Asnweb.org
Skew Deviation
Gennadiy Shevchenko, MD and Robert A Taylor, MD
Department of Neurology, University of Minnesota
A 31-year-old female presented to emergency department (ED) with acute onset of double vision, vertigo, balance difficulty, nausea, and emesis of one-day duration. Her symptoms were better with closed eyes, and diplopia was worse on left gaze with images one above the other. Her past medical history was significant for cerebellar astrocytoma at the age of 4 (which was treated with resection and location radiation therapy), seizure disorder, and ventriculoperitoneal shunt placement for treatment of hydrocephalus. She also had known hypertension. Her home medications included oxcarbazepine, verapamil, and oral contraceptive pills (OCP).
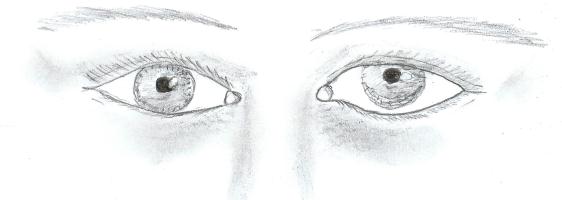
On physical exam, her initial blood pressure was 201/118. Her cardiac exam was normal. The National Institute of Health Stroke Scale (NIHSS) score was zero, however, her neurological examination showed left hypertropia (figure 1), primary gaze diplopia, worse on left gaze with images displaced in vertical plane, horizontal left beat nystagmus on primary gaze, worse on left gaze and better on right gaze.
Figure 1: Left hypertropia
In the ED, the initial differential diagnosis included stroke, multiple sclerosis, and tumor recurrence. Head computed tomography (CT) scan showed no hemorrhage. CT angiogram showed a short segment narrowing of the second part of the left posterior cerebral artery.
Patient was admitted to the hospital. Laboratory tests included hemoglobin A1C of 5.2%, LDL 94 mg/dL, and hypercoagulable workup (which was negative except for elevated anticardiolipin IgG antibody 109 units). Transthoracic echocardiogram showed mild atherosclerotic disease (one non-mobile plaque) in proximal portion of transverse aortic arch, but was negative for wall motion abnormality, patent foramen ovale, or thrombus. MRI showed a small area of diffusion restriction in the right pontomedullary junction in the vicinity of the vestibular nuclei (figure 2). MRA showed normal vessels.
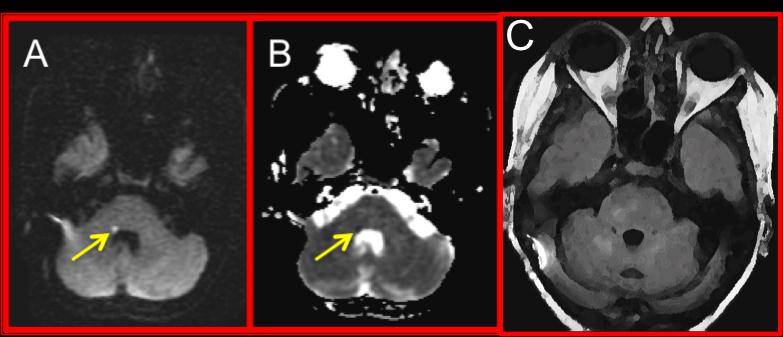
Figure 2: Small area of diffusion restriction (A) with hypointensity on
apparent diffusion coefficient map (B) within a larger area of T2
hyperintensity (C) seen on FLAIR.
Based on this workup, the primary stroke mechanism was felt to be post-radiation small vessel vasculopathy, possibly with some contribution of hypertension. OCP use and elevated anticardiolipin IgG were felt less likely a cause of the stroke. The patient was treated with aspirin and risk factor modification (including tighter blood pressure control). Her symptoms improved with symptomatic treatment. She was discharged to an acute rehabilitation facility.
Discussion
Skew deviation is vertical misalignment in which the eyes move in
opposite directions equally, an acquired hypertropia secondary to sensory
imbalance of graviceptive pathways that run from utricle and semicircular
canals to supranuclear centers (interstitial nucleus of Cajal [INC] and the
rostral interstitial nucleus of the medial longitudinal fasciculus [riMLF])
crossing at the pontine level. By convention, higher eye and term
hypertropia are always used as a reference regardless of affected side:
such as on denoted above face picture left eye is higher, thus – left
hypertropia, not right hypotropia. Skew deviation may be associated with
head tilt and ocular torsion, together representing an ocular tilt reaction
(OTR).
