dermatology. 2006;24(4):276–280.
Stewart PM. The adrenal cortex. In: Larsen P, ed. Williams Textbook of Endocrinology. 10th ed. Philadelphia: Saunders; 2003:491–551.
Ten S, New M, Maclaren N. Clinical Review 130: Addison's disease 2001. Journal of Clinical Endocrinology & Metabolism.2001;86(7):2909–2922.
Williams GH, Dluhy RC. Disorders of the adrenal cortex. In: Braunwald E, ed. Harrison's Principles of Internal Medicine. 17th ed. New York: McGraw-Hill Professional; 2008:2247–2268.
Publications produced by the NIDDK are carefully reviewed by both NIDDK scientists and outside experts. This publication was reviewed by Karen Loechner, M.D., Ph.D., University of North Carolina at Chapel Hill.
This publication may contain information about medications. When prepared, this publication included the most current information available. For updates or for questions about any medications, contact the U.S. Food and Drug Administration toll-free at 1–
888–INFO–FDA (1–888–463–6332) or visit www.fda.gov. Consult your doctor for more information.
National Endocrine and Metabolic Diseases Information Service
6 Information Way Bethesda, MD 20892–3569 Phone: 1–888–828–0904 TTY: 1–866–569–1162 Fax: 703–738–4929 Email: [email protected] Internet: www.endocrine.niddk.nih.gov
The National Endocrine and Metabolic Diseases Information Service is an information dissemination service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The NIDDK is part of the National Institutes of Health, which is part of the U.S. Department of Health and Human Services.
The NIDDK conducts and supports biomedical research. As a public service, the NIDDK has established information services to increase knowledge and understanding about health and disease among patients, health professionals and the public.
This publication is not copyrighted. The NIDDK encourages users of this publication to duplicate and distribute as many copies as desired.
NIH Publication No. 09–3054 May 2009
Source: http://www.barronmdfl.com/medicalinfoendocrinology/Adrenal%20Insufficiency%20and%20Addison.pdf
Msif 06 pp1-28 • english
MS in Focus Issue One • 2003 Issue One • 2002 MS in focus Issue 6 • 2005 Intimacy and Sexuality The Magazine of the Multiple Sclerosis International Federation MS in focus Issue 6 • 2005 Executive Editor Nancy Holland, EdD, RN, MSCN, Vice Multiple Sclerosis
Die wahrscheinlichkeit, dass katzen mit husten an einer atemwegserkrankung leiden, ist bei weitem größer als die wahrscheinlic
Wenn die Mieze hustet Ein Überblick über feline Atemwegserkrankungen Husten bei einer Katze sollte man nicht auf die leichte Schulter nehmen. Katzen erkälten sich nicht so leicht wie wir Menschen, Husten gehört bei ihnen nicht zum „Alltäglichen". Daher sollte eine Katze, die wiederholt hustet (ohne dabei etwas hervorzuwürgen, z. B. Haarballen) dem Tierarzt vorgestellt werden.Erste Asthma-Anzeichen zeigen sich oft im Alter von 1 – 3 Jahren, können aber auch früher oder später auftreten. Bei manchen Katzen tritt parallel Niesen und / oder Augenausfluss auf.Wenn eine Katze schwere Atemnot hat (mit geöffnetem Maul und sichtlicher Anstrengung atmet, dabei die Ellbogen evtl. etwas nach aussen dreht), muss sie unverzüglich in tierärztliche Behandlung – dieser Zustand ist lebensbedrohlich! Auch wenn es mitten in der Nacht geschehen sollte – warten Sie lieber nicht bis zum Morgen, sondern rufen Sie den tierärztlichen Notdienst oder bringen Sie Ihre Katze ins nächste Tierspital.