ETIOLOGY: injury within the posterior fossa
Common: stroke, multiple sclerosis, tumor, trauma, abscess,
syringobulbia, neurosurgical procedures.
Rare: increased intracranial pressure, Arnold-Chiari malformation,
platybasia, paroxysmal epileptic skew deviation, Creutzfelt-Jakob disease,
multifocal
encephalomyelitis
LOCALIZING VALUE: unilateral peripheral or pontomedullary lesions
induce ipsiversive skew deviations (toward the side of the lower eye), while
unilateral pontomesencephalic and mesodiencephalic lesions cause
contraversive (contralateral eye undermost) skew deviations. Mnemonic:
high-high, low-low helps memorizing in a way that if insult is lower in the
brain prior to the crossing of the pathways, lower eye will be on the same
side as lesion, but if it occurs higher in the brain after crossing of the
pathways, then higher eye will be on the same side as lesion.
On the other hand, it also helps to lateralize the lesion if level is known from other clinical signs – for example, patient with known lesion level at mesodiencephalic region and left hypertropia has left sided insult, whereas patient with known pontine lesion and left hypertropia has right sided injury.
Next, unilateral posterior thalamic lesions can induce ipsiversive or contraversive skew deviations in addition to thalamic astasia, thus hindering its use in localization.
Finally, unilateral lesions of vestibular cortex (parieto-insular regions) cause mostly contraversive skew deviation.
TREATMENT AND PROGNOSIS:
- spontaneous recovery in several weeks to months.
- eye patch and prism correction may be used for symptomatic relief of vertical diplopia.
- prisms, botulinum toxin, and surgical correction (vertical rectus muscle recession) are usually effective in persistent cases.
Teaching points
NIHSS can be low or even 0 despite a stroke causing significant deficit.
By convention, higher eye and term hypertropia are always used to describe vertical misalignment regardless of affected side
Skew deviation can aid localizing and lateralizing unilateral lesion:
mnemonic "high-high, low-low" helps memorizing in a way that if
insult is lower in the brain prior to the crossing of the pathways, lower
eye will be on the same side as lesion, but if it occurs higher in the
brain after crossing of the pathways, then higher eye will be on the
same side as lesion. It also helps to lateralize the lesion if level is
known from other clinical signs.
Most of the skew deviations recover spontaneously within several weeks to months, but eye patch and prism correction may be used for symptomatic relief in acute period.
References
1. Brodsky MC, Donahue SP, Vaphiades M, at al: Skew Deviation Revisited. Surv Ophthalmol 51 (2): 105-28, 2006 DOI: 10.1016/j.survophthal.2005.12.008
2. Zwergal A, Cnyrim C, Arbusow V, at al: Unilateral INO is associated with ocular tilt reaction in pontomesencephalic lesions: INO plus. Neurology, 71(8): 590-3, 2008
3. Lui G: Neuro-Ophthalmology: Diagnosis and Management. 1st edition, Saunders Company, 524-8, 2001
4. Brazilis P, Masdeu J, Biller J: Localization in Clinical Neurology, 5th Edition, Lippincott Williams & Wlikins, 231-3, 2007
5. Teaching point "high-high, low-low" credited to Steven Galetta MD,
Department of Neurology, NYU.
Corresponding Author
Gennadiy Shevchenko, MD
Department of Neurology, University of Minnesota
420 Delaware St. SE, MMC 295
Minneapolis, MN 55455
Tel: 612-626-6519
Fax 612-625-7950
Source: http://www.asnweb.org/files/Residents%20and%20Fellows%20Section/Case%20Reports/8_28_12%20Skew%20deviation%20Final.pdf
polyfinances.ca
Fonds d'investissement étudiant de Polytechnique Montréal Note Sectorielle Semaine du 28 Janvier 2013 Cette note sectorielle a été réalisée par l'ensemble des étudiants de PolyFinances, le fonds d'investissement étudiant de Polytechnique Montréal. Elle a pour but de vous présenter l'actualité économique, industrielle et de la recherche dans les secteurs associés aux génies enseignés à Polytechnique Montréal.
Finaledp
EVALUACIÓN CONJUNTA DE LA DECLARACIÓN DE PARÍS, FASE 2 COLOMBIA 31 de diciembre de 2010 Centro de Pensamiento Estratégico Internacional – Cepei- Grupo Coordinador Philipp Schönrock Coordinador General e-mail: [email protected] Juan Fernando Buchelli Coordinador Académico e-mail: [email protected] Asistente de Investigación